Executive Briefing: Pricing Is Not an Art, It’s an IP-Driven War
Let’s be blunt. Setting the launch price for a new medicine is arguably the most critical, high-stakes, and durable decision a pharmaceutical company will ever make. It is not a last-minute marketing calculation. It is the culmination of a multi-decade strategic process, a high-stakes war of competitive intelligence, clinical positioning, regulatory navigation, and, most importantly, intellectual property law.
For you—the professionals in pharmaceutical intellectual property, R&D, and business development; the law firms that counsel them; the consultants who model for them; and the investors who bet on them—this process is your entire world. You are, quite rightly, skeptical of hype and demand hard data. You know that the “price of a miracle” isn’t a number pulled from thin air. It is a complex, strategic calculation designed to balance two fundamentally opposing forces: the societal demand for accessible, life-saving medications and the commercial imperative to generate a return on the monumental, high-risk investments that define biopharmaceutical innovation.1
This tension is the entire game. And for too long, public discussions about pricing have missed the single most important variable in the entire equation.
Most reports will tell you that patents grant a “government-sponsored monopoly”.1 This is true, but it’s a first-level understanding. It frames the patent as a simple on/off switch: for 20 years, you have a monopoly; on day 7,301, you fall off a cliff. This is dangerously simplistic.
The central argument of this report is that the patent itself is not the key. The data within the patent portfolio is. The specific, granular details—the “composition of matter” claim versus a weaker “method of use” claim, the exact adjusted expiration date, the thicket of secondary patents, the list of pending generic challenges—are not legal footnotes. They are the primary variables in your pricing model. The Loss of Exclusivity (LOE) date, that ultimate anchor, doesn’t just predict the end of your revenue; it dictates the height and shape of your launch price from Day One.
A patent portfolio isn’t a wall; it’s a measure of confidence. And that confidence—or lack thereof—is what allows a company to set a $100,000-a-year price tag and defend it, or what forces them into a discount just to grab market share. This report will provide an exhaustive guide to this process. We will deconstruct the unique economics of the pharma market, debunk the myths, and build, from the ground up, a modern framework for pricing. We will connect the dots from the R&D lab, to the patent attorney’s desk, to the HTA reviewer’s spreadsheet, to the PBM’s negotiating table.
This is not a guide to the “art” of pricing. This is a blueprint for the IP-driven war.
The Unique Architecture of Pharma Pricing: Why Normal Economics Don’t Apply
Before you can set a price, you must understand the bizarre economic arena in which you’re operating. In no other industry is the “customer” (the patient) not the “payer” (the insurer).1 In no other industry is demand for a life-saving product so profoundly inelastic. And in no other industry is the central justification for price so hotly debated.
The R&D Imperative: Deconstructing the $2.8 Billion Justification
The pharmaceutical industry’s core narrative, its central justification for the high prices of innovative medicines, is the immense cost, risk, and time required for research and development. And the numbers are, indeed, staggering.
The process of bringing a single new drug to market is a gauntlet of failure. It begins with screening 5,000 to 10,000 chemical compounds to find a handful of promising candidates.2 It then enters rigorous, multi-phase clinical trials. Phase I tests for safety. Phase II tests for efficacy. Phase III confirms effectiveness and compares it to existing treatments.2 This process can take 10 to 15 years.3
The failure rate is astronomical. Fully 90% of clinical drug development programs fail.4 Only 12% of drugs that enter Phase I trials will ultimately gain FDA approval.2 Because of this, the capitalized cost of a single approved drug—factoring in the cost of all the failures that preceded it—is estimated to be anywhere from $879 million to a staggering $2.8 billion.1 Some estimates go as high as $4.5 billion.3
This is the “R&D imperative.” The industry’s argument is that high launch prices, protected by a temporary patent monopoly, are the only mechanism that provides a sufficient incentive for investors to pour billions into such a high-risk, low-probability-of-success venture.3 This logic, they argue, is the “lifeblood of innovation”.5
The Counter-Argument: Is R&D a Justification or a Narrative?
If you’re an R&D leader, a BD executive, or a pricing strategist, you know that while the macro R&D argument is true, it’s not actually how a specific drug’s price is set. No pricing committee sits down, calculates the sunk R&D cost for that specific asset, and adds a 30% margin. That is not the formula.
The reality, as you know, is that the launch price is determined by “what the market will bear”.1 This is a calculation based on the drug’s perceived clinical value, the severity of the unmet medical need, and the competitive landscape.1 The R&D cost is a sunk cost; it is not a direct input into the pricing equation.
Skeptics and researchers have proven this with data. A 2020 JAMA study, for instance, found “no association” between estimated R&D investments and treatment costs, either at the list price at launch or the net price a year later.6 Another study from UC San Diego came to the same conclusion, finding no link between R&D costs and drug prices.7
The most damning data point, and the one most frequently used by critics, relates to corporate spending priorities.
A 2020 analysis published in The BMJ found that from 1999 to 2018, the world’s 15 largest biopharmaceutical companies spent significantly more on selling, general, and administrative (SG&A) activities—which includes marketing—than on research and development. The figures were staggering: $2.2 trillion on SG&A versus $1.4 trillion on R&D. 6
Further analysis of large pharma companies from 2009-2018 found that shareholder payouts (dividends and stock buybacks) accounted for 29% of global revenue, while R&D accounted for only 17%.5
So, what are we to make of this? Is the R&D justification a lie?
No. It’s a misunderstanding of its purpose. The R&D cost argument is not a pricing formula. It is a political and regulatory narrative. It is the industry’s public-facing argument to policymakers (like Congress) to justify the existence and duration of the patent-granted monopoly system. It’s an argument about policy, not price.
As pricing and IP professionals, we can acknowledge this nuance. We can set aside the public debate and focus on the true economic drivers that actually enable premium pricing.
The Real Drivers: Inelastic Demand and the Third-Party Payer Distortion
If sunk R&D costs don’t set the price, what does? The unique, distorted architecture of the pharmaceutical market, which is built on two pillars that shatter normal economic principles:
- Profound Inelasticity of Demand: In a normal market, if the price of a product (like a car or a television) goes up, demand for it goes down. Consumers “shop around” or choose an alternative. This does not happen with essential medicines. A patient with metastatic cancer, multiple sclerosis, or a rare genetic disorder does not “shop around” for a cheaper treatment. For life-saving or life-altering therapies, demand is profoundly inelastic. The “consumer” will pay (or, more accurately, have their insurer pay) almost any price.1
- The Third-Party Payer Distortion: This is the most significant distortion. In 99% of transactions, the consumer of the drug (the patient) is not the payer of the drug. The bill is paid by a third party: a private insurer, a Pharmacy Benefit Manager (PBM), or a government (Medicare/Medicaid). This system effectively insulates the patient from the full cost at the point of care, shattering the normal price-sensitivity that governs free markets.1
These two factors—inelastic demand and the third-party payer system—create a market where price is “whatever the payer can be convinced to bear.” And what convinces a payer to bear a high price? Clinical value, yes. But even more fundamentally: a government-granted monopoly, rooted in the patent.
The Patent Is the Price: How IP Data Forms the Bedrock of Launch Strategy
This is the central thesis that bridges the gap between the legal department and the commercial team. The launch price is not just a number; it is an equation. And the most important variables in that equation are drawn directly from your patent portfolio.
Your Price Is Your Patent’s Expiration Date
The single most important number in any pharmaceutical revenue model is the Loss of Exclusivity (LOE) date. This is the date when your key patents expire, and generic or biosimilar competitors can flood the market. It is the “patent cliff”.9
Every financial model, every investment thesis, every pricing strategy is, at its core, a countdown to this date. Why? Because the data is unanimous on what happens after this date.
- Studies show that after patent expiry, drug prices decrease significantly, with reductions ranging from 30% to 80% depending on the country and product.10
- One study tracking drugs over their lifecycle found a median price decrease of 41% within four years after patent expiration.12
- This cliff is immediate and severe. The innovator’s brand faces a “dramatic shift” and must “relinquish monopoly” to multiple, low-cost generic alternatives.9
This is why the LOE date is the anchor for your launch price. Your entire pricing strategy is an attempt to maximize the area under the revenue curve before you hit that cliff. A drug with 15 years of protected, exclusive life is a fundamentally different asset—and commands a fundamentally different launch price—than a drug with only 5 years left.13 Your pricing power is a direct function of your remaining patent life.
The “Patent Thicket” vs. The “Composition of Matter” Moat
Here’s the next level of sophistication: not all patent protection is created equal. A savvy BD or pricing team knows that the type and quality of the patents in their portfolio are a direct measure of their pricing confidence.
There are two basic forms of patent protection: the “moat” and the “thicket.”
- The “Moat”: Composition of Matter Patents
This is the gold standard.14 A “composition of matter” (CoM) patent covers the active pharmaceutical ingredient (API) itself—the core molecule. This is the strongest, widest, and most defensible “moat” you can have. It provides the highest degree of market exclusivity and, therefore, the highest confidence for a premium, value-based launch price. It gives you a clear, legally-defended monopoly.14 - The “Thicket”: Secondary and Defensive Patents
A “patent thicket” is a defensive strategy. It’s a dense, overlapping web of dozens or even hundreds of secondary patents filed after the core CoM patent.16 These weaker patents don’t cover the molecule itself, but everything around it 17:
- Formulation Patents: (e.g., an extended-release version) 15
- Method of Use Patents: (e.g., using the drug for a new disease) 15
- Delivery Device Patents: (e.g., a specific auto-injector pen)
The most famous example is AbbVie’s Humira, which was protected by a “thicket” of over 100 patents, delaying biosimilar entry for years after its initial CoM patent expired.18
A pricing team with a strong CoM “moat” can be patient, confident, and focus on building value. A pricing team whose drug is only protected by a “thicket” is in a different position. They are in a constant legal-commercial battle. Their pricing must reflect the high risk that a generic competitor will successfully challenge one of these weaker patents and enter the market early.
