Have you ever looked at your “3-month supply” of medication and done the math? A typical quarter of the year—say, January, February, and March—adds up to 90 days. But another quarter, like April, May, and June, comes to 91 days. And yet another, July, August, and September, totals 92 days. So why, regardless of the season, does your prescription bottle almost invariably contain a neat, round 90-day supply? This two-day discrepancy, this seemingly trivial rounding error, is anything but. It’s a clue. It’s the loose thread that, when pulled, unravels the entire complex, and often confounding, tapestry of the American pharmaceutical system.
This isn’t an oversight; it’s a feature. The 90-day standard is not a unit of time, but a meticulously engineered unit of commerce. It represents a hard-won compromise, a nexus point where the competing forces of regulatory constraint, operational efficiency, patient convenience, and—above all—powerful financial incentives collide and find a precarious equilibrium. As one clinical pharmacist noted, “The 92-day supply is a standardized approach in pharmacy practice, designed to balance patient convenience with regulatory compliance”. While true on the surface, this simple explanation belies a much deeper and more consequential reality. The balance is not an equal one; it is profoundly tilted by the economic architecture that governs how drugs are priced, paid for, and distributed in the United States.
To truly understand this puzzle, we must look beyond the pharmacy counter and into the boardrooms of insurers, the data centers of Pharmacy Benefit Managers (PBMs), the production lines of pharmaceutical manufacturers, and the halls of regulatory agencies. We must explore how a simple number—90—became the magic number that simplifies billing cycles, optimizes logistics, and serves as a critical lever in the multi-trillion-dollar chess game of healthcare. This report will deconstruct that system piece by piece, revealing how those two missing days tell a story not just about your prescription, but about the very nature of power, profit, and patient care in modern medicine.
Part I: The Architecture of a Standard – Why 90 Became the Magic Number
The journey to the standardized 90-day prescription is not a story of a single decree or a moment of invention. It is an evolutionary tale, shaped over a century by the gradual transformation of medicine from a bespoke craft into a massive, industrialized system. The conventions we now take for granted were forged in response to new laws, new technologies, and new economic realities that demanded order and predictability where there once was none.
Historical Roots: From Apothecary Jars to Standardized Dispensing
For centuries, the concept of a “standard” supply was alien. Medicine was a local, personalized affair. The apothecary, a respected community medical provider, was both diagnostician and manufacturer.2 Prescriptions were often compounded on-site from raw materials—herbs, minerals, and chemicals—procured from wholesalers or importers. The earliest known record of such a compounded medicine dates back to the 6th century BC. In 19th-century America, physicians often prepared medicines at a patient’s bedside from herbs carried in their saddlebags, and the first “drug stores” were often simply the offices of doctors who kept larger batches of their remedies on hand. The prescription itself was a set of instructions written in Latin on any handy piece of paper, directing the pharmacist to “take thou” (Rx) a list of ingredients and prepare a specific formulation, like a dozen pills.
This world of bespoke medicine began to change with the rise of industrial pharmaceutical manufacturing and the corresponding need for regulation. The passage of the 1951 Durham-Humphrey Amendment to the Federal Food, Drug, and Cosmetic Act of 1938 was a pivotal moment. It formally created the distinction between over-the-counter (OTC) drugs and “legend” drugs that required a prescription, fundamentally altering the pharmacist’s role.2 No longer a primary compounder and prescriber, the pharmacist’s focus shifted toward dispensing pre-manufactured products and ensuring their safety.
This industrialization coincided with another transformative force: the growth of third-party payers. As health insurance became more common in the mid-20th century, the system required a common language for transactions. To process and reimburse claims for millions of people, insurers needed standardized units. The “30-day supply” emerged as a natural and convenient billing unit, aligning with monthly insurance premiums and billing cycles.1 It was a simple, repeatable quantity that brought predictability to an increasingly complex financial ecosystem. The 90-day supply was a logical extension of this principle, representing a quarterly unit that offered greater convenience and efficiency for stable, long-term medications. This historical shift reveals a crucial truth: the standardization of dispensing quantities was driven less by clinical necessity and more by the administrative and financial demands of a scaled-up healthcare system.
The Regulatory Labyrinth: A Patchwork of Federal and State Mandates
Contrary to popular belief, there is no single, overarching federal law that mandates a 90-day supply for all medications. Instead, the rules governing prescription duration are a complex and often confusing patchwork of federal agency guidelines, state-specific laws, and temporary emergency measures. This fragmented regulatory landscape has created a power vacuum, allowing industry practices, driven by economic incentives, to become the de facto standard.
Federal Oversight: The FDA, DEA, and Controlled Substances
The Food and Drug Administration (FDA) plays a significant role in shaping dispensing practices through its broad oversight of drug safety and labeling, but it does not explicitly mandate a 90-day limit for most drugs. Its guidelines influence how manufacturers package drugs and how pharmacies and insurers approach extended supplies, but they do not set a hard cap.
The most direct federal intervention in supply duration comes from the Drug Enforcement Administration (DEA), which regulates controlled substances due to their potential for abuse and diversion. For years, physicians could only prescribe up to a 30-day supply of Schedule II medications—which include many opioids and stimulants—requiring patients with chronic conditions to make burdensome monthly visits.
In a significant policy shift that went into effect in December 2007, the DEA amended its regulations to allow physicians to issue up to a 90-day supply of a Schedule II controlled substance. This was not a single 90-day prescription, but rather up to three separate 30-day prescriptions issued during a single office visit, each with a “do not fill before” date. This change was the result of long-term advocacy from physician groups like the American Medical Association (AMA) and the American Psychiatric Association (APA), who argued that the monthly visit requirement was an unnecessary hardship for stable, chronically ill patients, such as those with ADHD or chronic pain. While praised for improving patient access and reducing administrative burden, the change also highlighted the delicate balance between convenience and safety, as critics raised concerns about the increased risk of drug diversion and abuse. This DEA rule is a prime example of how the 90-day quantity became formally codified into federal policy for a specific, high-risk class of drugs.
State-Level Variations: The Unspoken Complexity
Adding another layer of complexity, state laws and pharmacy board regulations can vary dramatically, creating what has been described as a “patchwork of practices across the country”. While many states default to federal guidelines, others impose their own specific limits. For instance, a 2012 study noted that most states imposed a dispensing limit of 34 days for Medicaid programs, with only 13 allowing up to a 90-day supply for some medications.
Conversely, some states are more permissive than federal standards might suggest. The AMA’s “Debunking Regulatory Myths” series seeks to clarify these misconceptions for physicians. It points out that for non-controlled substances, the maximum prescription duration is generally 12 months, and at least six states—Idaho, Illinois, Iowa, Maine, South Carolina, and Wyoming—now permit even longer durations. This directly challenges the common assumption that a 90-day supply is a universal legal ceiling. This regulatory fragmentation is key. The absence of a single, uniform national standard for all drugs creates an environment where the operational preferences of the most powerful players—the payers and PBMs who control reimbursement—can easily become the industry norm.
Crisis as a Catalyst: The CARES Act and Medicare Part D
Public health crises can often force rapid and significant changes in healthcare policy, and the COVID-19 pandemic provided a stark example. To ensure that vulnerable seniors could maintain access to their medications while minimizing trips to the pharmacy, the Coronavirus Aid, Relief, and Economic Security (CARES) Act of 2020 included a provision that required Medicare Part D plans to provide up to a 90-day supply of covered drugs to any enrollee who requested it.
This was a major shift. Before the CARES Act, Part D plans had the discretion to allow or deny extended supplies. An analysis of 2020 plan data by the Kaiser Family Foundation revealed the state of play just before the pandemic hit: while three-quarters of enrollees were in plans that covered 90-day supplies for generic drugs, only about half were in plans that did so for brand-name drugs. For high-cost specialty tier drugs, coverage for extended supplies was virtually nonexistent, available to only 4% of enrollees. The CARES Act temporarily suspended this insurer discretion, transforming the 90-day supply from a negotiated benefit into a mandated right. This event underscores that, in the absence of a crisis, the 90-day supply is often treated not as a clinical standard but as a contractual term, applied selectively by payers based on the cost and type of medication.
The fragmented and reactive nature of this regulatory framework is telling. It has not been designed from the top down with a single, coherent vision. Instead, it has evolved through a series of pressures: lobbying from professional groups, responses to public health emergencies, and a general deference to the operational standards established by the industry itself. This lack of a unified federal mandate has created a crucial opening for the financial and administrative giants of the industry to establish their preferred 90-day model as the default standard, not because it is legally required everywhere, but because they control the flow of money that makes the entire system run.
The Supply-Side Equation: Manufacturing, Packaging, and Logistics
Beyond the realms of regulation and history, the 90-day standard is also deeply rooted in the physical realities of making and moving medicine. For pharmaceutical manufacturers and the vast supply chain that connects them to pharmacies, standardization is not just a convenience; it is an economic and logistical necessity.
The efficiency of modern pharmaceutical production hinges on scale and predictability. It is far more cost-effective to produce, package, and ship medications in massive, uniform batches. Consequently, pharmaceutical companies typically design their packaging around standardized supply durations, with 30-day and 90-day counts being the most common. A bottle of 90 tablets is a simple, repeatable unit that streamlines every step of the process, from the robotic arms on the assembly line to the inventory management software in a pharmacy’s back room.
