In the complex ecosystem of modern healthcare, few challenges loom as large and as persistently as the relentless rise of prescription drug prices. It’s a high-stakes game where the rules are constantly shifting, and the health of millions hangs in the balance. For healthcare systems—from sprawling hospital networks to small, independent clinics—this isn’t just an abstract economic problem. It’s a tangible, day-to-day struggle that directly impacts their ability to deliver quality care, manage their budgets, and, ultimately, protect their patients. The cost of a single groundbreaking therapy can cripple a hospital’s annual budget, while incremental price hikes on hundreds of essential medications act like a slow, crushing tide. How, then, are these systems navigating this treacherous terrain?
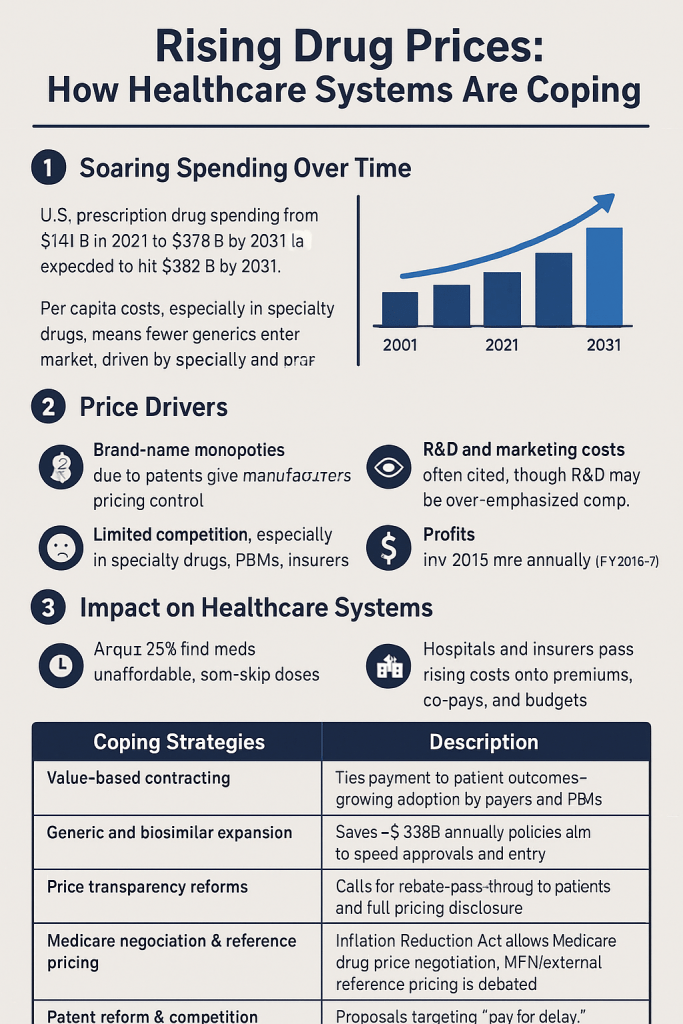
This is not a new problem, but its scale and complexity have reached unprecedented levels. Consider the median annual price for a new drug, which soared to $300,000 in 2023, a staggering 35% increase from the prior year [1]. Such figures are not outliers; they are becoming the norm, driven by an influx of high-cost specialty drugs, gene therapies, and biologics that offer life-changing potential but come with a prohibitive price tag. The question for every healthcare executive, every pharmacist, and every clinician is no longer “if” drug prices will impact their operations, but “how significantly?” and “what can we do about it?”
The Multi-Faceted Impact of Escalating Drug Costs
The repercussions of rising drug prices ripple through the entire healthcare system, affecting every stakeholder from the patient at the pharmacy counter to the CFO in the C-suite. It’s a domino effect, where a price increase in one area creates pressure, and sometimes crisis, in another.
1. Budgetary Strain and Operational Challenges
For hospitals and health systems, prescription drugs represent a major and volatile expense. Unlike other operational costs that can be predicted with relative stability, drug spending is subject to rapid, significant increases. A 2017 study by the New Jersey Hospital Association found that hospital drug spending more than doubled between 2008 and 2017, outstripping the growth of total hospital expenses [2].