The Critical Difference: Patent vs. Regulatory Exclusivity
This is one of the most vital and frequently misunderstood concepts in pharmaceutical strategy. Your market monopoly is not protected by one clock; it is protected by two separate and independent clocks.16
- Patents (from the USPTO): This is the intellectual property right granted by the U.S. Patent and Trademark Office (PTO) for an invention.16 As we’ve discussed, this can be the molecule, the formulation, or the method of use. The term is generally 20 years from the filing date, which is often many years before the drug is ever approved.16
- Regulatory Exclusivity (from the FDA): This is a totally separate protection granted by the Food and Drug Administration (FDA) upon the drug’s approval.16 This is not a patent. This is a data exclusivity period. It prohibits the FDA from approving a generic or biosimilar application that relies on the innovator’s clinical trial data for a set period, regardless of the patent status.16
These two clocks run concurrently, and your true monopoly ends on whatever date is later.
The key FDA exclusivities you must track are 22:
- New Chemical Entity (NCE) Exclusivity: 5 years from approval for a new, novel molecule.
- Orphan Drug Exclusivity (ODE): 7 years from approval for a drug that treats a rare disease (affecting <200,000 people in the US).
- “Other” Exclusivity (New Clinical Investigation): 3 years for a “change” to an approved drug (like a new indication or formulation) if new clinical trials were required.
- Pediatric Exclusivity (PED): This is a 6-month “kicker” that the FDA grants as a reward for conducting pediatric studies. This 6 months is added to any existing patents and exclusivity periods.22
A pricing strategist must model both timelines. A drug might have a patent that expires in 8 years, but if it has Orphan Drug status, it’s protected by FDA exclusivity for 7 years. Conversely, its 5-year NCE exclusivity might run out, but its core “composition of matter” patent could protect it for another 12 years. The real LOE date is the one that comes last.
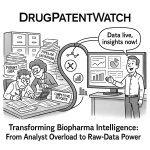
Using Patent Intelligence Tools for Pricing Models
So, how does a BD or pricing team actually get and use this data? You’re not going to manually read USPTO filings. This is where competitive intelligence platforms become non-negotiable.
Platforms like DrugPatentWatch are designed for this exact purpose: to translate complex legal and patent data into actionable, commercial and strategic intelligence.18
This is the “how-to” for a pricing or BD team. You use these tools to feed the critical, time-based variables into your revenue and pricing models.18 Specifically, you track:
- Verified Patent Expiry Dates: The system calculates the real expiration dates, factoring in Patent Term Adjustments (PTA) from the USPTO and any extensions.18
- Market Exclusivity Status: It tracks the separate FDA exclusivity clock (NCE, ODE, PED) so you can model both timelines.18
- Paragraph IV (PIV) Challenges: This is perhaps the most critical live data. A PIV filing is a public notification that a generic company is challenging your patent(s), claiming they are invalid or that their product does not infringe.13 This is the “check engine” light for your revenue stream. Tracking PIV filings, and their subsequent litigation outcomes, is the only way to predict if your patent cliff is going to arrive years earlier than expected.
- Authorized Generics & First Entrants: The platform helps identify who the first generic entrants are likely to be, allowing you to prepare a counter-strategy.18
This data is the bedrock of the pricing model. It allows you to “set reasonable launch prices” by defining the duration of your monopoly.18 It allows you to “plan product lifecycles” and “predict market-shaking events” like a PIV settlement.13 The quality of your patent portfolio—how many PIV challenges it attracts, how strong its “moat” is—becomes the risk variable in your financial model. A weak, heavily-challenged patent portfolio means your pricing model must be more aggressive, or your launch price lower, to account for the high risk of premature generic entry.
The Modern Pricing Toolkit: A Deconstruction of Core Models
Once you have established your IP-protected timeline, you must choose a pricing strategy. This is the “missing Section 3” from the original analysis 1—the actual models that commercial teams use to justify a price to payers. The final list price is rarely the result of one model; it’s a sophisticated blend, where one model provides the public justification (VBP) and another sets the market boundaries (Competitor-Based).
Value-Based Pricing (VBP): The Dominant Paradigm for Innovation
Value-Based Pricing (VBP) is the predominant framework used to justify the high cost of truly novel, innovative medicines.25
- Core Mechanic: The price is not based on the cost of R&D or manufacturing. Instead, the price is linked directly to the value the medicine delivers to patients, providers, and the healthcare system as a whole.25
- How is “Value” Defined? It’s a function of multiple factors:
- Superior efficacy (e.g., extends life, cures disease)
- Improved safety profile (fewer side effects)
- Better quality of life (QoL)
- Cost-offsets (e.g., reduces expensive hospitalizations or surgeries) 25
- Strategic Application: This is the only model that justifies a premium, high-cost launch. It is used exclusively for innovative, first-in-class, or highly differentiated drugs that can prove they are a significant advancement over the old standard of care.25 The industry champions this approach as the mechanism that rewards and encourages true innovation.25
Competitor-Based Pricing: The “First-in-Class” vs. “Me-Too” Gamble
This is the most straightforward model: you simply benchmark your price against existing therapies in the same class.25 However, your strategy within this model depends entirely on your clinical data.
- Premium Pricing: If your drug is “first-in-class” or, more importantly, if you have clinical trial data demonstrating superiority to the competition, you will use “premium pricing.” You set your price above competitors to signal its superior value.1
- Parity or Discount Pricing: If your drug is a “me-too” product—meaning it offers similar efficacy and safety to established treatments—you have no justification for a premium. You will use “parity pricing” (matching the competitor’s price) or “discount pricing” (pricing just below it) to encourage uptake and steal market share.1
The Clinical Data Lynchpin: Superiority vs. Non-Inferiority
This is one of the most critical, cross-functional concepts for R&D and BD teams to understand. The most important pricing decision you make is often locked in years before launch, not by the commercial team, but by the clinical team when they design the Phase III trial.
There are two fundamental trial designs when testing against an existing standard of care:
- Superiority Trial: This trial is designed to prove that your new drug is statistically better than the current standard of care.26 This is a high-risk, high-cost, and time-consuming trial. You might fail. But if you succeed, you have just generated the golden ticket for pricing. You have the hard evidence required to go to payers and demand a premium, value-based price.
- Non-Inferiority Trial: This trial is designed only to prove that your new drug is no worse than (i.e., “non-inferior” to) the current standard of care.26 These trials are often cheaper, faster, and have a higher probability of success.28
Here is the strategic trap: The moment your R&D team commits to a “non-inferiority” trial design, they have already forfeited your ability to argue for a premium price. You have made a business decision to not even try to prove you are better. When you go to payers, they will look at your “non-inferior” data and say, “Congratulations. You’ve proven your drug is ‘just as good’ as the one we already pay for. We will not pay a penny more for it.”
You have locked yourself into a “me-too,” competitor-based, parity-pricing strategy.27 This decision, made in R&D, has a multi-billion dollar consequence for the commercial launch.
Niche Models: Cost-Plus, Indication-Specific, and the Rise of “Pay-for-Performance”
While VBP and competitor-based pricing dominate, a few other models exist for specific situations.
- Cost-Plus Pricing: Simply the cost of goods sold (COGS) plus a fixed percentage markup.25 This model is never used for innovative, patented drugs. It is the domain of the generics market.25
- Indication-Specific Pricing: A more complex, high-level strategy where the same drug has different net prices for different indications. For example, a drug might command a high price for a high-value oncology indication but a lower net price for a less severe autoimmune condition.
- Outcomes-Based Agreements (OBAs): This is the new frontier, designed for the “sticker shock” of ultra-high-cost cell and gene therapies. Also known as “pay-for-performance,” this model directly addresses payer uncertainty about long-term value.29 Instead of just a one-time high price, the manufacturer is paid based on actual patient outcomes.32 If the drug works as promised, the manufacturer gets the full price. If it fails, they must pay a significant rebate. We will explore this in detail in our case studies.
The Value Gauntlet: Navigating the HTA Maze (ICER, NICE, & IQWiG)
So, you’ve chosen a Value-Based Pricing strategy. You’ve declared your drug has “value.”
Now you have to prove it.
This is the “Value Gauntlet,” a complex and varied global network of Health Technology Assessment (HTA) bodies. These are the gatekeepers—often government-run—who analyze your clinical and economic data to decide if your drug provides “value for money.” A negative HTA recommendation can kill your market access.
The QALY and the ICER: The Math Behind “Value”
To navigate the HTA maze, you must first speak their language. And in most of the world (with one major exception), that language is mathematics.