This standardization extends to quality control and safety. Medication expiration dates are carefully calculated and tested based on standard supply durations. While the difference between a 90-day and a 92-day supply might seem negligible from a stability perspective for most drugs, adhering to a consistent standard simplifies the complex process of dating and tracking millions of batches of product across the globe.
For pharmacies, this supply-side standardization is essential for managing their day-to-day operations. Stocking and managing inventory based on 30 and 90-day units is far more straightforward than trying to accommodate a variety of different supply lengths. It allows for more accurate forecasting of demand, reduces the risk of stockouts or overstocking, and simplifies the physical organization of thousands of different medications on pharmacy shelves. In essence, the 90-day supply acts as a common language spoken by everyone in the supply chain, from the factory floor to the pharmacy counter, enabling the smooth and efficient flow of medicine on a national scale.
Part II: The Power Brokers – Following the Money Behind the 90-Day Fill
While history, regulation, and logistics form the foundation of the 90-day standard, its modern dominance is cemented by a far more powerful force: money. To truly solve the 92-day puzzle, one must follow the intricate and often opaque flow of funds through the U.S. pharmaceutical system. At the center of this financial web sit the Pharmacy Benefit Managers (PBMs), the powerful middlemen whose business models are not only compatible with the 90-day supply but are engineered to actively promote it as a tool for profit and market control.
The Middleman’s Empire: Deconstructing the PBM Business Model
Pharmacy Benefit Managers were originally created in the 1960s to act as third-party administrators, processing prescription claims for insurance companies. Today, they are anything but simple administrators. They are colossal, vertically integrated entities that manage the pharmacy benefits for an estimated 275 million Americans. The market is extraordinarily concentrated. Just three companies—CVS Caremark (owned by CVS Health), Express Scripts (owned by Cigna), and Optum Rx (owned by UnitedHealth Group)—process nearly 80% of all prescription claims in the United States.12 In 2023, the combined PBM-segment revenue for these three giants was approximately $473.5 billion.
This immense market power allows PBMs to dictate terms to nearly every other player in the system. They build and manage the pharmacy networks, deciding which pharmacies patients can use and how much those pharmacies will be reimbursed. They negotiate directly with pharmaceutical manufacturers to create formularies—the tiered lists of drugs that an insurance plan will cover—which effectively determines patient access to medications. Their revenue is generated through several complex and often non-transparent mechanisms:
- Spread Pricing: In this model, the PBM charges a health plan a certain price for a medication but reimburses the dispensing pharmacy a lower amount, keeping the difference or “spread” as profit.14 This practice is particularly common with generic drugs and has been heavily scrutinized by regulators for driving up costs for payers like state Medicaid programs.
- Administrative Fees: PBMs charge their clients (insurers, large employers) administrative fees for their services, often calculated on a per-member-per-month (PMPM) or per-claim basis.16
- Rebates and the “Gross-to-Net Bubble”: This is the most significant and controversial source of PBM revenue. PBMs leverage their control over millions of patients to demand massive discounts, or rebates, from brand-name drug manufacturers in exchange for giving a drug preferential placement on their formulary (e.g., a lower co-pay tier).14 This has created a phenomenon known as the “gross-to-net bubble”—the enormous and growing gap between a drug’s official list price (the Wholesale Acquisition Cost, or WAC) and the actual net price the manufacturer receives after all rebates are paid. In 2023, the total value of these gross-to-net reductions for brand-name drugs was estimated to be a staggering $334 billion. Because rebates are often calculated as a percentage of the list price, PBMs can be financially incentivized to favor drugs with higher list prices and larger rebates, even if a competing drug with a lower list price would have a lower net cost to the health plan.14
This business model—built on scale, leverage, and opacity—is the engine that drives the healthcare system’s preference for the 90-day supply.
The 90-Day Incentive Structure: How PBMs Engineer the Market
The 90-day prescription is not merely a passive convention that PBMs accommodate; it is an active strategic tool they use to enhance their business model, control patient behavior, and solidify their market power. They achieve this through a combination of structural advantages and direct financial incentives.
The Mail-Order Mandate
A key element of the PBM strategy is vertical integration. The “Big 3” PBMs are all part of massive healthcare conglomerates that also own their own specialty and mail-order pharmacies.11 Express Scripts® Pharmacy, CenterWell Pharmacy (Humana), and CVS Caremark® are not just vendors; they are core components of the PBMs’ profit centers.22
These mail-order pharmacies are built for high-volume, automated dispensing of maintenance medications, and their entire operational model is optimized around the 90-day supply. PBMs aggressively steer patients toward these affiliated pharmacies using powerful financial incentives. For example, a PBM might offer a patient a 90-day supply of their medication for the cost of two 30-day co-pays, but only if they use the PBM’s mail-order service. They simultaneously prohibit independent community pharmacies within their network from offering the same deal, creating an unlevel playing field and effectively forcing patients to switch to the PBM’s preferred channel. This practice, known as patient steering, locks in revenue for the PBM’s parent company and ensures a steady, predictable stream of 90-day prescriptions that feed their efficient, centralized dispensing facilities.
Adherence as a Financial Metric
PBMs also leverage the concept of medication adherence to drive the adoption of 90-day supplies at the retail pharmacy level. Adherence is typically measured using a metric called Proportion of Days Covered (PDC), which calculates the percentage of days in a given period that a patient has a supply of their medication on hand. A PDC of 80% or higher is generally considered “adherent.”
Payers and PBMs use these adherence scores to rate pharmacy performance, and they tie these scores to financial payments through a system of post-transaction fees known as Direct and Indirect Remuneration (DIR) fees. As one pharmacist on an online forum explained, “Insurance companies will actually take money away from a pharmacy (in the form of DIR fees) 90-120 days after a prescription is filled due to a lack of patient adherence”.
This system creates a powerful incentive for pharmacies to maximize their patients’ adherence scores. Dispensing a 90-day supply is a much more efficient way to achieve a high PDC than dispensing a 30-day supply. A single 90-day fill immediately covers roughly 25% of the days in a year (90/365). To reach the 80% threshold, a patient only needs to refill that prescription two more times during the year. In contrast, a patient on a 30-day supply would need to refill at least ten times to achieve the same score. Therefore, pharmacies are financially motivated to encourage patients to switch to 90-day supplies, not just for workflow efficiency, but to protect themselves from punitive DIR fees. This aligns the financial interests of the retail pharmacy directly with the strategic goals of the PBM.
The promotion of 90-day supplies is far more than a simple matter of convenience or cost-saving on dispensing fees. It is a sophisticated strategy employed by PBMs to entrench their market position and create a more predictable, controllable revenue stream. A patient receiving a 30-day supply has twelve decision points per year—twelve opportunities to discuss switching to a cheaper generic, to stop taking a medication due to side effects, or to change pharmacies. A patient on a 90-day supply has only four such opportunities. This reduction in “churn” creates a stickier, more stable patient population.
This stability becomes a highly valuable asset in the high-stakes negotiations surrounding drug patent expirations. When a blockbuster drug is about to face generic competition, its manufacturer is desperate to slow the erosion of its market share. The manufacturer can offer a PBM a massive rebate to keep the branded drug in a preferred position on its formulary. The PBM, in turn, can deliver on this promise more effectively if a large portion of its members are locked into 90-day supplies, often through its own mail-order pharmacy. This slows the initial uptake of the new generic, preserving revenue for the brand manufacturer and securing a lucrative rebate stream for the PBM. In this context, the 90-day standard is not just an operational detail; it is a strategic lever that directly influences the multi-billion-dollar outcomes of patent cliffs. For any analyst using a platform like DrugPatentWatch to model post-exclusivity revenue decay, understanding the prevalence of 90-day dispensing within a drug’s patient population is a critical and often overlooked variable.
The Payer’s Perspective: A Calculus of Cost and Control
For payers—the health insurance companies and self-insured employers who ultimately foot the bill for prescription drugs—the 90-day standard is primarily viewed through the lens of cost containment and risk management. Their embrace of this convention is driven by a straightforward financial calculus and a belief in its ability to improve long-term health outcomes.
The most immediate and tangible benefit for payers is the reduction in administrative costs. A pharmacy is paid a professional dispensing fee for each prescription it fills. By encouraging a 90-day supply, the payer pays this fee only once per quarter instead of three times. While a single dispensing fee may be modest, when multiplied across millions of members filling billions of prescriptions, the savings become substantial. A 2012 study analyzing Medicaid data found that, after accounting for potential waste, 90-day refills resulted in per-patient-per-year savings across all studied drug classes, ranging from $7.70 for statins to $26.86 for oral hypoglycemics.
Beyond these direct administrative savings, payers are heavily invested in improving medication adherence. Poor adherence to medications for chronic conditions like hypertension, diabetes, and high cholesterol is a primary driver of costly medical events, such as heart attacks, strokes, and preventable hospitalizations.
“This lack of prescription adherence leads to an estimated 125,000 deaths and at least 10 percent of all hospitalizations in the U.S. annually. And it costs the health care system between $100 billion and $289 billion each year.”
From the payer’s perspective, the slightly higher upfront cost of a 90-day supply is a worthwhile investment if it leads to better adherence and avoids a far more expensive hospital stay down the road. Numerous studies support this link, showing that patients on 90-day supplies have significantly higher rates of adherence and persistency.8
Finally, there is the simple matter of the two-day discrepancy. While it may seem trivial to a patient, for an insurance company managing a population of millions, those two extra days of medication in a 92-day supply represent a real and measurable cost. They are paying for two additional days of drug therapy per member, per prescription, four times a year. Without a clear clinical or contractual reason to do so, they have a strong financial incentive to adhere to the simpler, cheaper, and administratively cleaner 90-day standard.