This financial pressure forces difficult trade-offs. To absorb the costs, hospitals may have to delay critical infrastructure investments, cut staffing levels, or reduce the scope of services they offer [3]. This isn’t just about financial health; it’s about the very capacity of the system to function. The budget that could have funded a new MRI machine or hired more nurses is instead being diverted to an exorbitant cancer drug.
2. The Patient’s Burden: A Crisis of Adherence
Perhaps the most tragic consequence of high drug prices is the direct impact on patients. When out-of-pocket costs become insurmountable, patients are often forced to make impossible choices. Do I pay for my medication, or do I pay my rent? Do I take my full dose, or do I stretch it out to make the prescription last longer? A Kaiser Family Foundation survey found that one in four Americans taking prescription drugs reports difficulty affording their medication [3]. This leads to a dangerous decline in medication adherence, which can result in worsening health conditions, emergency room visits, and hospitalizations—ultimately increasing the overall cost of care. The system pays the price, but the patient endures the suffering.
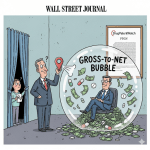
3. The Supply Chain Squeeze: Navigating a Labyrinth of Middlemen
The journey of a drug from the manufacturer to the patient is not a straight line. It’s a complex, often opaque, supply chain involving wholesalers, pharmacy benefit managers (PBMs), and insurers. This labyrinth contributes to the high list prices of drugs, as rebates and discounts are negotiated in a secretive process known as the “gross-to-net bubble.” As one report from the U.S. Department of Labor highlighted, “For many drugs, however, list prices are not the prices ultimately paid to manufacturers; payers or pharmacy benefit managers (PBMs) negotiate with manufacturers over formulary placement in exchange for discounts in the form of reb1ates off the list price” [4]. This lack of transparency makes it difficult for healthcare systems and patients to understand the true cost of a medication.
Proactive Strategies: Taking Control of the Narrative
Instead of passively accepting rising costs, healthcare systems are adopting a portfolio of proactive and innovative strategies to regain control. This is where innovation meets necessity, and where data-driven insights become a powerful weapon.
1. Strategic Formulary Management
The formulary—the list of drugs a health system or insurer covers—is a powerful tool. By strategically managing it, systems can incentivize the use of lower-cost, clinically effective alternatives. This involves:
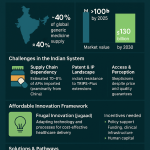
- Promoting Generic and Biosimilar Adoption: When a brand-name drug loses its patent exclusivity, generic versions can enter the market at a fraction of the cost [5]. Similarly, biosimilars—near-identical versions of complex biologic drugs—provide a competitive alternative. Healthcare systems are aggressively promoting the use of these alternatives through physician education, tiered copay structures, and pharmacy-level substitution programs.
- Tiered Formularies: By placing drugs into different tiers with varying copayment levels, health plans can encourage patients and physicians to choose more affordable options. For example, a generic drug might be in Tier 1 with a low copay, while a high-cost brand name drug is in Tier 3 with a high copay.
- Value-Based Formulary Design: Moving beyond simple cost, some health systems are designing formularies based on a drug’s clinical value. This means a new, high-cost therapy will only be covered if it demonstrably provides better patient outcomes than existing, less expensive options.
2. Leveraging Data and Analytics for Insight
In the battle against rising costs, knowledge is power. Healthcare systems are turning to sophisticated data analytics to identify spending trends, predict future costs, and pinpoint opportunities for savings.
- Predictive Cost Modeling: By analyzing historical purchasing data, systems can predict which drug classes are likely to drive future cost increases. This allows them to proactively negotiate contracts or seek alternative sourcing.
- Patient-Level Spend Analysis: Digging into de-identified patient data can reveal patterns of non-adherence driven by cost. For example, if a patient with a chronic condition consistently fails to refill an expensive prescription, it’s a clear signal that a different, more affordable solution is needed.
- Competitive Intelligence from Patent Data: This is where a resource like DrugPatentWatch becomes invaluable. By tracking patent expiration dates and litigation outcomes, a health system can anticipate the entry of generic and biosimilar competitors. This intelligence allows them to prepare for new, lower-cost options and gain leverage in negotiations with brand-name manufacturers. A system that knows exactly when a key drug’s patent is set to expire is a system prepared to save millions.