- The QALY (Quality-Adjusted Life Year): This is the universal metric for measuring health benefit. It combines both quantity of life (mortality) and quality of life (morbidity, side effects) into a single number. One QALY is equal to one year of life in perfect health.34
- The ICER (Incremental Cost-Effectiveness Ratio): This is the core formula HTA bodies use. It is not a drug’s price tag. It is a ratio that compares your new, more-expensive drug to the old, cheaper standard of care.35
The formula is:
$$ICER = \frac{(Cost_{New Drug} – Cost_{Old Standard of Care})}{(QALYs_{Gained from New Drug} – QALYs_{Gained from Old Standard of Care})}$$
The result is a number expressed as “cost per QALY gained.”
This ICER number is then compared to a willingness-to-pay (WTP) threshold. This is the “value” a country’s health system places on a single year of perfect health.
- In the United Kingdom, the National Institute for Health and Care Excellence (NICE) historically uses a threshold of £20,000 to £30,000 per QALY.36
- In the United States, the de facto threshold used by the Institute for Clinical and Economic Review (ICER) is typically between $50,000 and $200,000 per QALY.37
If your drug’s ICER is below this threshold, it’s deemed “cost-effective” and recommended for reimbursement. If it’s above it, it’s rejected as “not providing value for money,” and you will be forced to offer a steep discount to get it covered.
The Gatekeepers: Comparing HTA Methodologies (NICE vs. IQWiG)
A global launch strategy is complex because every major market runs its HTA gauntlet differently. Your evidence dossier for the UK will be useless in Germany. A pricing and R&D team must understand this difference.
- NICE (United Kingdom): The Economic Model
NICE is the classic, QALY-based economic evaluator. Their recommendations are legally binding in England and Wales.38 Their entire system is built on integrating clinical benefit and cost-effectiveness.38 Their recommendations “heavily rely” on that ICER (cost-per-QALY) calculation as the primary indicator of “value for money”.38 - What You Need to Win: A robust health-economic model proving your ICER is below their WTP threshold.
- IQWiG (Germany): The Clinical Model
Germany is the great exception. The German HTA system, run by IQWiG and the G-BA (Federal Joint Committee), explicitly rejects the cost-per-QALY metric as a measure of value.38
- What You Need to Win: Their “Early Benefit Assessment” (EBA) is not an economic evaluation. It is a comparative clinical evaluation.38 The G-BA asks only one question: “Does this new drug provide an added clinical benefit over the current, established standard of care?” This benefit must be proven with head-to-head data on “patient-relevant end points” like survival or morbidity.38 In the German assessment, economic evaluation “has not yet played any real role”.38
- The Strategic Impact: This is a crucial divergence. A pharma company needs two completely different value dossiers for its European launch:
- For NICE: A health-economic dossier full of QALY models.
- For IQWiG: A clinical dossier full of head-to-head superiority data.
ICER (US): The “Shadow” Gatekeeper
The United States has a unique, market-driven model with no formal, government-run HTA body that can set prices for the entire country (at least, not until the IRA).
Into this vacuum has stepped the Institute for Clinical and Economic Review (ICER). ICER is an independent, non-profit watchdog that has become the de facto “shadow” HTA for the US market.37
ICER produces highly influential, public reports that assess the value of new, high-cost drugs. They use a QALY-based, ICER-driven model, similar to NICE, with their own “value-based price benchmarks” based on WTP thresholds of $50,000 to $200,000 per QALY.37
While ICER has no legal power, its reports are a weapon for payers. PBMs and insurers love ICER reports. They use them as objective, third-party ammunition to go into rebate negotiations and justify to manufacturers why they will not cover a new drug at its high launch price. As we will see in the Aduhelm case study, a negative ICER report can be a commercial death sentence.41
Table 1: HTA Methodology at a Glance: ICER vs. NICE vs. IQWiG
| Feature | ICER (United States) | NICE (United Kingdom) | IQWiG / G-BA (Germany) |
| Official Role | Independent “watchdog” / “Shadow” HTA. No legal power, but high payer influence.37 | Government-affiliated body. Recommendations are legally binding.38 | Independent institute (IQWiG) and statutory body (G-BA). Assessment is binding for price negotiation.38 |
| Primary Methodology | Economic Evaluation (Cost-Effectiveness). | Economic Evaluation (Cost-Effectiveness). | Clinical Evaluation (Comparative Benefit). |
| Use of QALY? | Yes. Central to the model.37 | Yes. The primary metric for value.38 | No. Explicitly rejects the QALY metric.38 |
| Stated Threshold | $50,000 – $200,000 per QALY.37 | ~£20,000 – £30,000 per QALY (can be higher for EoL).36 | None. Assessment is based only on the level of added clinical benefit (e.g., Major, Considerable, Minor).38 |
| Impact on Price | Used by PBMs/payers as ammunition in confidential rebate negotiations.41 | Sets the “value” bar. A high ICER forces the manufacturer to offer a confidential discount to meet the threshold. | The level of added benefit sets the negotiating power. “No added benefit” = drug is priced at the generic level. “Major added benefit” = full pricing freedom.43 |
The Payer Wall: Cracking the PBM Formulary and the Gross-to-Net Bubble
You’ve cleared the HTA gauntlet. You have your patent-protected timeline. You have your “value-based” price. Now you enter the “Wild West”: the American payer system.
Here, your carefully calculated value-based price collides with the market power of Pharmacy Benefit Managers (PBMs) and the opaque, perverse incentives of the “Gross-to-Net Bubble.” This is the second major gap in most pricing analyses—understanding that in the US, your “launch price” is not a price at all. It’s an opening bid.
The Gatekeepers: What Are PBMs and How Do They Work?
PBMs are the powerful, and often invisible, “middlemen” in the US drug supply chain.44 Health insurers and large employers hire PBMs to manage their entire prescription drug benefit.45
PBMs derive their power from three main functions:
- Formulary Creation: They create the formulary—the list of drugs the health plan will cover—and decide which tier a drug is on (e.g., Tier 1 Preferred Generic, Tier 3 Non-Preferred Brand), which determines the patient’s copay.45
- Rebate Negotiation: They use the formulary as a weapon. They go to manufacturers and negotiate massive, confidential rebates in exchange for placing a drug on a preferred tier.47
- Pharmacy Networks: They contract with pharmacy chains to create a “network” that patients must use.44
This is a highly concentrated market. The three largest PBMs (CVS Caremark, Cigna’s Express Scripts, and UnitedHealth’s OptumRx) control approximately 80% of all prescription drug claims.44 This concentration gives them immense, non-negotiable leverage over manufacturers.
Deconstructing the “Gross-to-Net Bubble”
This is the single most important concept in understanding US pharmaceutical pricing. In the US, every brand-name drug effectively has two prices 49:
- List Price (or WAC): The “Wholesale Acquisition Cost” is the official, publicly-announced “sticker price” set by the manufacturer.50 This is the price you see in news reports.
- Net Price: This is the actual revenue the manufacturer gets to keep after paying all confidential rebates, discounts, and administrative fees to the PBMs and other payers.50 This price is a closely guarded secret.
The “Gross-to-Net Bubble” is the vast, and rapidly growing, dollar gap between these two numbers.51 In 2023, this bubble—the total value of all rebates and discounts—hit a record $334 billion.51 More than half of that went to rebates and fees paid to PBMs.51 For some drug classes, like insulin, the net price has barely budged while the list price has soared over 300%, with the entire difference being consumed by this “bubble”.52
The Perverse Incentive: Why PBMs Love High List Prices
This is the “dirty secret” of the PBM system. Why would a PBM want a high list price? Why not just demand a low, simple price from the start?
It’s because of the “perverse incentive” in their business model.
PBMs negotiate rebates from manufacturers in exchange for formulary placement.47 Critically, these rebates are almost always calculated as a percentage of the list price (WAC).47
This creates a system that rewards high list prices. Consider this:
- Drug A (Transparent Price): Launches at a simple, low $300 net price with a 0% rebate.
- Drug B (PBM-Friendly Price): Launches at a $1,000 list price but offers a 70% ($700) rebate.
Which drug does the PBM prefer? Drug B.
The $300 net-price drug offers the PBM nothing to work with. They can’t show “savings” to their insurer client, and they have no margin to profit from.
The $1,000 list-price drug, however, gives the PBM a massive $700 rebate to play with. The PBM can pass $600 of that rebate back to the insurer client (proving its “value” in “negotiating” the price down from $1,000 to $400) and keep $100 for itself as an “administrative fee” or profit from “spread pricing”.46
The manufacturer is indifferent; they get $300 in net revenue either way. But the PBM and insurer vastly prefer the high-list/high-rebate model. This systemic incentive inflates list prices across the entire market.47
How the Bubble Hurts Patients
If the insurer is getting a rebate and the manufacturer is getting their target net price, who is harmed?
The patient.
Patient out-of-pocket costs—deductibles and, most importantly, coinsurance—are almost always based on the fake, undiscounted list price.51
Let’s return to our example. A patient has a 20% coinsurance plan.
- If they take Drug A ($300 net price), their coinsurance is 20% of $300, or $60.
- If they take Drug B ($1,000 list price), their coinsurance is 20% of $1,000, or $200.
The patient on the PBM-preferred drug pays over 3x more out-of-pocket, even though the net cost of both drugs to the system is identical. The PBM and insurer still collect the $700 rebate, meaning the insurer’s total cost for the drug is $300 (net price) – $200 (patient share) = $100. The patient’s high coinsurance payment, based on the inflated list price, flows directly to the insurer’s bottom line.