Stakeholder Analysis of 30-Day vs. 90-Day Prescription Supplies
To synthesize the complex and often conflicting motivations driving the 90-day standard, the following table breaks down the perceived benefits, drawbacks, and primary incentives for each key stakeholder in the pharmaceutical ecosystem.
| Stakeholder | Perceived Benefits of 90-Day Supply | Drawbacks/Risks of 90-Day Supply | Primary Financial/Operational Incentive |
| Patient | Fewer trips to the pharmacy; potentially lower co-pays; improved continuity of therapy.1 | Medication waste if therapy changes; financial loss if medication is lost or damaged; potential for stockpiling and safety risks (especially for high-risk drugs).33 | Convenience and immediate out-of-pocket cost savings. |
| Physician/Prescriber | Reduced administrative burden from fewer refill requests; improved patient adherence for stable, chronic conditions.9 | Loss of clinical oversight; difficulty with dose titration for new therapies; significant safety concerns for patients at risk of overdose.34 | Reduced administrative workload and improved population health metrics. |
| Retail Pharmacy | More predictable workflow; improved inventory management; better adherence scores can help avoid PBM penalties (DIR fees).1 | Drastic reduction in revenue from dispensing fees (one fee vs. three); financial pressure from PBMs; contributes to the economic unsustainability of independent pharmacies.28 | Operational efficiency and avoidance of PBM financial penalties. |
| Pharmacy Benefit Manager (PBM) | Drives volume to owned mail-order pharmacies; reduces administrative costs; increases patient “stickiness,” providing leverage with manufacturers; helps meet adherence metrics.11 | Increased scrutiny from regulators and lawmakers over anticompetitive practices like patient steering.38 | Maximizing profit through rebates, spread pricing, and utilization of vertically integrated assets (mail-order pharmacies). |
| Payer (Insurer/Employer) | Lower costs due to fewer dispensing fees; improved medication adherence may lead to lower long-term medical costs (e.g., fewer hospitalizations). | Cost of wasted medication if therapy changes; potential for fraud and abuse. | Reduction of both pharmacy and overall medical expenditures. |
| Brand Manufacturer | Can be used in “rebate wall” strategies with PBMs to slow generic erosion post-patent expiry by locking in patient volume. | Can make “product hopping” to a new formulation more difficult as patients are locked into a 90-day supply of the older version. | Maximizing revenue and defending market share, especially around the patent cliff. |
| Generic Manufacturer | A market dominated by 90-day fills can slow the initial uptake of a new generic, as fewer patients are making refill decisions at the time of launch. | Once established, the 90-day supply model provides a high-volume, predictable market for maintenance medications. | Rapidly capturing market share post-patent expiry through low prices and high volume. |
This table starkly illustrates the web of competing interests. The alignment between PBMs and payers on cost reduction creates immense pressure on retail pharmacies, whose revenue model is directly threatened. The clinical judgment of physicians regarding patient safety can be overridden by the financial and administrative logic of the system. And for pharmaceutical manufacturers, the 90-day standard is a double-edged sword—a tool that can be leveraged for brand defense but also a barrier to lifecycle management. It is within these tensions that the true complexity of the 92-day puzzle resides.
Part III: The Front Lines – Operational Realities for Pharmacies and Physicians
While the strategic decisions that favor the 90-day standard are made in corporate boardrooms and by government agencies, their impact is felt most acutely on the front lines of healthcare—in community pharmacies and physicians’ offices. For the pharmacists and doctors tasked with managing patient care, the 90-day supply presents a profound dilemma, offering a path to greater operational efficiency while simultaneously creating significant financial strain and adding to an already crushing administrative burden.
The Dispenser’s Dilemma: Operational Efficiency vs. Financial Strain
For a busy pharmacy, the allure of the 90-day prescription is undeniable. From a workflow perspective, it is a clear win. Filling one prescription for a 90-day supply is more efficient than filling the same medication three separate times over three months. This allows for a more streamlined process, more predictable inventory management, and fewer interruptions from patients coming in for routine refills.1 As one pharmacist noted, the goal is “shorter lines and a more streamlined work load,” especially for managing patients with multiple medications. The preference is to see a complex patient four times a year rather than twelve, reducing the chaos of on-demand filling.
However, this operational efficiency comes at a steep financial price. The pharmacy business model, particularly for independent pharmacies, relies heavily on the professional dispensing fee paid for each prescription filled. A switch from a 30-day to a 90-day supply cuts that fee-based revenue stream by two-thirds for that medication. This financial pressure is not happening in a vacuum. It is compounded by the broader economic realities of the pharmacy market, where PBMs exert immense control. Pharmacies are often forced to accept below-cost reimbursement for the drugs themselves and are then hit with retroactive DIR fees based on performance metrics they can’t fully control. The combination of declining reimbursement and the push for 90-day supplies has created an existential crisis for many community pharmacies. Since 2013 in Minnesota, for example, a staggering 61% of independently owned pharmacies have closed, with below-cost PBM reimbursement cited as the primary driver.
The Administrative Burden and the Burnout Epidemic
The process of prescribing and refilling medications has become a major source of administrative friction and a significant contributor to burnout among both physicians and pharmacists. The AMA has highlighted this issue extensively, noting that in primary care practices, physicians and their teams spend a considerable amount of time refilling prescriptions for patients who are not even scheduled for an office visit. This “invisible” work adds to the strain on already overburdened clinical staff.
A 2022 study quantified this burden, estimating that physicians spend a median of 4.0 hours per week on drug utilization management tasks like handling prior authorizations and formulary restrictions. When factoring in the time spent by nurses and administrative staff, the total time commitment was associated with a calculated cost of over $75,000 per physician per year. Another survey found that pharmacists spend nearly twice as much time on administrative tasks as they do on direct patient care.
This relentless administrative workload is a key driver of the burnout epidemic plaguing the pharmacy profession. Multiple studies have found that over half of all pharmacists experience symptoms of burnout, with rates among community pharmacists exceeding 80%.43 The COVID-19 pandemic exacerbated these issues, and as of 2024, one in four pharmacists still reports feeling “very stressed” at work. The top sources of stress are overwhelming demand for services (cited by 78% of pharmacists) and a lack of appropriate staff (cited by 73%). In this high-pressure environment, any measure that can reduce administrative tasks and streamline workflow, such as the 90-day supply, is seen as a welcome relief, even if it comes with financial downsides.
A Potential Solution: The Rise of Medication Synchronization
In response to the chaotic and inefficient nature of the traditional refill process, many pharmacies have proactively adopted a service model known as medication synchronization, or “med sync.” Med sync is the process of aligning all of a patient’s chronic medication refills so they can be picked up on a single, convenient day each month or every 90 days. This approach transforms the pharmacy’s workflow from reactive to proactive. Instead of responding to a scattered series of patient requests, the pharmacy team can plan ahead, resolving any insurance issues, confirming refills with doctors, and preparing all of a patient’s medications for a single, scheduled appointment.
The clinical benefits of med sync are well-documented and substantial. By simplifying the refill process and reducing the number of potential gaps in therapy, med sync programs have been shown to dramatically improve medication adherence. One health-system pharmacy study found that 97.8% of patients in their med sync program were adherent (PDC ≥80%), compared to just 70.3% in the control group. The odds of being adherent were nearly 20 times greater for patients in the program. Another large study of nearly 23,000 patients found that med sync was associated with a 3-percentage-point gain in the mean proportion of days covered and a 9% lower rate of hospitalization and emergency department visits.
Med sync represents a strategic adaptation by pharmacies to reclaim a measure of control and demonstrate their value in a system that often treats them as a commodity. The traditional, chaotic refill model leaves pharmacies vulnerable to the financial penalties imposed by PBMs for poor adherence scores. By implementing med sync, pharmacies take direct, proactive control over the refill process, which in turn improves the very adherence metrics PBMs use for performance evaluation. This helps pharmacies protect their bottom line by avoiding punitive DIR fees. Furthermore, the scheduled monthly appointment created by med sync provides a dedicated opportunity for pharmacists to deliver higher-value clinical services, such as comprehensive medication reviews or immunizations, which can be new sources of reimbursement. In this light, med sync is more than just a convenience tool; it is a business model innovation that allows pharmacies to better manage their workload, improve patient outcomes, and fortify their financial health within the challenging, PBM-dominated landscape.
Part IV: The Patient Experience – A Double-Edged Sword
For patients, the 90-day prescription is a classic example of a healthcare trade-off. It offers undeniable benefits in terms of convenience and can play a crucial role in promoting better health outcomes through improved medication adherence. However, these advantages are shadowed by significant downsides, including the potential for medication waste, financial loss, and, in some cases, serious safety risks. The ideal dispensing quantity is not a one-size-fits-all solution but depends heavily on the patient’s clinical stability, the nature of their medication, and their individual circumstances.