3. Innovative Payment and Purchasing Models
The traditional fee-for-service model is ill-equipped to handle the financial volatility of modern drug pricing. As a result, healthcare systems are exploring and implementing groundbreaking payment and purchasing models.
- Value-Based Pricing and Contracting: This model ties the payment for a drug to its actual performance in patients. For example, a manufacturer of a diabetes drug might agree to a contract where they receive full payment only if the patient achieves a certain A1c level. This shifts the risk from the payer to the manufacturer and aligns incentives around patient outcomes, not just product volume.
- The “Netflix Model” or Subscription-Based Pricing: Pioneered in Louisiana for hepatitis C treatments, this model involves a state or health system paying a flat fee for unlimited access to a specific drug for a set population [6]. This provides budget predictability for the payer and ensures all patients who need the treatment can get it, without the prohibitive per-unit cost.
- Group Purchasing Organizations (GPOs): GPOs are consortiums that leverage the collective purchasing power of multiple hospitals and health systems to negotiate better prices with drug manufacturers and distributors. By pooling their volume, they can secure discounts that would be impossible for a single institution to obtain.
4. Policy and Advocacy: Changing the Rules of the Game
The root of the problem lies in the broader policy landscape. Healthcare systems are not just reacting; they are actively engaging in advocacy to push for systemic change.
- Negotiating Power: The Inflation Reduction Act (IRA) of 2022 gave Medicare the power to negotiate prices for certain high-cost drugs, a historic shift that could have ripple effects throughout the market. Healthcare systems are lobbying to expand these negotiation powers to a broader range of drugs and payers [7].
- Tackling Patent Abuse: Pharmaceutical companies often employ strategies to extend their patent exclusivity, a practice known as “evergreening.” They may file for new patents on minor modifications to a drug (e.g., a new dosage form), effectively delaying generic competition. Advocacy groups and policymakers are increasingly targeting these tactics, with a recent study finding that “anti-competitive patent abuse tactics used by big pharmaceutical companies cost U.S. consumers an additional $40.7 billion in prescription drug expenses in one year alone” [8].
- Enhancing Transparency: Healthcare systems are pushing for legislation that would require greater transparency in the drug supply chain, particularly regarding the rebates and fees charged by PBMs.
“The relentless rise in prescription drug prices is not just a financial challenge; it is a public health crisis. It forces patients to choose between their health and their financial security, and it strains the very foundation of our healthcare system, jeopardizing access to quality care for all.”— Rick Pollack, President and CEO, American Hospital Association [3]
The Role of Technology and the Future of Drug Cost Management
As healthcare systems look to the horizon, technology and data will be their most powerful allies. The future of drug cost management is not just about negotiation, but about a holistic, integrated approach.
- AI and Machine Learning: Algorithms can analyze vast datasets to identify pricing anomalies, predict market changes, and even optimize formulary design in real-time based on patient population needs and market dynamics.
- Electronic Health Record (EHR) Integration: Integrating drug cost data directly into the EHR at the point of prescribing can empower physicians to make more cost-conscious decisions without compromising clinical efficacy. A doctor could see an alert for a lower-cost generic or a more affordable alternative within the patient’s insurance formulary, right as they write the prescription.
- Enhanced Patient Engagement Platforms: These platforms can provide patients with clear, easy-to-understand information about their drug costs, discount programs, and patient assistance options, empowering them to become active participants in managing their own healthcare expenses.
Key Takeaways
- Rising drug prices are a major threat to healthcare systems’ financial stability and a significant barrier to patient care. The median price for new drugs is increasing at an alarming rate, and existing drugs often see price hikes that outpace inflation.
- The impact is felt throughout the system: from strained hospital budgets and delayed capital investments to reduced patient adherence and worsening health outcomes.
- Healthcare systems are fighting back with a mix of strategies. These include strategic formulary management (prioritizing generics and biosimilars), leveraging data and analytics for competitive intelligence and predictive modeling, and adopting innovative payment models like value-based contracting and subscription models.
- Policy and advocacy are crucial. Systems are working to reform the broader ecosystem by advocating for greater drug price negotiation powers for Medicare, tackling anti-competitive patent abuse, and demanding more transparency in the supply chain.