This is the “Money From Sick People” phenomenon.51 It is the direct consequence of the gross-to-net bubble.
For a pricing strategist, this is the takeaway: you cannot simply launch with a low, transparent net price in the US, even if you wanted to. You would get zero formulary access because you offer no “rebate” for the PBMs to profit from. Your “launch price” is just the opening bid in the rebate negotiation, set artificially high to have “room” to negotiate down.
The Global Chessboard: Managing Price Contagion with IRP-Aware Launch Sequencing
Pricing is not a domestic decision. The moment you launch in one country, you have started a global domino effect. A drug’s price in Germany can, and will, directly determine its price in Japan, Canada, and Australia.
What is International Reference Pricing (IRP)?
International Reference Pricing (IRP), also known as External Reference Pricing (ERP), is a price control mechanism used by governments all over the world.56 It is extremely common, used by the vast majority of EU countries (notably, the UK and Sweden are exceptions), as well as major markets like Japan, Canada, and Australia.1
The mechanism is simple:
- A government (e.g., Canada) wants to set the price for your new drug.
- It looks at a “basket” of other, similar countries (e.g., France, Germany, UK, Italy).56
- It finds the price you are charging in those countries and sets its own price at the average (or sometimes, the lowest) of that basket.
This is a rational tool for smaller countries with less negotiating power to ensure they don’t overpay.56
The “Price Contagion” Risk and Strategic Launch Sequencing
For a pharmaceutical company, IRP is the single greatest global pricing risk. It creates a phenomenon called “price contagion”.1
This is the nightmare scenario:
- You launch your innovative drug first in a smaller, lower-income country like Portugal, which has a low willingness-to-pay. They demand, and you grant, a low price of, say, €1,000/month.
- Next, you launch in Germany, a massive, high-value market.
- But Germany’s IRP basket includes Portugal. The German government “references” your €1,000 Portuguese price and uses it to permanently set your German price far below what the market would have actually borne.
- Then, Japan, Canada, and two dozen other countries all reference Germany’s new, low price.
You have just made a multi-billion dollar mistake. That one low price in a small market has “contaminated” your entire global revenue potential.
The only rational business response to this threat is strategic launch sequencing.57
To maximize value and mitigate IRP risk, a global pricing team must follow a careful sequence 57:
- Launch FIRST in high-price, market-driven, or non-IRP “anchor” countries. This almost always means the United States (which has no price controls) and Germany (which, as we saw, prices based on clinical benefit, not QALY-economics).
- Launch SECOND in other major HTA/IRP markets, using the high US/German prices as your positive reference points.
- Launch LAST (or delay launch, sometimes for years) in the smaller, lower-price countries that are most likely to “contaminate” your reference basket.58
This creates a profound ethical and commercial dilemma. The rational, profit-maximizing strategy for a pharmaceutical company, in direct response to IRP, is to intentionally withhold or delay access to innovative medicines from patients in poorer countries to protect their pricing power in richer ones.58
The New Earthquake: How the Inflation Reduction Act (IRA) Rewrote the Pricing Playbook
If IRP was the established order, the Inflation Reduction Act (IRA) of 2022 is the earthquake that just toppled the entire chessboard—at least in the United States, the world’s largest and most profitable market.
For the first time, the IRA gives the U.S. government (specifically, Medicare) the power to do what it was always forbidden from doing: “negotiate” drug prices. For pricing, R&D, and IP teams, the IRA is the single most disruptive piece of legislation in decades, and one of its provisions is already shifting billions in R&D investment.
The Mechanism: How Medicare “Negotiation” Works
The IRA’s Drug Price Negotiation Program is not a “negotiation” in the way you negotiate with a PBM. It is a one-way mechanism for the government to set a price.59
- Who is Targeted: The law targets “qualifying single source drugs” (brand-name drugs with no generic/biosimilar competition) that have the highest total expenditure for Medicare Part D (pharmacy) and Part B (physician-administered).59
- The Timeline: The first 10 Part D drugs were selected in 2023. This list includes blockbusters you all know: Eliquis, Jardiance, Xarelto, Januvia, Farxiga, Entresto, Enbrel, Imbruvica, and Stelara.59 Their new, “negotiated” prices will take effect on January 1, 2026.60
- The “Price Cut”: The law doesn’t just allow negotiation; it mandates a price ceiling. The “Maximum Fair Price” (MFP) cannot be higher than a certain percentage of the non-federal Average Manufacturer Price (AMP).60 The end result is a massive, forced price cut estimated to be between 25% and 65%.61
The “Small Molecule Penalty”: A 9-Year vs. 13-Year Clock
Now we come to the single most important, and strategically alarming, provision in the entire law. Buried in the text is a new IP-based distinction that has created a massive, and likely unintended, “penalty” against one class of drugs.
The IRA created two different “safe harbor” clocks for how long a drug can be on the market before it becomes eligible for price negotiation 61:
- Small Molecule Drugs (Pills): These drugs (which make up 90% of all medicines 63) have been on the market for 7 years post-approval. They are eligible for selection and negotiation, with the price taking effect just 9 years after their initial FDA approval.61
- Biologics (Large Molecules): These drugs (injectables, infusions) have been on the market for 11 years post-approval. They are protected from negotiation until 13 years after their initial approval.61
The Chilling Effect: How the “Penalty” Is Shifting R&D Investment
This 4-year difference is not a minor detail. It is a catastrophic blow to the small molecule business model.
Why? Because that 9-to-13-year post-launch window is a drug’s peak revenue period.62 This is when the drug is fully established, and before its patents typically expire.
Analysis from IQVIA shows this 4-year “penalty” period (years 10-13) accounts for approximately one-third of a small molecule’s entire lifetime sales revenue.62 For first-in-class novel pills, it’s even worse, accounting for 38-40% of lifetime net sales.62
The IRA has effectively vaporized a third of the potential return on investment for every small molecule drug in development.
The “chilling effect” on R&D was not theoretical; it was immediate and quantifiable.65 R&D investment is now fleeing patient-friendly small molecules and flooding into more complex, procedurally-protected biologics.67
The data is stark. A longitudinal study presented in 2024 64 analyzed the impact of the IRA on post-approval oncology trials (trials for new indications, which often happen in that 9-13 year window). The findings:
- Post-IRA, the monthly average of post-approval clinical trials for small molecule oncology drugs dropped by a staggering 43.6% to 45.3%.
- In contrast, post-approval trials for biologics saw a much smaller, non-statistically significant reduction (e.g., 8.4%).64
This is the perverse, unintended consequence. An R&D executive or a BD team now has a fiduciary duty to question investment in a promising first-in-class pill (9-year clock) and instead favor a me-too biologic (13-year clock). The law, intended to cut costs, has created a new, non-scientific incentive that actively penalizes innovation in the most common and patient-friendly form of medicine.
Case Studies in High-Stakes Pricing: Lessons from the Field
Theory is useful. But for this audience, case studies are everything. Let’s apply this entire framework—VBP, HTAs, PBMs, Patents, and the IRA—to the highest-profile launches (and failures) of the last few years.
The Launch Failure: Aduhelm (Biogen) and the ICER Takedown
- The Asset: Aduhelm (aducanumab), a treatment for Alzheimer’s disease.
- The Price: Biogen launched in June 2021 with an annual list price of $56,000.41
- The Strategy (The “Why”): The launch was built on a monumental unmet need (Alzheimer’s) and a highly controversial FDA Accelerated Approval.69 The FDA overruled its own scientific advisory committee, which voted nearly unanimously against approval.70
- The Flaw (The “Clinical Data Lynchpin”): The approval was not based on a clear clinical benefit (i.e., stopping cognitive decline). It was based on conflicting Phase 3 data (one trial failed, one “succeeded”) 41 and the drug’s effect on a “surrogate endpoint”—its ability to reduce amyloid plaque in the brain.69 The link between plaque reduction and actual cognitive improvement remains unproven.69
- The Gauntlet (The “ICER Takedown”): Biogen had the FDA’s approval. But they had not proven “value.” The “shadow HTA,” ICER, immediately published a blistering report. They analyzed the weak, conflicting clinical data and concluded that the actual value-based price for Aduhelm was not $56,000. It was between $3,000 and $8,400 per year.41
- The Result: Commercial disaster. Payers—led by Medicare—sided with ICER. They refused to cover the drug, issuing severe restrictions that made it virtually inaccessible. Biogen, in a desperate move, slashed the price to $28,200 68, but it was too late. The launch was one of the worst commercial failures in modern pharma history.
- The Lesson: FDA approval is not market access. In the modern era, if you cannot prove value and clinical benefit to the HTA bodies (official or “shadow”), the payers will not pay. Your price will collapse.
The Patent Cliff: The Humira (AbbVie) Biosimilar War
- The Asset: Humira (adalimumab), the best-selling drug in history, for autoimmune diseases.
- The Strategy (The “Patent Thicket”): AbbVie was the master of IP defense. It protected Humira for over 20 years, long after its core patent expired, by building a legendary “patent thicket” of over 100 secondary patents on formulations and methods of use.18
- The Cliff (The “LOE Date”): After years of litigation and settlements, the “thicket” finally broke. The dam of biosimilar competition burst in the US, starting in 2023.72
- The PBM Power Play: This became a perfect case study of the Gross-to-Net Bubble. Biosimilars entered with two different strategies:
- Low-List-Price: Some, like Yusimry, launched with an 85% discount to WAC.73
- High-List-Price: Others launched with a high list price, designed to “play the game” and offer big rebates to PBMs.