The Compelling Case for Adherence and Convenience
The most powerful argument in favor of extended supplies is their proven impact on medication adherence. Non-adherence is one of the most pervasive and costly problems in modern healthcare. When patients don’t take their medications as prescribed, chronic conditions go unmanaged, leading to disease progression, poor clinical outcomes, and a cascade of avoidable medical costs. The scale of the problem is immense: medication non-adherence is associated with an estimated 125,000 deaths annually in the United States and contributes to at least 10% of all hospitalizations.30 The financial toll is staggering, with studies estimating the cost of non-optimized medication therapy at over $528.4 billion per year, representing 16% of total U.S. healthcare spending.
Reducing the number of times a patient has to interact with the healthcare system to get their medication is a simple yet effective way to improve adherence. Every required refill is a potential point of failure—an opportunity to forget, to be unable to afford a co-pay, or to be unable to get to the pharmacy. By reducing the number of potential gaps in care from twelve per year to four, the 90-day supply significantly lowers these barriers.
The data bear this out. A large study of Medicaid beneficiaries found that patients in the 90-day refill group had 20% higher adherence and 23% higher persistency (continuous therapy days) compared to those on 30-day refills. Similarly, a major study of over 350,000 patients who had suffered a myocardial infarction found that 12-month adherence rates were significantly higher for those who filled 90-day supplies across all four major classes of evidence-based medications, including statins (83.1% vs. 75.3%) and P2Y12 inhibitors (78.5% vs. 66.6%).32 For patients managing stable, chronic conditions, the combination of convenience and better health outcomes makes a powerful case for the 90-day standard.
The Hidden Costs: Waste, Safety, and the Risk of Stockpiling
Despite its benefits for adherence, the 90-day supply carries significant and often overlooked risks. These drawbacks are most pronounced when a patient’s treatment plan is in flux or when the medications themselves carry a high potential for harm.
Medication Waste and Financial Loss
For patients who are stable on a long-term medication, a 90-day supply makes perfect sense. However, this is often not the case when a patient is starting a new therapy or when a physician is adjusting the dosage of an existing one. During these trial periods, it is common for a medication to be found ineffective or to cause intolerable side effects, leading the physician to change the prescription. When this happens with a 90-day supply, the remaining two-plus months of medication are wasted. This represents a direct financial loss to the patient (who paid a co-pay) and the insurer, and it results in medication that may be stockpiled in the home or disposed of improperly.34 The American Medical Association has raised concerns about PBM and insurer policies that may require a 90-day supply to be dispensed even when a 30-day supply was prescribed specifically for such a trial period.
A Critical Safety Risk: The Case of Psychiatric Medications
The risks associated with 90-day supplies escalate dramatically when dealing with medications that can be lethal in large quantities. This is a particularly acute concern in the field of psychiatry, where prescribers must constantly assess the suicide risk of their patients. A growing body of research and clinical concern highlights the danger of placing large quantities of potentially lethal medications in the hands of vulnerable individuals. Studies have shown a positive association between the number of tablets available in a medication’s packaging and the quantity consumed in intentional overdose attempts. Antidepressants, for example, were involved in 16-17% of fatalities in a 2020 study of over 421,000 intentional overdoses.
For this reason, psychiatrists often deliberately prescribe limited quantities—such as a 30-day supply with no refills—as a crucial safety measure, especially for patients in high-risk periods, such as immediately following a psychiatric hospitalization.33 This practice allows for frequent check-ins and limits the means available for a lethal overdose. However, this clinical judgment is increasingly being challenged by the economic incentives of the broader healthcare system. There is a growing and alarming trend of insurers, PBMs, and even pharmacies promoting and sometimes unilaterally dispensing 90-day supplies of these high-risk medications, often overriding the prescriber’s explicit safety-based decision.33
In some states, laws permit pharmacists to convert a 30-day prescription with two refills into a single 90-day supply, sometimes without even notifying the prescriber. This practice is deeply concerning to the psychiatric community, as pharmacists are typically not trained in suicide risk assessment and do not have access to the patient’s full clinical history. This creates a dangerous disconnect where a decision made for financial and administrative convenience can directly undermine a critical clinical safety strategy, with potentially tragic consequences.
This conflict reveals a fundamental flaw in how the healthcare system often defines and measures “value.” From the perspective of a PBM or payer, value is often measured through easily quantifiable, population-level metrics like adherence rates (PDC) and the cost per dispensing event. By these measures, 90-day supplies are an unambiguous success. However, from a clinical perspective, particularly for patients who are not stable or are taking high-risk medications, value is defined by safety, flexibility, and the ability to monitor and adjust treatment closely. By these measures, a 30-day supply is often the superior choice. The current system is overwhelmingly optimized to reward the payer’s definition of value. This can lead to a situation where a physician’s sound clinical judgment to prescribe a 30-day supply for safety is overridden by a system-wide policy designed to optimize a financial metric. The result is a system that can appear to be “adherent” on paper but is, in reality, dangerously unsafe for some of its most vulnerable patients.
Voices from the Counter: Patient and Physician Narratives
Behind the data and the policy debates are the lived experiences of patients and providers navigating this complex system every day. Their stories bring the trade-offs of the 90-day puzzle into sharp focus.
One practicing physician, quoted in an AMA publication, captured the frustration of the uncoordinated, 30-day refill cycle: “To expect a patient on six medicines to refill them six different times over the course of 90 days just because they are not synchronized is disheartening… That’s 24 trips to the pharmacy for a medicine every year! If the patient doesn’t have their medicine, they can’t take it and nonadherence leads to poor outcomes”. This highlights the very real burden that a fragmented refill schedule places on patients with chronic conditions.
On the other hand, patient advocacy forums are filled with stories of the financial and emotional toll of high drug costs, which can be exacerbated by the need to pay for a large 90-day supply upfront. One patient shared, “My drugs are so expensive, I have to choose which ones are most important… Most days it is pay the bills or get my medications. I dose them out, so I can afford them (which is not how my doctor prescribed them)”. For those struggling with affordability, a 90-day supply can feel less like a convenience and more like a financial barrier.
Patients with chronic pain face a different set of challenges, often living in fear of being unable to fill their prescriptions due to shortages or pharmacy policies. One patient described the monthly anxiety: “The pharmacies try their best to fill your prescription, but if they don’t have it in stock, they don’t have it in stock. It definitely affects the quality of life. You live in fear every month that this is going to be it”. For these individuals, the debate over 30 vs. 90 days is secondary to the fundamental question of whether they will be able to access their necessary medication at all. These narratives remind us that behind every prescription is a person, and the optimal solution must be flexible enough to accommodate their unique clinical, financial, and personal needs.
Part V: Strategic Implications for the Pharmaceutical Industry
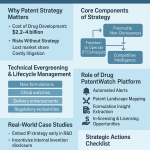
For professionals in the pharmaceutical and biotech sectors, the nuances of prescription dispensing conventions are not merely academic. They are critical variables in the high-stakes world of product lifecycle management, competitive strategy, and revenue forecasting. Understanding the forces that drive the 90-day standard—particularly the powerful economic incentives of PBMs—is essential for navigating the treacherous waters of a drug’s journey from market launch to patent expiration.
The Patent Cliff and the Battle for Post-Exclusivity Market Share
The most significant financial event in the life of any successful drug is the loss of market exclusivity, an event colloquially known as the “patent cliff.” It represents a sudden, sharp, and often catastrophic decline in revenue that occurs when a blockbuster drug’s patents expire, opening the market to a flood of low-cost generic competitors.40 The financial impact is staggering; it is not uncommon for a drug’s revenue to plummet by 80-90% within the first year of generic entry.
The stakes are astronomical. Pfizer’s cholesterol drug Lipitor, once the world’s best-selling medication, saw its sales fall precipitously after its patent expired. More recently, AbbVie’s immunology drug Humira, which generated a breathtaking $21.2 billion in 2022 and roughly $200 billion over its lifetime, began facing biosimilar competition in the U.S. in 2023.57 The industry as a whole is perpetually staring down this precipice; analysts project that between 2025 and 2030, drugs representing over $236 billion in annual revenue are set to lose patent protection.
Navigating this patent cliff is the central strategic challenge for every innovative pharmaceutical company. It requires years of proactive, data-driven planning to develop strategies that can mitigate the inevitable revenue loss and build a bridge to the company’s next generation of products. This is precisely where a deep understanding of the pharmaceutical patent landscape becomes a critical competitive advantage. Platforms like DrugPatentWatch are indispensable in this arena, providing the foundational business intelligence that companies need. By offering detailed data on patent expiration dates, regulatory exclusivities, potential generic and biosimilar challengers, and ongoing patent litigation, such services allow strategists to map the competitive landscape, anticipate threats, and identify opportunities long before a patent cliff arrives. This foresight is the bedrock upon which all effective lifecycle management strategies are built.
Leveraging Dispensing Dynamics: The Lifecycle Management Playbook
The 90-day dispensing standard is not just a passive feature of the market; it is an active lever that can be manipulated by brand manufacturers as part of their defensive strategy against generic erosion. By understanding and influencing these dispensing dynamics, companies can help shape the post-exclusivity market to their advantage.
The “Product Hop” and Reformulation
One of the most common lifecycle management strategies is “product hopping,” where a company develops an improved, next-generation version of an existing drug and secures new patents on it just before the original product’s patent expires. This could be an extended-release formulation that reduces dosing frequency, a new delivery system like a transdermal patch, or a fixed-dose combination with another active ingredient.59 The goal is to switch as many patients as possible to the new, patent-protected version before generics of the original formulation hit the market.