- The Result: The PBMs made their move. In 2024, CVS Caremark and Express Scripts announced they were removing the original Humira from their largest commercial formularies.74 This was the “popping” of the gross-to-net bubble. But what did they replace it with?
- CVS Caremark gave preferred status to its own private-label biosimilar, “Cordavis” Hyrimoz, which it sources from Sandoz.74
- Cigna’s Express Scripts favored its own biosimilars, marketed by its subsidiary Quallent Pharmaceuticals.74
- The Lesson: This case study reveals the raw, consolidating power of PBMs. They are no longer just “middlemen.” They are now vertically integrating, becoming payers and producers (via private labels) to capture the “bubble” value for themselves. For a brand company, the PBM is not just a gatekeeper; it is now a direct competitor.
The Market Tsunami: GLP-1s (Novo/Lilly) and the 2025 Medicare Deal
- The Asset: The GLP-1 “fat drugs”: Ozempic/Wegovy (semaglutide) and Mounjaro/Zepbound (tirzepatide).
- The Price: Launched with massive list prices, over $1,000 to $1,350 per month.75
- The Strategy (The “IRP” Problem): The high US price created a political firestorm. The drugs’ popularity, combined with their high cost, made them a target. Politicians, including President Trump, repeatedly hammered the IRP-driven discrepancy: “$88 in London… $1,200 in New York”.77
- The New Model (Political Negotiation): The high price and political pressure became untenable. In November 2025, the Trump administration announced it had cut a direct deal with Novo Nordisk and Eli Lilly—a deal that completely bypassed the PBMs.75
- The New Prices:
- Medicare “Negotiated” Price: $245 per month.76
- Medicare Patient Copay: A flat $50 per month.78
- Uninsured Patients (via TrumpRx.gov): A direct-to-consumer cash price of ~$350/month, trending down to $245.79
- The “Carrot”: What did the pharma companies get in return for this massive price cut? The ultimate prize: Medicare coverage for the obesity indication.78 This was a massive, untapped market of 7 million seniors that was previously excluded.78 They traded price for volume.
- The Lesson: For high-volume, high-spend, politically-sensitive drugs, a new pricing model has emerged: direct political negotiation. The government used the threat of IRP and the carrot of expanded Medicare access to force a deal outside the PBM system. This is a potential future for all blockbuster drugs.
The New Frontier: Zolgensma, Lyfgenia, and the $3M “Pay-for-Performance” Model
- The Asset: One-time, curative cell and gene therapies (CGTs).
- Zolgensma (Novartis): For spinal muscular atrophy (SMA), launched at $2.125 million.81
- Lyfgenia (bluebird bio): For sickle cell disease (SCD), launched at $3.1 million.83
- The Problem (The “Payer Wall”): Payers, especially state Medicaid programs (which cover 50% of all SCD patients 85), cannot sustain these multi-million dollar upfront costs. They create a “financial shock”.86 Furthermore, payers are terrified of the long-term risk: What if they pay $3.1M for a “cure” that fails in 3 or 5 years?.87
- The Solution (The “Outcomes-Based Agreement”): The only viable path to market access is the “pay-for-performance” model.29
- How it Works (Lyfgenia): Bluebird bio announced it had signed multiple OBAs with Medicaid and national commercial payers.84 Here’s the mechanic:
- The payer agrees to pay the $3.1 million upfront.
- However, the contract is “tied to VOE-related hospitalizations”—the primary clinical endpoint for SCD—for a period of three years.85
- If the patient who received the $3.1M therapy is subsequently hospitalized for a vaso-occlusive event (VOE), it means the therapy failed to deliver its curative value.
- If that happens, bluebird bio must pay a massive rebate back to the payer.29
- The Lesson: For ultra-high-cost, potentially curative therapies, the old pricing models are dead. The new model is one of shared risk. Manufacturers must be so confident in their clinical value that they are willing to financially guarantee it.
The Strategic Data Advantage: An Actionable Playbook for Stakeholders
We have deconstructed the theory, the players, and the case studies. Now, what do you do with this information? How do you, in your specific role, use patent and pricing data to create a competitive advantage?
For R&D and Clinical Teams: Designing for Price
Your work in the lab and the clinic is the first and most important step in pricing. The commercial team cannot sell what you do not give them.
- Mandate 1: Stop seeing pricing as a “commercial problem.” Pricing strategy starts at discovery.
- Action 1: Use patent landscape analysis before discovery. Before you commit millions to a target, use patent landscape data to identify true white space, not just another crowded “me-too” target where you’ll be locked into a parity-pricing war.14
- Action 2: The IRA clock is now a core scientific variable. The decision between a small molecule (9-year negotiation clock 64) and a biologic (13-year clock 64) is now a core financial decision, not just a scientific one. The commercial and financial viability of your project may depend on this choice.
- Action 3: Your trial design is your pricing strategy. Understand the “Clinical Data Lynchpin”.26 If you design a non-inferiority trial, you have locked your company into a competitor-based, parity-price strategy.27 Do not expect a premium. If you want a premium, value-based price, you must design for, and win, a superiority trial.
For Business Development & M&A Teams: The IP Due Diligence Playbook
Your job is to buy, sell, and license assets. In pharma, the patent portfolio is the asset.13 Your ability to accurately price that asset is your entire job.
- Mandate 2: Your job is to buy patent-protected revenue streams.
- Action 1: Use patent data for portfolio management. Use patent landscape analysis to map the competitive space.15 Identify acquisition or in-licensing targets that fill your company’s strategic gaps, either in the pipeline or in your LOE-facing “patent thickets”.90
- Action 2: Master IP Due Diligence. Use platforms like DrugPatentWatch to “de-risk” an acquisition before you bid.13 This is a formal “IP due diligence” process that goes far beyond a simple LOE date check.91
- Action 3: Hunt for the “Red Flags.” During due diligence, you are a detective. You must look for the “buried bodies” in the IP portfolio.92 The most common and costly red flags include:
- Freedom-to-Operate (FTO) Risk: This is the big one. Does the target’s amazing drug infringe on a competitor’s broader patent? A patent only gives you the right to exclude others; it does not give you the right to practice your own invention if it’s blocked by someone else’s.94
- Weak or Narrow Claims: Did the patent office reject the broad claims during prosecution, forcing the inventors to accept very narrow ones? This means the patent is easy to “design around”.91
- Broken “Chain of Title”: Does the company actually own the patent? Was the IP fully and cleanly transferred from the university lab where it was discovered?.95
- Missed Maintenance Fees: A shocking “rookie mistake.” Has the patent already lapsed because someone forgot to pay the USPTO maintenance fees?.91
For IP Law Firms & Legal Counsel: From Defense to Offense
Your role is evolving. You are no longer just a “filing” service or a defensive cost center. You are a commercial strategist tasked with maximizing the value of the IP portfolio.
- Mandate 3: Your job is not to file patents; it’s to build revenue-protecting fortresses.
- Action 1: Master the “LOE Strategy.” Proactively advise your clients on their Loss of Exclusivity strategy years in advance. This means building the defensive “patent thicket” 17 with formulation, method-of-use, and delivery device patents to “evergreen” the product and delay the cliff.
- Action 2: Use competitive monitoring as an offensive weapon. Use patent intelligence to monitor competitor activity.96 When a generic files a PIV challenge, analyze its merits and advise the business on the real risk. When a competitor launches, run an FTO analysis to see if they are infringing on your client’s patents.
- Action 3: Mandate cross-functional alignment. The best legal advice is commercially aware. You must be part of a C-suite-level “LOE Steering Committee” that includes Legal, R&D, and Commercial. Legal must understand the “patient switch strategy” (e.g., moving patients from the 1.0 tablet to the 2.0 patented, extended-release version) to ensure the IP filings support it.97
For Investors & Financial Analysts: Pricing the “Patent Cliff”
Your job is to accurately forecast revenue and value assets. The patent data is not “noise”; it is the core variable in your model.
- Mandate 4: The LOE date is your revenue model.
- Action 1: Build your model around the real LOE date. Use tools like DrugPatentWatch to find the actual patent cliff, factoring in all patents, regulatory exclusivities (NCE, ODE), and extensions (PED).13 A model based on a headline “20-year” patent term is wrong.
- Action 2: Treat a Paragraph IV (PIV) challenge as a material event. A PIV filing is a public signal from a generic company that they believe they can break your patent early. Tracking these filings (and the subsequent court rulings or settlements) is the only way to predict if your revenue cliff is going to hit 2, 3, or 5 years sooner than the LOE date in your model.
- Action 3: Use IP strength to adjust your rNPV. The quality of the patent portfolio (a strong CoM “moat” vs. a weak, heavily-challenged “thicket”) is a direct input for your risk-adjusted Net Present Value (rNPV) calculation.91 A weak portfolio deserves a higher discount rate, as its cash flows are far less certain.