The 90-day supply plays a complex role here. On one hand, it can create “stickiness” that makes it harder to switch patients who are locked into a three-month supply of the old product. On the other hand, it makes the successful execution of the product hop even more critical. Manufacturers will often work closely with PBMs, offering substantial rebates on the new formulation to ensure it receives preferred formulary status, thereby encouraging physicians and pharmacists to make the switch and building a defensive moat against the impending generic competition.
The Authorized Generic (AG) Gambit
Another sophisticated and counterintuitive strategy is the launch of an “authorized generic” or AG.40 An AG is a medication that is identical to the original brand-name drug but is marketed as a generic, typically by a subsidiary of the brand company or a partner generic firm. By launching an AG at the same time as the first independent generic competitor, the brand company can directly compete in the generic space and recapture a significant portion of the market share—and revenue—that would otherwise be lost entirely. The prevalence of 90-day fills can influence the velocity of generic uptake, making the timing and potential profitability of an AG launch a critical strategic calculation. Pfizer famously used this strategy with Lipitor, partnering with Watson Pharmaceuticals to launch an AG and soften the blow of its patent cliff.
The “Rebate Wall”
This strategy directly leverages the power of the PBMs and the 90-day supply. As a blockbuster drug nears patent expiration, the brand manufacturer can offer PBMs extremely deep rebates to maintain the brand’s preferred status on the formulary and, in some cases, to place restrictions on the coverage of competing generics or biosimilars. The PBM’s ability to deliver on this arrangement is enhanced by having a large number of patients on 90-day, mail-order supplies, which locks in volume for the brand and slows the rate at which patients switch to the new, cheaper alternatives. This “rebate wall” was a key component of AbbVie’s formidable defense of Humira, which, combined with a “patent thicket” of over 160 patents, resulted in a remarkably slow uptake of biosimilars in the first year of competition.
The Future of Dispensing: Technology, Regulation, and Personalization
While the 90-day standard is deeply entrenched, the healthcare landscape is not static. A confluence of technological innovation and increasing regulatory pressure has the potential to disrupt this long-standing convention, paving the way for a more flexible and personalized future for medication dispensing.
The Rise of Health Tech
The current 90-day paradigm is fundamentally a product of an information-poor healthcare model. It uses crude, lagging indicators like prescription refill data to estimate patient adherence. However, a new wave of health technology is poised to replace this system of estimation with one of precise, real-time measurement.
Innovations like smart pill bottles and caps from companies like AdhereTech can track when a patient opens their medication bottle, providing direct, real-time data on actual medication-taking behavior. Automated, in-home dispensing devices, such as the Medherent platform from Altruix, not only remind patients to take their medication but also dispense the correct dose at the correct time and can alert caregivers if a dose is missed. These technologies generate a rich stream of data that makes the traditional Proportion of Days Covered (PDC) metric, and the 90-day supply designed to optimize it, seem archaic.
Simultaneously, integrated software platforms from companies like CoverMyMeds, Veradigm, and AdhereHealth are streamlining the entire prescription workflow, from electronic prescribing and prior authorization to claims processing and patient support.65 As these systems become more sophisticated and interconnected, they create the technical capability to move beyond rigid 30 or 90-day standards and support more flexible, personalized dispensing quantities tailored to a patient’s specific clinical needs.
The implications of this technological shift are profound. The entire PBM business model, with its reliance on opaque rebate negotiations and adherence-based DIR fees calculated from crude refill data, is built on the foundations of the current information-poor system. As real-time adherence data becomes more widely available, payers and providers will have a far more accurate way to measure patient behavior and clinical outcomes. This could completely undermine the rationale for the PBMs’ current incentive structures, forcing a radical rethinking of how adherence and value are defined and reimbursed. In the long run, the greatest threat to the 90-day standard may not be legislation, but the disruptive power of data.
The Shifting Regulatory Tide
The business practices of PBMs, once conducted largely out of the public eye, are now under intense scrutiny from state and federal lawmakers. There is a growing bipartisan consensus that the lack of transparency in the pharmaceutical supply chain is contributing to high drug costs. Numerous bills have been introduced in Congress and in state legislatures aimed at reining in PBMs by banning practices like spread pricing, requiring the pass-through of rebates to payers and patients, and increasing overall transparency.15
The American Medical Association has been a vocal critic, with AMA President Dr. Bobby Mukkamala stating, “As PBMs increasingly act in their own self-interest without transparency or accountability, drug prices rise and patients face health risks from cost prohibitive drug treatments… The AMA fully supports greater transparency and accountability that is needed to prohibit PBMs from engaging in opaque and harmful business practices”. While the path for any specific piece of legislation is uncertain, the direction of travel is clear. The regulatory environment is becoming less favorable for the opaque business models that have allowed PBMs to flourish. As these financial incentives are altered, the powerful forces that prop up the rigid 90-day standard may begin to weaken, opening the door to more flexible and patient-centered approaches to dispensing.
Conclusion: Beyond the Calendar – A Puzzle of Power, Profit, and Patients
The 92-day pill puzzle, the simple question of why a three-month supply is always 90 days, reveals itself to be far more than a mathematical curiosity. It is a diagnostic tool, a window into the soul of the American healthcare system. The answer is not a single, simple fact but a complex, multi-layered industry construct, meticulously assembled over decades by the competing interests of every major stakeholder in the pharmaceutical value chain.
The 90-day standard is not an error; it is a deliberate choice. It is the product of a system that prioritizes administrative simplicity and financial predictability over clinical precision. It was born from the logistical needs of an industrial-scale manufacturing and distribution network and nurtured by a fragmented regulatory environment that allowed industry practices to become de facto law. But its modern dominance is a story of power and profit, engineered and enforced by Pharmacy Benefit Managers who have transformed this simple unit of dispensing into a powerful lever for market control. For PBMs and payers, the 90-day supply is an instrument of cost containment and efficiency, a way to reduce administrative fees and optimize adherence metrics that are tied directly to their bottom line.
For those on the front lines, the standard is a double-edged sword. For overworked physicians and pharmacists, it offers a reprieve from the administrative chaos of uncoordinated refills, yet for the pharmacy business model, it represents a significant financial threat. And for the patient, it is the ultimate trade-off: the undeniable convenience of fewer pharmacy trips weighed against the risks of medication waste, the financial burden of large upfront co-pays, and the profound safety concerns for those on high-risk medications.
The two-day discrepancy between the calendar and the prescription bottle is, in the end, the space where all these competing interests are reconciled. It is a compromise where the needs of the system for standardization have, for now, won out over the nuances of individual patient care. But as disruptive technologies introduce real-time data into this ecosystem and as regulators intensify their scrutiny of the system’s opaque financial arrangements, the foundations of this long-standing convention are beginning to show cracks. The future may lead us away from rigid, one-size-fits-all standards and toward a more personalized, data-driven, and truly patient-centric model of dispensing—a future where a three-month supply might just mean 92 days.
Key Takeaways
- The 90-Day Standard is a Unit of Commerce, Not Time: The standardization of prescriptions at 90 days is not a clinical or calendrical decision but an administrative and financial one, designed to simplify billing, reimbursement, and logistics for payers, PBMs, and manufacturers.
- PBMs are the Primary Drivers: Pharmacy Benefit Managers (PBMs) actively promote 90-day supplies as a strategic tool. It drives volume to their own mail-order pharmacies, reduces their administrative costs, and helps them meet adherence metrics that are tied to their revenue through mechanisms like DIR fees.
- Regulatory Fragmentation Creates a Power Vacuum: The absence of a single, uniform federal law mandating prescription duration has allowed the operational and financial preferences of powerful payers and PBMs to become the industry’s default standard.
- Adherence is a Double-Edged Sword: While 90-day supplies are proven to improve medication adherence, which can lower long-term medical costs, they also pose significant risks. These include medication waste when therapies change and critical safety concerns for patients on high-risk medications, such as psychiatric drugs, where large quantities can increase the risk of lethal overdose.
- A Strategic Lever in Lifecycle Management: For pharmaceutical manufacturers, the 90-day standard is a key variable in navigating the patent cliff. It can be used in “rebate wall” strategies to defend market share but can also complicate “product hop” strategies to newer formulations. Understanding these dynamics is crucial for post-exclusivity revenue forecasting.
- Technology is the Ultimate Disruptor: The rise of health tech, such as smart pill bottles and integrated data platforms, provides real-time adherence data. This threatens to make the current system of estimating adherence via refill records (and the 90-day supply designed to optimize it) obsolete, potentially forcing a radical restructuring of PBM business models.
Frequently Asked Questions (FAQ)
1. If the 90-day supply is so entrenched, are there any situations where a 92-day or true three-month supply is actually dispensed?
While uncommon for most standard prescriptions, there are exceptions. Some state Medicaid programs or specific commercial plans may have policies that allow for dispensing up to a 93-day supply to align more closely with a calendar quarter. Additionally, certain specialty medications with very specific treatment protocols or unique packaging may be dispensed in quantities that align with a precise treatment cycle rather than a standard 30 or 90-day unit. However, for the vast majority of maintenance medications processed through major PBMs and payers, the 90-day standard remains the rigid rule due to the overwhelming preference for standardized billing and administrative units.
2. How does the upcoming “patent cliff” for major biologic drugs differ from past cliffs for small-molecule drugs like Lipitor, and how does the 90-day supply factor in?