Table 2: The Stakeholder Patent Data Playbook
| Stakeholder | Primary Goal | Key Data Points to Track | Strategic Action | Key Red Flags to Find |
| R&D / Clinical Teams | Design high-value, commercially-viable assets. | Patent “white space,” competitor trial designs, IRA timelines. | Design “superiority” trials for VBP. Prioritize biologics or high-value small molecules to mitigate IRA’s 9-year clock.26 | Crowded patent landscapes (“me-too” traps); non-inferiority trial designs that lock in low prices. |
| Business Development / M&A Teams | Acquire and license-in high-value, de-risked assets. | Target’s patent portfolio (CoM, thicket), FTO landscape, PIV challenges, patent-chain-of-title. | Use DrugPatentWatch for IP due diligence. Model the real LOE date. Price the asset based on IP strength.13 | Freedom-to-Operate (FTO) risk 95, broken chain-of-title 95, missed maintenance fees 91, weak claims. |
| IP Law Firms / Legal Counsel | Maximize commercial value of the IP portfolio. | Client’s LOE dates, competitor PIV filings, competitor new launches, secondary patent opportunities. | Build the “patent thicket” (formulation, method-of-use). Form a cross-functional LOE steering committee. Monitor for infringement.17 | A client with a single CoM patent and no “thicket” strategy; a commercial team unaware of its LOE date. |
| Investors / Financial Analysts | Accurately forecast revenue and value companies. | LOE Dates (Patents + FDA Exclusivity), PIV Filings (generic challenges), litigation outcomes, IRA eligibility (9 vs 13 yr). | Build revenue models anchored to the real LOE date.13 Treat PIV challenges as material events that pull the “cliff” forward. Adjust rNPV based on IP strength.13 | A company whose high-revenue drug is 1-2 years from LOE with no follow-on; a small molecule drug entering the IRA 9-year window.64 |
Conclusion: The Future of Pharmaceutical Pricing
The era of simple, cost-plus, or “what the market will bear” pricing is over. We have entered a new, far more complex and fragmented era. The future of pharmaceutical pricing is not a single number, but a multi-variable calculus, a delicate synthesis of four opposing forces.
The launch price of tomorrow will be a function of:
- Demonstrated Value: The non-negotiable, evidence-based proof of clinical superiority and cost-effectiveness, as demanded by HTA bodies like NICE, IQWiG, and the “shadow HTA,” ICER.
- Payer Leverage: The raw, concentrated market power of PBMs, and the strategic necessity of navigating the “Gross-to-Net Bubble” to gain formulary access.
- Political Will: A new and volatile variable. This includes the “price contagion” of global IRP and the domestic “negotiation” clubs of the IRA and direct-to-government deals.
- IP-Protected Lifespan: The ultimate anchor. The real, risk-adjusted LOE date, meticulously calculated from a deep understanding of patent and exclusivity data.
The winners of this new era will not be the companies with the best science alone. The winners will be the organizations that are structured to win this IP-driven war—the companies that integrate their legal, R&D, and commercial strategies from the earliest days of discovery, and who understand that the patent isn’t just a legal shield; it is the blueprint for the price itself.
Key Takeaways
- Pricing Is an IP Strategy: The launch price is not a last-minute decision. It is a long-term strategy anchored by the quality, type, and duration of your patent and exclusivity portfolio. The Loss of Exclusivity (LOE) date is the most important variable in your financial model.
- The R&D Myth vs. Reality: The ~$2.8B R&D cost is a political narrative to justify the patent system, not a pricing formula. The true price is set by “what the market will bear,” which is a function of clinical value, competitive landscape, and payer leverage.
- Your Trial Design Is Your Pricing Strategy: A “Superiority” trial is your only path to a premium, Value-Based Price. A “Non-Inferiority” trial is a business decision that locks you into a lower, “me-too” competitor-based price.
- The “Gross-to-Net Bubble” Is the System: The $334B gap between high “List Prices” and low “Net Prices” is driven by a perverse PBM incentive. PBMs prefer high-list/high-rebate drugs, and patient coinsurance is based on the inflated list price.
- The “Small Molecule Penalty” Is Reshaping R&D: The IRA’s 9-year negotiation clock for pills (vs. 13 years for biologics) is catastrophic for the small molecule business model. Data shows R&D investment is already fleeing small molecules in favor of biologics.
- HTAs Are Not Monolithic (NICE vs. IQWiG): Global launch teams need two different value dossiers. The UK (NICE) is built on economics (the QALY). Germany (IQWiG) rejects the QALY and is built on comparative clinical data.
- IRP Has an Unintended Consequence: International Reference Pricing, a tool to lower prices, creates a rational business incentive for companies to delay or withhold launching new drugs in smaller, poorer countries to prevent “price contagion.”
- New Pricing Models Are Emerging: The old models are breaking. The future is a mix of:
- Political Negotiation: (e.g., the 2025 GLP-1 deal that bypassed PBMs).
- Outcomes-Based Agreements: (e.g., Lyfgenia’s $3.1M “pay-for-performance” model).
- Patent Data Is Actionable for All Stakeholders: R&D teams use it to find targets. BD uses it for due diligence (e.g., checking FTO risk). IP Law Firms use it to build “thickets.” Investors use it to find the real “patent cliff” and track PIV challenges as material events.
Frequently Asked Questions (FAQ)
1. What is the “small molecule penalty” in the Inflation Reduction Act (IRA)?
- This is a critical, and likely unintended, provision in the IRA that creates two different timelines for drugs to be “safe” from government price negotiation. Small molecule drugs (typically pills) are protected for only 9 years post-launch, while biologics (typically injectables/infusions) are protected for 13 years.62 Because the 9-to-13-year period is a drug’s peak revenue window 62, this “penalty” disproportionately harms the small molecule business model and is causing a “chilling effect” as R&D investment shifts toward biologics.64
2. What is the difference between a patent and regulatory exclusivity?
- They are two separate and independent clocks that both protect a drug’s monopoly. A patent is granted by the USPTO (Patent Office) and protects the invention (e.g., the molecule, the formulation) for ~20 years from its filing date.16 Regulatory Exclusivity is granted by the FDA upon approval and protects the clinical trial data. It bars the FDA from approving a generic for a set period (e.g., 5 years for a New Chemical Entity, 7 years for an Orphan Drug) regardless of the patent status.19 Your true monopoly is the longer of these two clocks.
3. Why would a drug company launch with a $1,000 list price instead of a simple $300 low price?
- This is due to the “Gross-to-Net Bubble” and the perverse incentives of the U.S. PBM (Pharmacy Benefit Manager) system.52 PBMs, who control patient access, demand large rebates in exchange for formulary placement. These rebates are calculated as a percentage of the high list price.47 A simple $300 net-price drug offers no rebate, so PBMs have no incentive to cover it. A $1,000 drug with a $700 rebate does give the PBM a margin to profit from, even though the manufacturer only keeps $300. This system inflates list prices, and patients on coinsurance (which is based on the list price) end up paying the price.51
4. What is the main difference between how NICE (UK) and IQWiG (Germany) evaluate a new drug’s price?
- It’s a critical difference in methodology. NICE (UK) is built around economics. It asks, “Is this drug cost-effective?” It determines this by calculating the “cost-per-QALY” (Quality-Adjusted Life Year) and comparing it to a set threshold (e.g., £20,000/QALY).38 IQWiG (Germany) rejects the QALY model.38 It is built around clinical data. It asks, “Is this drug clinically better than the current standard of care?” It focuses purely on comparative efficacy and patient-relevant benefits, with economics playing almost no role in the initial assessment.38
5. How does patent data really impact an investor’s financial model?
- Patent data is the financial model’s core set of variables. The Loss of Exclusivity (LOE) date is the “patent cliff” and defines the entire revenue forecast.13 Step one for an investor is using tools like DrugPatentWatch to find that real date, factoring in all patents, extensions, and regulatory exclusivities.13 Step two is de-risking that date. Tracking Paragraph IV (PIV) challenges (when a generic sues to break the patent) is a material event. A PIV filing tells an investor the “cliff” might be coming sooner than the patent’s expiration date, forcing a significant downward adjustment to the revenue forecast and the stock’s valuation.