The upcoming patent cliff for biologics (like Humira and Keytruda) is more complex. Unlike small-molecule generics, which are identical copies, biosimilars are highly similar but not identical, making automatic substitution at the pharmacy level more complicated. This gives brand manufacturers and PBMs more leverage. PBMs can create “rebate walls,” offering payers deep discounts on the original biologic to keep it as the preferred drug, making it difficult for biosimilars to gain market share. The 90-day supply is a key tool in this strategy, as it locks large patient volumes into the branded product for longer periods, slowing the uptake of biosimilars even after they launch. This is a significant reason why the initial market penetration of Humira biosimilars was much slower than anticipated.
3. The AMA is advocating for longer prescription durations, like 15 months (“90 plus four” refills). What are the primary barriers to this becoming a widespread practice?
The primary barriers are not legal but structural and financial. While many states legally permit 12 or 15-month prescriptions for non-controlled substances , the entire reimbursement and dispensing infrastructure is built around 30 and 90-day cycles. PBM and payer systems are designed to adjudicate claims in these increments. Furthermore, PBMs have a financial disincentive to promote this practice widely, as it would reduce the number of claims processed (a source of administrative fees) and lessen their ability to use frequent refills as a lever for steering patients to their mail-order pharmacies or for managing adherence metrics tied to DIR fees. Widespread adoption would require a fundamental re-engineering of PBM and payer claims processing systems and a shift in their underlying business models.
4. With the rise of real-time adherence technology like smart pill bottles, could PBMs adapt their business model to incorporate this data instead of being disrupted by it?
Yes, this is a plausible future scenario. While disruptive, PBMs could pivot their business model from being managers of claims to becoming managers of data. Instead of using crude PDC metrics, a PBM could offer a premium service to payers that integrates real-time adherence data from various smart devices. They could then use this data to trigger personalized interventions—a text message to a patient who missed a dose, a call from a pharmacist, or an alert to a caregiver—and charge payers for these value-added clinical services. This would represent a shift from a transactional model based on dispensing units to a service-based model focused on real-time patient management, potentially allowing them to maintain their central role in the ecosystem.
5. How might the Inflation Reduction Act (IRA) and its drug price negotiation provisions impact the dynamics of the 90-day supply?
The IRA’s price negotiation provisions could have complex, indirect effects. By allowing Medicare to negotiate the price of high-cost drugs, the IRA will lower the “net price” that manufacturers receive for some of their biggest products. This could reduce the size of the “gross-to-net bubble” and, consequently, the dollar value of the rebates that manufacturers can offer to PBMs. If the financial incentive from rebates is diminished, PBMs might have less motivation to aggressively steer patients to certain high-rebate brand-name drugs via 90-day mail-order mandates. This could slightly weaken one of the key economic forces supporting the rigid 90-day standard, potentially opening the door for more flexibility in dispensing, though the PBMs’ other incentives for promoting 90-day fills (e.g., operational efficiency, administrative fees) would remain.
References
- The 92-Day Pill Puzzle: Why Your 3-Month Supply Doesn’t Add Up …, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/the-92-day-pill-puzzle-why-your-3-month-supply-doesnt-add-up/
- The History of Pharmacy | Texas Tech University Health Sciences Center, accessed August 4, 2025, https://www.ttuhsc.edu/pharmacy/museum/pharmacy.history.aspx
- History of pharmacy in the United States – Wikipedia, accessed August 4, 2025, https://en.wikipedia.org/wiki/History_of_pharmacy_in_the_United_States
- Preparing and Dispensing Prescriptions during the Civil War Era – American Institute of the History of Pharmacy, accessed August 4, 2025, https://aihp.org/wp-content/uploads/2017/07/AC10.pdf
- History of PSSNY – Pharmacists Society of the State of New York, accessed August 4, 2025, https://www.pssny.org/page/History/History-of-PSSNY.htm
- Understanding Billing Cycle in Medical Billing – EZ Settle Solutions, accessed August 4, 2025, https://ezsettlesolutions.com/what-is-billing-cycle-in-medical-billing/
- DEA to Allow 90-Day Supply of Schedule II Drugs | Psychiatric News – Psychiatry Online, accessed August 4, 2025, https://psychiatryonline.org/doi/full/10.1176/pn.43.1.0002
- Medication Days’ Supply, Adherence, Wastage, and Cost Among Chronic Patients in Medicaid – CMS, accessed August 4, 2025, https://www.cms.gov/mmrr/Downloads/MMRR2012_002_03_A04.pdf
- Myth or fact? Rx durations are limited to 90 days plus 1 refill | American Medical Association, accessed August 4, 2025, https://www.ama-assn.org/practice-management/sustainability/myth-or-fact-rx-durations-are-limited-90-days-plus-1-refill
- Examining Medicare Part D Policies for Extended Supplies of … – KFF, accessed August 4, 2025, https://www.kff.org/coronavirus-covid-19/issue-brief/examining-medicare-part-d-policies-for-extended-supplies-of-medication/
- PBM Basics – Pharmacists Society of the State of New York, accessed August 4, 2025, https://www.pssny.org/page/PBMBasics
- Pharmacy benefit management – Wikipedia, accessed August 4, 2025, https://en.wikipedia.org/wiki/Pharmacy_benefit_management
- The Top Pharmacy Benefit Managers of 2024: Market Share and Key Industry Developments – Drug Channels, accessed August 4, 2025, https://www.drugchannels.net/2025/03/the-top-pharmacy-benefit-managers-of.html
- PBMs, Formularies, and Rebates: What Investors Should Know …, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/pbms-formularies-and-rebates-what-investors-should-know/
- What Pharmacy Benefit Managers Do, and How They Contribute to Drug Spending, accessed August 4, 2025, https://www.commonwealthfund.org/publications/explainer/2025/mar/what-pharmacy-benefit-managers-do-how-they-contribute-drug-spending
- Three ways PBMs Make Money: Rebates, Admin Fees and Spread – AffirmedRx, accessed August 4, 2025, https://affirmedrx.com/how-pbms-make-money/
- How PBMs Make Money: PBM Practices & Profits – [Infographic], accessed August 4, 2025, https://info.rxsafe.com/blog/pbms-make-money-infographic
- What is a PBM Admin Fee? – SmithRx, accessed August 4, 2025, https://smithrx.com/blog/what-is-a-pbm-admin-fee
- PBM Rebates Explained: How They Work and What to Know – Xevant, accessed August 4, 2025, https://www.xevant.com/blog/pbm-rebates-explained/
- PBM Power: The Gross-to-Net Bubble Reached $334 Billion in 2023—But Will Soon Start Deflating – Drug Channels, accessed August 4, 2025, https://www.drugchannels.net/2024/07/pbm-power-gross-to-net-bubble-reached.html
- 5 Things To Know About Pharmacy Benefit Managers – Center for American Progress, accessed August 4, 2025, https://www.americanprogress.org/article/5-things-to-know-about-pharmacy-benefit-managers/
- Texas Pharmacy Coverage | Ambetter from Superior HealthPlan, accessed August 4, 2025, https://www.ambetterhealth.com/en/tx/resources/pharmacy-resources/
- Getting Started With Mail Order Prescriptions | CenterWell Pharmacy®, accessed August 4, 2025, https://www.centerwellpharmacy.com/how-mail-order-prescription-works.html
- Mail Order Pharmacy Delivery – CVS Health, accessed August 4, 2025, https://www.cvshealth.com/services/pharmacy/mail-order-pharmacy.html
- Home Delivery | Express Scripts® Pharmacy, accessed August 4, 2025, https://www.express-scripts.com/rx
- Mail Order Pharmacy | New Hampshire Medicaid – WellSense Health Plan, accessed August 4, 2025, https://www.wellsense.org/members/nh/new-hampshire-medicaid/prescriptions/mail-order-pharmacy
- The Role of Pharmacy Benefit Managers in Prescription Drug Markets – House Oversight Committee, accessed August 4, 2025, https://oversight.house.gov/wp-content/uploads/2024/07/PBM-Report-FINAL-with-Redactions.pdf
- Why 90 day prescriptions? : r/pharmacy – Reddit, accessed August 4, 2025, https://www.reddit.com/r/pharmacy/comments/1afgg1f/why_90_day_prescriptions/
- One Less Errand, One Healthier Member: The Power of 90-Day Prescriptions, accessed August 4, 2025, https://www.premisehealth.com/resources/blog/one-less-errand-one-healthier-member-the-power-of-90-day-prescriptions/
- 90-day prescription fills benefit your employees – Wellmark, accessed August 4, 2025, https://www.wellmark.com/blue-at-work/insights/90-day-prescription-refills
- Medicare Beneficiaries Achieve Greater Medication Adherence with Home Delivery 90-Day Prescriptions – UnitedHealth Group, accessed August 4, 2025, https://www.unitedhealthgroup.com/content/dam/UHG/PDF/2024/2024-01-orx-home-delivery-clinical-value-medicare.pdf