Works cited
- Implementing Patent-Expiry Forecasting: A 12-Step Checklist for Competitive Advantage, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/implementing-patent-expiry-forecasting-a-12-step-checklist-for-competitive-advantage/
- Setting the Correct Medicine Launch Prices: A Comprehensive Guide – DrugPatentWatch, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/setting-the-correct-medicine-launch-prices-a-comprehensive-guide/
- The Economics of Drug Discovery and the Impact of Patents – R Street Institute, accessed November 9, 2025, https://www.rstreet.org/commentary/the-economics-of-drug-discovery-and-the-impact-of-patents/
- Drug Patents: How Pharmaceutical IP Incentivizes Innovation and Affects Pricing – ALS TDI, accessed November 9, 2025, https://www.als.net/news/drug-patents/
- Breaking down silos: How pharma is speeding up drug R&D with data – AVEVA, accessed November 9, 2025, https://www.aveva.com/en/perspectives/blog/how-pharma-is-speeding-up-drug-r-and-d-with-data/
- Five things to understand about pharmaceutical R&D, accessed November 9, 2025, https://www.brookings.edu/articles/five-things-to-understand-about-pharmaceutical-rd/
- Do R&D costs justify the price of drugs? Nope, new study says | PharmaVoice, accessed November 9, 2025, https://www.pharmavoice.com/news/rd-costs-justify-price-drugs-BMJ/643774/
- High R&D Isn’t Necessarily Why Drugs Are So Expensive – UC San Diego Today, accessed November 9, 2025, https://today.ucsd.edu/story/high-rd-isnt-necessarily-why-drugs-are-so-expensive
- Drug prices not justified by industry’s research and development spending – BMJ Group, accessed November 9, 2025, https://bmjgroup.com/drug-prices-not-justified-by-industrys-research-and-development-spending/
- Navigating pharma loss of exclusivity | EY – US, accessed November 9, 2025, https://www.ey.com/en_us/insights/life-sciences/navigating-pharma-loss-of-exclusivity
- The Impact of Patent Expiry on Drug Prices: A Systematic Literature Review – PMC – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6132437/
- Life after patent: Drug price dynamics and cost-effectiveness analysis – medRxiv, accessed November 9, 2025, https://www.medrxiv.org/content/10.1101/2023.06.08.23290510v1.full-text
- Full article: The impact of patent expiry on drug prices: insights from the Dutch market, accessed November 9, 2025, https://www.tandfonline.com/doi/full/10.1080/20016689.2020.1849984
- Leveraging Drug Patent Data for Strategic Investment Decisions: A …, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/leveraging-drug-patent-data-for-strategic-investment-decisions-a-comprehensive-analysis/
- Balancing Patents and Drug Prices: Navigating the Complex Landscape of Pharmaceutical Innovation and Accessibility – DrugPatentWatch, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/balancing-patents-drug-prices/
- Best Practices for Drug Patent Portfolio Management: Leveraging Patent Data for Competitive Advantage – DrugPatentWatch, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/best-practices-for-drug-patent-portfolio-management-2/
- The Role of Patents and Regulatory Exclusivities in Drug Pricing | Congress.gov, accessed November 9, 2025, https://www.congress.gov/crs-product/R46679
- Drug patents: how they work, duration & importance – Questel, accessed November 9, 2025, https://www.questel.com/resourcehub/understanding-drug-patents-duration-process-challenges-and-real-world-impact/
- Decoding Drug Pricing Models: A Strategic Guide to Market …, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/decoding-drug-pricing-models-a-strategic-guide-to-market-domination/
- Frequently Asked Questions on Patents and Exclusivity – FDA, accessed November 9, 2025, https://www.fda.gov/drugs/development-approval-process-drugs/frequently-asked-questions-patents-and-exclusivity
- Managing Patent Portfolios in the Pharmaceutical Industry – PatentPC, accessed November 9, 2025, https://patentpc.com/blog/managing-patent-portfolios-in-the-pharmaceutical-industry
- Drug patent and exclusivity study – USPTO, accessed November 9, 2025, https://www.uspto.gov/sites/default/files/documents/USPTO_Drug_Patent_and_Exclusivity_Study_Report.pdf
- How can I better understand Patents and Exclusivity? – FDA, accessed November 9, 2025, https://www.fda.gov/industry/fda-basics-industry/how-can-i-better-understand-patents-and-exclusivity
- Patents and Exclusivity | FDA, accessed November 9, 2025, https://www.fda.gov/media/92548/download
- FDA Drug Info Rounds, July 2012: Patents and Exclusivity – YouTube, accessed November 9, 2025, https://www.youtube.com/watch?v=Npx5UV_yQOA
- Deconstructing Drug Pricing Strategy for Big Pharma – DrugPatentWatch – Transform Data into Market Domination, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/deconstructing-drug-pricing-strategy-for-big-pharma/
- Trial Designs—Non-inferiority vs. Superiority vs. Equivalence – Certara, accessed November 9, 2025, https://www.certara.com/knowledge-base/trial-designs-non-inferiority-vs-superiority-vs-equivalence/
- Evaluating “superiority”, “equivalence” and “non-inferiority” in clinical trials – PMC – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6074290/
- Non-Inferiority Clinical Trials to Establish Effectiveness; Guidance for Industry – FDA, accessed November 9, 2025, https://www.fda.gov/media/78504/download
- Innovative Payment Models for Sickle-Cell Disease Gene Therapies in Medicaid, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12011968/
- Novel payment models to facilitate patient access to gene therapies – Dolon, accessed November 9, 2025, https://dolon.com/wp-content/uploads/2024/10/Novel-payment-models-to-facilitate-patient-access-to-gene-therapy-2024-10-10-vF.pdf?x45798
- Breakthroughs and Barriers: Advancing Value-Based Payment for Transformative Therapies – Duke-Margolis Institute for Health Policy, accessed November 9, 2025, https://healthpolicy.duke.edu/sites/default/files/2021-05/advancing_vbp_for_transformative_therapies.pdf
- How the Federal Government Could Support Innovative Medicaid Payment Arrangements for High-Cost Drugs | Commonwealth Fund, accessed November 9, 2025, https://www.commonwealthfund.org/blog/2025/how-federal-government-could-support-innovative-medicaid-payment-arrangements-high-cost
- Assessing CMMI’s proposals on Medicaid payment for cell and gene therapies | Brookings, accessed November 9, 2025, https://www.brookings.edu/articles/assessing-cmmis-proposals-on-medicaid-payment-for-cell-and-gene-therapies/
- A theory on ICER pricing and optimal levels of cost-effectiveness …, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10484610/
- Conditional Approval and Value-Based Pricing for New Health Technologies – Wharton Faculty Platform – University of Pennsylvania, accessed November 9, 2025, https://faculty.wharton.upenn.edu/wp-content/uploads/2016/11/Conditional_Approval-final.pdf
- A Framework for Using Cost-effectiveness Analysis to Support Pricing and Reimbursement Decisions for New Pharmaceuticals in a Context of Evolving Treatments, Prices, and Evidence – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12227514/
- ICER 2019 Perspectives on Cost-Effectiveness Threshold Ranges, accessed November 9, 2025, https://icer.org/wp-content/uploads/2023/08/ICER_2019_Perspectives-on-Cost-Effectiveness-Threshold-Ranges.pdf
- Health technology assessment (HTA) in England, France and …, accessed November 9, 2025, https://becarispublishing.com/doi/10.2217/cer-2021-0047
- Investigation of Factors Considered by Health Technology Assessment Agencies in Eight Countries – PMC – PubMed Central, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7895890/
- Value Assessment Methods and Pricing Recommendations for Potential Cures – ICER, accessed November 9, 2025, https://icer.org/wp-content/uploads/2020/10/ICER_SST_Report_Response_to_Comments_111219.pdf
- Biogen’s $56K price tag on Aduhelm? Think again, ICER says …, accessed November 9, 2025, https://www.fiercepharma.com/pharma/biogen-s-56k-price-tag-for-alzheimer-s-drug-aduhelm-worth-it-watchdog-says-try-more-like-8
- European health technology assessment | IQWiG.de, accessed November 9, 2025, https://www.iqwig.de/en/presse/in-the-focus/european-health-technology-assessment/
- HTA – Health Technologies Economic Evaluation – IQWiG, accessed November 9, 2025, https://www.iqwig.de/veranstaltungen/hs14_harousseau_hta-the_future_role_of_economics.pdf
- The Role of Pharmacy Benefit Managers and Skyrocketing Cost of Medications – PMC – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11482839/
- What Pharmacy Benefit Managers Do, and How They Contribute to Drug Spending, accessed November 9, 2025, https://www.commonwealthfund.org/publications/explainer/2025/mar/what-pharmacy-benefit-managers-do-how-they-contribute-drug-spending
- 5 Things To Know About Pharmacy Benefit Managers – Center for American Progress, accessed November 9, 2025, https://www.americanprogress.org/article/5-things-to-know-about-pharmacy-benefit-managers/
- Pharmacy Benefit Managers, Rebates, and Drug Prices: Conflicts of Interest in the Market for Prescription Drugs – Yale Law School Open Scholarship Repository, accessed November 9, 2025, https://openyls.law.yale.edu/server/api/core/bitstreams/fc20e184-b2d6-4b02-a0f6-a495e3fb5cd2/content
- accessed November 9, 2025, https://www.pssny.org/page/PBMBasics#:~:text=PBMs%20and%20Drug%20Manufacturer%20Rebates,drug%2C%20the%20higher%20the%20rebate.