- Difference in Medication Adherence Between Patients Prescribed a 30-Day Versus 90-Day Supply After Acute Myocardial Infarction, accessed August 4, 2025, https://www.ahajournals.org/doi/pdf/10.1161/JAHA.119.016215
- Intentional Overdose Prevention in the Era of the 90-Day Prescription | Psychiatric Services, accessed August 4, 2025, https://psychiatryonline.org/doi/10.1176/appi.ps.202100050
- Reducing Patient Access to Lethal Quantities of Medication, accessed August 4, 2025, https://www.psychiatry.org/getmedia/46fec838-56eb-4880-a756-08deaefdba50/90-Day-Prescribing-Factsheet.pdf
- REMINDER: NYRx allows 90-day Prescribing for Most Maintenance Medications and OTC Drugs – eMedNY, accessed August 4, 2025, https://www.emedny.org/ProviderManuals/communications/NYRx_Allows_90_Day_Prescribing.pdf
- COUNCIL ON MEDICAL SERVICE, accessed August 4, 2025, https://www.ama-assn.org/system/files/a23-cms05.pdf
- Patient Access To Minnesota Pharmacy Services In Peril, accessed August 4, 2025, https://www.house.mn.gov/comm/docs/ERWvP29OlEG5kStvAom4tQ.pdf
- PBMs concentrate market share across the nation: AMA – Medical Economics, accessed August 4, 2025, https://www.medicaleconomics.com/view/pbms-concentrate-market-share-across-the-nation-ama
- A brief look at current debates about pharmacy benefit managers – Brookings Institution, accessed August 4, 2025, https://www.brookings.edu/articles/a-brief-look-at-current-debates-about-pharmacy-benefit-managers/
- The End of Exclusivity: Navigating the Drug Patent Cliff for …, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/the-impact-of-drug-patent-expiration-financial-implications-lifecycle-strategies-and-market-transformations/
- The Physician and Administrator-Reported Cost of Drug Utilization Management to Physician Practices: A Cross-Sectional Survey – PMC – PubMed Central, accessed August 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9308474/
- Combatting Pharmacist Burnout: Alleviating Administrative Burden | – SpinSci, accessed August 4, 2025, https://spinsci.com/blog/combatting-pharmacist-burnout-alleviating-administrative-burden/
- A systematic review and pooled prevalence of burnout in pharmacists – PubMed Central, accessed August 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9707850/
- Addressing Pharmacist Burnout and Staffing Shortages: A Review of Challenges and Solutions – IJFMR, accessed August 4, 2025, https://www.ijfmr.com/papers/2024/2/38294.pdf
- Special report: the stressors burning out pharmacists – The Pharmaceutical Journal, accessed August 4, 2025, https://pharmaceutical-journal.com/article/feature/special-report-the-stressors-burning-out-pharmacists
- Medication Synchronization Resource Guide – ASHP, accessed August 4, 2025, https://www.ashp.org/-/media/assets/pharmacy-practice/resource-centers/patient-safety/ASHP-Medication-Synchronization-Resource-Guide.pdf
- The Impact of a Medication Synchronization Program on Adherence and Patient Satisfaction, accessed August 4, 2025, https://www.pharmacytimes.com/view/the-impact-of-a-medication-synchronization-program-on-adherence-and-patient-satisfaction/1000
- Medication Synchronization Programs Improve Adherence To Cardiovascular Medications And Health Care Use | Health Affairs, accessed August 4, 2025, https://www.healthaffairs.org/doi/10.1377/hlthaff.2017.0881
- Medication Nonadherence Increases Health Costs, Hospital Readmissions, accessed August 4, 2025, https://physicians.dukehealth.org/articles/medication-nonadherence-increases-health-costs-hospital-readmissions
- New Study Reports Non-Optimized Medication Therapy Costs $528.4 Billion Annually, accessed August 4, 2025, https://naspa.us/2018/04/06/new-study-reports-non-optimized-medication-therapy-costs-528-4-billion-annually/
- Difference in Medication Adherence Between Patients Prescribed a 30‐Day Versus 90‐Day Supply After Acute Myocardial Infarction, accessed August 4, 2025, https://www.ahajournals.org/doi/10.1161/JAHA.119.016215
- Difference in Medication Adherence Between Patients Prescribed a 30‐Day Versus 90‐Day Supply After Acute Myocardial Infarction, accessed August 4, 2025, https://www.ahajournals.org/doi/abs/10.1161/JAHA.119.016215
- Difference in Medication Adherence Between Patients Prescribed a 30-Day Versus 90-Day Supply After Acute Myocardial Infarction – PubMed, accessed August 4, 2025, https://pubmed.ncbi.nlm.nih.gov/33342227/
- Your Stories | TruthinRx, accessed August 4, 2025, https://truthinrx.org/your-stories
- 90% of Pain Patients Have Trouble Filling Opioid Prescriptions, accessed August 4, 2025, https://www.painnewsnetwork.org/stories/2024/1/11/nbsp-90-of-us-pain-patients-have-trouble-filling-opioid-prescriptions
- What is a patent cliff, and how does it impact companies? – Patsnap Synapse, accessed August 4, 2025, https://synapse.patsnap.com/article/what-is-a-patent-cliff-and-how-does-it-impact-companies
- After a year on the market, Humira biosimilars aren’t making much of a dent, accessed August 4, 2025, https://www.healthcare-brew.com/stories/2024/01/29/after-a-year-on-the-market-humira-biosimilars-aren-t-making-much-of-a-dent
- Two decades and $200 billion: AbbVie’s Humira monopoly nears its end | BioPharma Dive, accessed August 4, 2025, https://www.biopharmadive.com/news/humira-abbvie-biosimilar-competition-monopoly/620516/
- 5 Steps to Take When Your Drug Patent is About to Expire, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/5-steps-to-take-when-your-drug-patent-is-about-to-expire/
- Patent protection strategies – PMC, accessed August 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3146086/
- Top Strategies for Pharma Profitability after Drug Patents Expire – DrugPatentWatch, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/top-strategies-for-pharma-profitability-after-drug-patents-expire/
- Navigating pharma loss of exclusivity | EY – US, accessed August 4, 2025, https://www.ey.com/en_us/insights/life-sciences/navigating-pharma-loss-of-exclusivity
- AdhereTech: Medication Adherence Solutions for Better Health, accessed August 4, 2025, https://adheretech.com/
- Medication Adherence Technology – Altruix, accessed August 4, 2025, https://altruix.com/medherent-medication-adherence-technology/
- CoverMyMeds: Healthcare technology solutions, accessed August 4, 2025, https://covermymeds.health/
- Veradigm® | Data-driven Healthcare Solutions & Insights, accessed August 4, 2025, https://veradigm.com/
- AdhereHealth | Industry Leading Technology Company, accessed August 4, 2025, https://adherehealth.com/
- Prescription Drug Pricing Transparency Law Comparison Chart – NASHP, accessed August 4, 2025, https://nashp.org/state-tracker/prescription-drug-pricing-transparency-law-comparison-chart/
- Prescription Quantity Limits: What to Do When Insurance Coverage Is Restricted – GoodRx, accessed August 4, 2025, https://www.goodrx.com/insurance/health-insurance/prescription-quantity-limits-insurance-plans-limit-coverage
- Pharmacy – Mississippi Division of Medicaid – | MS.GOV, accessed August 4, 2025, https://medicaid.ms.gov/pharmacy/
- Medicare Prescription Drug Benefit Manual – Chapter 6 – Part D Drugs and Formulary Requirements – CMS, accessed August 4, 2025, https://www.cms.gov/medicare/prescription-drug-coverage/prescriptiondrugcovcontra/downloads/part-d-benefits-manual-chapter-6.pdf
- Phases of Part D coverage – Medicare Interactive, accessed August 4, 2025, https://www.medicareinteractive.org/understanding-medicare/medicare-prescription-drug-coverage-part-d/medicare-part-d-costs/phases-of-part-d-coverage
- Premium payments, grace periods, & losing coverage | HealthCare.gov, accessed August 4, 2025, https://www.healthcare.gov/apply-and-enroll/health-insurance-grace-period/
- Navigating Short-Cycle Billing | ComputerTalk For The Pharmacist, accessed August 4, 2025, https://www.computertalk.com/navigating-short-cycle-billing/
- Medicare Prescription Payment Plan Part 1 Guidance – CMS, accessed August 4, 2025, https://www.cms.gov/files/document/medicare-prescription-payment-plan-part-1-guidance.pdf
- ASHP Early Years, accessed August 4, 2025, https://www.ashp.org/About-ASHP/our-history/ASHP-Early-Years
- Mail Service Pharmacy – Walgreens, accessed August 4, 2025, https://www.walgreens.com/rx-settings/home-delivery-pharmacy
- Is a 90-Day Supply the Best Option to Improve Medication Adherence? – Pharmacy Times, accessed August 4, 2025, https://www.pharmacytimes.com/view/is-a-90-day-supply-the-best-option-to-improve-medication-adherence-
- Expanding Access to Patient Care and Ensuring Community Pharmacy Continuity of Operations, accessed August 4, 2025, https://www.nacds.org/pdfs/pharmacy/2020/COVID-19-RecommendedPriorities-State%20ExecutiveOrdersforDeclaredEmergency-final.pdf
- lawbook.pdf – California State Board of Pharmacy, accessed August 4, 2025, https://www.pharmacy.ca.gov/laws_regs/lawbook.pdf
- www.commonwealthfund.org, accessed August 4, 2025, https://www.commonwealthfund.org/publications/explainer/2025/mar/what-pharmacy-benefit-managers-do-how-they-contribute-drug-spending#:~:text=PBMs%20also%20derive%20revenue%20in,business%20to%20their%20affiliated%20pharmacies.
- A primer on prescription drug rebates: Insights into why rebates are a target for reducing prices – Milliman, accessed August 4, 2025, https://www.milliman.com/en/insight/a-primer-on-prescription-drug-rebates-insights-into-why-rebates-are-a-target-for-reducing
- Pharmacy Benefit Managers: The Powerful Middlemen Inflating Drug Costs and Squeezing Main Street Pharmacies – Federal Trade Commission, accessed August 4, 2025, https://www.ftc.gov/system/files/ftc_gov/pdf/pharmacy-benefit-managers-staff-report.pdf
- How Large PBMs Make Money Today: A 2025 Drug Channels Update, accessed August 4, 2025, https://www.drugchannels.net/2025/05/how-large-pbms-make-money-today-2025.html
- Payers’ PBMs ranked by market share, accessed August 4, 2025, https://www.beckerspayer.com/payer/payers-pbms-ranked-by-market-share/
- How the Big 3 PBMs Utilize Various Market Strategies – Drug Topics, accessed August 4, 2025, https://www.drugtopics.com/view/how-the-big-3-pbms-utilize-various-market-strategies
- Top PBMs by 2024 market share – Becker’s Hospital Review | Healthcare News & Analysis, accessed August 4, 2025, https://www.beckershospitalreview.com/pharmacy/top-pbms-by-2024-market-share/
- The golden era of biosimilars: patent expiration wave and their impact on global healthcare, accessed August 4, 2025, https://mabxience.com/the-golden-era-of-biosimilars-patent-expiration-wave-and-their-impact-on-global-healthcare/
- 5 Pharma Powerhouses Facing Massive Patent Cliffs—And What They’re Doing About It, accessed August 4, 2025, https://www.biospace.com/business/5-pharma-powerhouses-facing-massive-patent-cliffs-and-what-theyre-doing-about-it
- Biopharma’s Patent Cliff Puts Costs Front and Center – Boston Consulting Group, accessed August 4, 2025, https://www.bcg.com/publications/2025/patent-cliff-threatens-biopharmaceutical-revenue
- An Analysis on leveraging the patent cliff with drug sales worth USD 251 billion going off-patent and analysis of different drug – Department of Pharmaceuticals, accessed August 4, 2025, https://pharma-dept.gov.in/sites/default/files/FINAL-An%20analysis%20on%20leveraging%20the%20patent%20cliff.pdf
- Surviving patent expiration: strategies for marketing pharmaceutical products | Emerald Insight, accessed August 4, 2025, https://www.emerald.com/insight/content/doi/10.1108/10610429710179471/full/html
- Drug patents with formulation changes : r/pharmacy – Reddit, accessed August 4, 2025, https://www.reddit.com/r/pharmacy/comments/16dyv15/drug_patents_with_formulation_changes/
- Big Pharma Prepares for ‘Patent Cliff’ as Blockbuster Drug Revenue Losses Loom, accessed August 4, 2025, https://www.tradeandindustrydev.com/industry/bio-pharmaceuticals/big-pharma-prepares-patent-cliff-blockbuster-drug-34694
- The $400 Billion Patent Cliff: Big Pharma’s Revenue Crisis – The American Bazaar, accessed August 4, 2025, https://americanbazaaronline.com/2025/08/04/the-400-billion-patent-cliff-big-pharmas-revenue-crisis-465788/
- Drug Competition Series: Analysis of New Generic Markets Effect of Market Entry on Generic Drug Prices: Medicare Data 2007-2022 – HHS ASPE, accessed August 4, 2025, https://aspe.hhs.gov/reports/analysis-new-generic-markets-effect-market-entry-generic-drug-prices
- Durbin Delivers Opening Statement In Senate Judiciary Committee Hearing On Pharmacy Benefit Managers, accessed August 4, 2025, https://www.judiciary.senate.gov/press/dem/releases/durbin-delivers-opening-statement-in-senate-judiciary-committee-hearing-on-pharmacy-benefit-managers
- Prescription Drug Costs | Pros, Cons, Debate, Arguments, Economy, Laws, Government, & Regulation | Britannica, accessed August 4, 2025, https://www.britannica.com/procon/prescription-drug-costs-debate
- The Value of Pharmacy Benefit Management – Becker Friedman Institute for Economics, accessed August 4, 2025, https://bfi.uchicago.edu/wp-content/uploads/2022/07/BFI_WP_2022-93.pdf
- The Multi-Billion Dollar Countdown: Decoding the Patent Cliff and Seizing the Generic Opportunity – DrugPatentWatch, accessed August 4, 2025, https://www.drugpatentwatch.com/blog/patent-expirations-seizing-opportunities-in-the-generic-drug-market/
- Global pharmaceutical companies are under immense pressure: in the coming years, a “patent expiration wave” is approaching, and companies are now turning their attention to China in search of acquisition symbols., accessed August 4, 2025, https://news.futunn.com/en/post/58939207/global-pharmaceutical-companies-are-under-immense-pressure-in-the-coming
- Navigating the Patent Cliff: Precision Print Campaigns for Pharma’s Evolving Landscape – RxJam, accessed August 4, 2025, https://rxjam.com/blog/navigating-the-patent-cliff-precision-print-campaigns-for-pharmas-evolving-landscape/
- About Us – Patients For Affordable Drugs, accessed August 4, 2025, https://www.patientsforaffordabledrugs.org/about-us/
- PAN Foundation – Patient financial assistance, advocacy, and education, accessed August 4, 2025, https://www.panfoundation.org/
- Advocacy | Association for Accessible Medicines, accessed August 4, 2025, https://accessiblemeds.org/advocacy/
- Drug Pricing – ASHP, accessed August 4, 2025, https://www.ashp.org/Advocacy-and-Issues/Key-Issues/Drug-Pricing
- The impact of a retail prescription synchronization program on medication adherence – Harvard University, accessed August 4, 2025, https://scholar.harvard.edu/files/nkc/files/2017_the_impact_of_a_retail_prescription_sync_j_am_pharm_assoc.pdf
- Federal Regulation of Medication Dispensing – StatPearls – NCBI Bookshelf, accessed August 4, 2025, https://www.ncbi.nlm.nih.gov/books/NBK582130/
- Drug Supply Chain Security Act (DSCSA) – FDA, accessed August 4, 2025, https://www.fda.gov/drugs/drug-supply-chain-integrity/drug-supply-chain-security-act-dscsa
- E-Prescribing Standards and Requirements – CMS, accessed August 4, 2025, https://www.cms.gov/medicare/regulations-guidance/electronic-prescribing/adopted-standard-and-transactions
- House passes Borowski bill to simplify electronic prescription transfers between pharmacies & align with federal standards, accessed August 4, 2025, https://www.pahouse.com/InTheNews/NewsRelease/?id=137762
- Prescription Requirement Under Section 503A of the Federal Food, Drug, and Cosmetic Act Guidance for Industry | FDA, accessed August 4, 2025, https://www.fda.gov/files/drugs/published/Prescription-Requirement-Under-Section-503A-of-the-Federal-Food–Drug–and-Cosmetic-Act-Guidance-for-Industry.pdf
- UpToDate: Trusted, evidence-based solutions for modern healthcare – Wolters Kluwer, accessed August 4, 2025, https://www.wolterskluwer.com/en/solutions/uptodate
- Mobile and Home Health Tech Solutions – IQVIA, accessed August 4, 2025, https://www.iqvia.com/locations/middle-east-and-africa/solutions/provider-solutions/mobile-and-home-health-tech-solutions
- 30-5-35. Conversion of prescriptions authorizing refills. – West Virginia Code, accessed August 4, 2025, https://code.wvlegislature.gov/30-5-35/
- The Role of Pharmacy Benefit Managers and Skyrocketing Cost of Medications – PMC, accessed August 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11482839/
- Recent Trends in the Dispensing of 90-Day-Supply Prescriptions at Retail Pharmacies: Implications for Improved Convenience and Access – PubMed Central, accessed August 4, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4106580/
- The Use of Medicines in the U.S. 2023 – IQVIA, accessed August 4, 2025, https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/the-use-of-medicines-in-the-us-2023
- Average Administrative Cost for Prescriptions – Community Care – VA.gov, accessed August 4, 2025, https://www.va.gov/COMMUNITYCARE/revenue-ops/admin-costs.asp
- Management of Prescription Refills in Primary Care: An Oklahoma Physicians Resource/Research Network (OKPRN) Study, accessed August 4, 2025, https://www.jabfm.org/content/jabfp/19/1/31.full.pdf
- The top 15 blockbuster patent expirations coming this decade – Fierce Pharma, accessed August 4, 2025, https://www.fiercepharma.com/special-report/top-15-blockbuster-patent-expirations-coming-decade
- Recent Study Finds Appointment-based Medication Synchronization Programs Make Patients 3X More Likely to be Adherent – EnlivenHealth, accessed August 4, 2025, https://enlivenhealth.co/blog/recent-study-finds-appointment-based-medication-synchronization-programs-make-patients-3x-more-likely-to-be-adherent/
- Massachusetts law about prescription medication | Mass.gov, accessed August 4, 2025, https://www.mass.gov/info-details/massachusetts-law-about-prescription-medication
- 2024 Bills Impacting Health Care Professions – Florida Board of Pharmacy, accessed August 4, 2025, https://floridaspharmacy.gov/new-legislation-impacting-your-profession-2024-2/
- NeedyMeds, accessed August 4, 2025, https://www.needymeds.org/
- Our search for a reliable patent intelligence solution ended with …, accessed August 4, 2025, https://www.drugpatentwatch.com/