- Understanding Health Spending | National Pharmaceutical Council, accessed November 9, 2025, https://www.npcnow.org/topics/health-spending/understanding-health-spending
- Glossary of Drug Pricing Terms | PCMA – Pharmaceutical Care Management Association, accessed November 9, 2025, https://www.pcmanet.org/glossary-of-drug-pricing-terms/
- PBM Power: The Gross-to-Net Bubble Reached … – Drug Channels, accessed November 9, 2025, https://www.drugchannels.net/2024/07/pbm-power-gross-to-net-bubble-reached.html
- Novo Nordisk Sheds New Light on PBM Rebates … – Drug Channels, accessed November 9, 2025, https://www.drugchannels.net/2016/12/novo-nordisk-sheds-new-light-on-pbm.html
- The PBM Effect: Regulatory and Market Implications for Life Sciences Companies and Healthcare Providers | Buchanan Ingersoll & Rooney PC, accessed November 9, 2025, https://www.bipc.com/the-pbm-effect-regulatory-and-market-implications-for-life-sciences-companies-and-healthcare-providers
- PBM Basics – Pharmacists Society of the State of New York, accessed November 9, 2025, https://www.pssny.org/page/PBMBasics
- Role of PBMs on Patient Access and Affordability of Prescription Drugs – Alliance for Aging Research, accessed November 9, 2025, https://www.agingresearch.org/wp-content/uploads/2022/05/FTC-PBM-Final-5.20.22.pdf
- EFPIA – Principles for application of international reference pricing systems, accessed November 9, 2025, https://www.efpia.eu/media/15406/efpia-position-paper-principles-for-application-of-international-reference-pricing-systems-june-2014.pdf
- EU directive impact on product launch and IRP challenges, accessed November 9, 2025, https://www.simon-kucher.com/en/insights/new-eu-directive-optimizing-pharma-launch-sequences-and-navigating-irp-challenges
- U.S. International Reference Pricing: Global Implications and Pharma Strategy – Certara, accessed November 9, 2025, https://www.certara.com/blog/u-s-international-reference-pricing-global-implications-and-pharma-strategy/
- Inflation Reduction Act Research Series— Medicare Drug Price Negotiation Program – https: // aspe . hhs . gov., accessed November 9, 2025, https://aspe.hhs.gov/sites/default/files/documents/4bf549a55308c3aadc74b34abcb7a1d1/ira-drug-negotiation-report.pdf
- Impact of federal negotiation of prescription drug prices – Brookings Institution, accessed November 9, 2025, https://www.brookings.edu/articles/impact-of-federal-negotiation-of-prescription-drug-prices/
- Summary of Medicare Drug Negotiation Program in Inflation Reduction Act and Impact on Pharmacies and Providers Publications – Bass, Berry & Sims PLC, accessed November 9, 2025, https://www.bassberry.com/news/medicare-drug-negotiation-program-in-inflation-reduction-act/
- Medicare’s Drug Price Negotiation Program: The Disproportionate …, accessed November 9, 2025, https://www.iqvia.com/locations/united-states/blogs/2024/12/medicares-drug-price-negotiation-program
- The Inflation Reduction Act & the Small Molecule Penalty, accessed November 9, 2025, https://cahc.net/the-inflation-reduction-act-the-small-molecule-penalty/
- Early impact of the Inflation Reduction Act on small molecule vs …, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12392883/
- Effect of the Inflation Reduction Act on Drug Innovation – ISPOR, accessed November 9, 2025, https://www.ispor.org/heor-resources/presentations-database/presentation-cti/ispor-europe-2025/poster-session-3-2/effect-of-the-inflation-reduction-act-on-drug-innovation
- Medicare Drug Price Negotiation has Chilling Effect on Generic and Biosimilar Medicines Development and Availability, accessed November 9, 2025, https://accessiblemeds.org/resources/press-releases/medicare-drug-price-negotiation-has-chilling-effect-on-generic-and-biosimilar-medicines-development-and-availability/
- Navigating IRA’s Impact on Drug Pricing and Innovation | BCG, accessed November 9, 2025, https://www.bcg.com/publications/2023/navigating-inflation-reduction-act-impact-on-drug-pricing-innovation
- Aduhelm, the Newly Approved Medication for Alzheimer Disease: What Epidemiologists Can Learn and What Epidemiology Can Offer – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9614924/
- Ignoring the Experts: Implications of the FDA’s Aduhelm Approval | American Journal of Law & Medicine | Cambridge Core, accessed November 9, 2025, https://www.cambridge.org/core/journals/american-journal-of-law-and-medicine/article/ignoring-the-experts-implications-of-the-fdas-aduhelm-approval/21CED616643C9120F725E3325559D323
- Insights on FDA’s controversial approval of Alzheimer’s drug – JHU Hub, accessed November 9, 2025, https://hub.jhu.edu/2021/06/21/fda-aduhelm-approval/
- Biogen’s Aduhelm controversy as a case study for accelerated approval biomarkers in Alzheimer’s and related diseases – MIT Science Policy Review, accessed November 9, 2025, https://sciencepolicyreview.org/2022/07/mitspr-191618003012/
- PSG Report: Humira Biosimilars Ease Specialty Drug Claim Costs, accessed November 9, 2025, https://www.managedhealthcareexecutive.com/view/psg-report-humira-biosimilars-ease-specialty-drug-claim-costs
- Biosimilar Market Share: Growth and Price Trends in Q1 2025 – AJMC, accessed November 9, 2025, https://www.ajmc.com/view/biosimilar-market-share-growth-and-price-trends-in-q1-2025
- Humira Biosimilar Price War Update: Should We Be … – Drug Channels, accessed November 9, 2025, https://www.drugchannels.net/2024/09/humira-biosimilar-price-war-update.html
- Medicare Will Cover GLP-1s for Obesity Under Deal with Pharma, accessed November 9, 2025, https://www.hmpgloballearningnetwork.com/site/rheum/news/medicare-will-cover-glp-1s-obesity-under-deal-pharma
- Fact Sheet: President Donald J. Trump Announces Major Developments in Bringing Most-Favored-Nation Pricing to American Patients – The White House, accessed November 9, 2025, https://www.whitehouse.gov/fact-sheets/2025/11/fact-sheet-president-donald-j-trump-announces-major-developments-in-bringing-most-favored-nation-pricing-to-american-patients/
- Trump, long fixated on ‘fat drug,’ announces deal to lower its price, accessed November 9, 2025, https://www.washingtonpost.com/health/2025/11/06/ozempic-wegovy-trump-price-medicare-deal/
- What you need to know about Medicare coverage for weight-loss drugs, accessed November 9, 2025, https://www.washingtonpost.com/health/2025/11/07/weight-loss-drugs-medicare-seniors-diabetes-obesity/
- Trump announces plan to cut cost of weight loss drugs and expand access, accessed November 9, 2025, https://www.theguardian.com/us-news/2025/nov/06/trump-plan-weight-loss-drugs
- Medicare to Cover GLP-1 Drugs for as Little as $50 a Month Under Trump Plan, accessed November 9, 2025, https://www.investopedia.com/trump-negotiates-discounts-for-weight-loss-drugs-11845161
- Four Takeaways from the Zolgensma Pricing Storm | PharmExec, accessed November 9, 2025, https://www.pharmexec.com/view/cost-climate-change-case-study
- Full article: An updated cost-utility model for onasemnogene abeparvovec (Zolgensma®) in spinal muscular atrophy type 1 patients and comparison with evaluation by the Institute for Clinical and Effectiveness Review (ICER) – Taylor & Francis Online, accessed November 9, 2025, https://www.tandfonline.com/doi/full/10.1080/20016689.2021.1889841
- Bluebird signs major coverage deal for sickle cell gene therapy Lyfgenia, easing some price concerns | Fierce Pharma, accessed November 9, 2025, https://www.fiercepharma.com/pharma/bluebird-signs-first-deal-sickle-cell-gene-therapy-lyfgenia-covering-nearly-third-us
- Bluebird Bio Enters First Outcomes-Based Agreement with Medicaid for SCD Gene Therapy, accessed November 9, 2025, https://globalgenes.org/raredaily/bluebird-bio-enters-first-outcomes-based-agreement-with-medicaid-for-scd-gene-therapy/
- bluebird bio Announces First Outcomes-Based Agreement with Medicaid for Sickle Cell Disease Gene Therapy, accessed November 9, 2025, https://investor.bluebirdbio.com/news-releases/news-release-details/bluebird-bio-announces-first-outcomes-based-agreement-medicaid
- Managing the Challenges of Paying for Gene Therapy … – ICER, accessed November 9, 2025, https://icer.org/wp-content/uploads/2024/04/Managing-the-Challenges-of-Paying-for-Gene-Therapy-_-ICER-NEWDIGS-White-Paper-2024_final.pdf
- Pricing Zolgensma – the world’s most expensive drug – PMC – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8725676/
- Spinal Muscular Atrophy Therapies: ICER Grounds the Price to Value Conversation in Facts, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10403758/
- External innovation: Biopharma dealmaking to boost R&D productivity – McKinsey, accessed November 9, 2025, https://www.mckinsey.com/industries/life-sciences/our-insights/external-innovation-biopharma-dealmaking-to-boost-r-and-d-productivity
- Strategic Patenting by Pharmaceutical Companies – Should Competition Law Intervene? – PMC – NIH, accessed November 9, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7592140/
- A Comprehensive Guide to Pharmaceutical Patent Due Diligence in …, accessed November 9, 2025, https://www.drugpatentwatch.com/blog/ma-patent-due-diligence-comprehensive-guide/
- Biotech & Pharma Due Diligence Best Practices, Pitfalls & Checklist – Alacrita Consulting, accessed November 9, 2025, https://www.alacrita.com/whitepapers/due-diligence-the-pinnacle-of-expertise-based-consulting
- Precision in pharma: The critical role of due diligence for industry success – Simon-Kucher, accessed November 9, 2025, https://www.simon-kucher.com/en/insights/precision-pharma-critical-role-due-diligence-industry-success
- How IP Diligence Helps Corporate Lawyers Close the Life Sciences Deal, accessed November 9, 2025, https://www.americanbar.org/groups/business_law/resources/business-law-today/2024-december/how-ip-diligence-helps-corporate-lawyers-close-life-sciences-deal/
- VC Due Diligence Process for Life Sciences Investments – Excedr, accessed November 9, 2025, https://www.excedr.com/blog/vc-due-diligence-process-for-life-sciences-investments
- The Impact of Patent Expiry on IP Protection Strategies – PatentPC, accessed November 9, 2025, https://patentpc.com/blog/the-impact-of-patent-expiry-on-ip-protection-strategies