- Technology will be the key to the future. Tools like AI, EHR integration, and patient engagement platforms will provide the data and insights needed to make informed decisions and manage costs more effectively. The battle against rising drug prices is a long and arduous one, but with strategic action and a commitment to innovation, healthcare systems can protect their patients and secure a more sustainable future.
FAQ Section
1. What is the difference between a generic drug and a biosimilar, and why are they important for cost control?
A generic drug is a chemically identical copy of a small-molecule, brand-name drug whose patent has expired. It must contain the same active ingredient and be proven to be bioequivalent, meaning it works the same way in the body. A biosimilar is a highly similar, but not identical, version of a complex biologic drug. Because biologics are derived from living organisms, an exact copy is impossible, but biosimilars must be proven to have no clinically meaningful differences from the original. Both generics and biosimilars are crucial for cost control because they introduce competition to the market, which typically drives down the price of both the original brand-name product and the new competitors.
2. How do pharmacy benefit managers (PBMs) affect drug prices for healthcare systems?
PBMs are intermediaries that manage prescription drug benefits for insurers and health plans. They negotiate rebates with drug manufacturers in exchange for including a drug on their formulary. While PBMs argue that these rebates save money for health plans, critics point to the lack of transparency in this process. The difference between the price the PBM negotiates with the manufacturer and the price the PBM charges the health plan (known as the “spread”) can be significant. This lack of transparency and the complex rebate system can contribute to high list prices and make it difficult for healthcare systems to understand and control their true drug costs.
3. What is “evergreening,” and why is it a concern?
“Evergreening” refers to a pharmaceutical company’s strategy to extend the patent exclusivity of a brand-name drug beyond its original term. This is often done by filing for new patents on minor changes, such as a new formulation, dosage, or method of delivery. By securing these new patents, the company can block or delay the entry of generic competitors, thereby maintaining its monopoly and high pricing for an extended period. This practice is a major concern for healthcare systems and policymakers because it stifles competition and keeps drug costs artificially high.
4. Can technology alone solve the problem of rising drug costs?
No, technology is a powerful tool, but it is not a silver bullet. While data analytics and AI can provide invaluable insights for strategic decision-making and operational efficiency, they cannot change the fundamental market dynamics, patent laws, or regulatory frameworks that drive high prices. The successful management of drug costs requires a multi-pronged approach that combines technological innovation with strategic negotiation, proactive policy advocacy, and a commitment to transparency across the entire healthcare ecosystem.
5. How do a health system’s actions on drug pricing impact patients?
A health system’s strategies to manage drug costs directly and significantly impact patient care. When a system successfully negotiates lower drug prices, those savings can be passed on to patients through lower copays and premiums, improving medication adherence and health outcomes. Conversely, a system that fails to manage costs may be forced to raise patient costs, limit access to certain medications, or reduce other services, leading to poorer health outcomes. The choices health systems make in this arena are a direct reflection of their commitment to patient well-being.
References
[1] AHA News. (2024, May 22). Drug Prices and Shortages Jeopardize Patient Access to Quality Hospital Care. Retrieved from https://www.aha.org/news/blog/2024-05-22-drug-prices-and-shortages-jeopardize-patient-access-quality-hospital-care
[2] New Jersey Hospital Association. (2019). Rising Drug Costs Are Handcuffing Healthcare. Retrieved from https://www.njha.com/media/548875/CHART-Bulletin-Drug-Costs.pdf
[3] American Hospital Association. (2019, January 15). New Report Shows Impact of Rising Drug Prices and Drug Shortages on Patients and Hospitals. Retrieved from https://www.aha.org/press-releases/2019-01-15-new-report-shows-impact-rising-drug-prices-and-drug-shortages-patients
[4] U.S. Department of Labor. (2024). Prescription Drug Spending, Pricing Trends, and Premiums in Private Health Insurance Plans. Retrieved from https://www.dol.gov/sites/dolgov/files/ebsa/laws-and-regulations/laws/no-surprises-act/2024-report-to-congress-prescription-drug-spending.pdf
[5] NCBI Bookshelf. (2017). Factors Influencing Affordability. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK493090/
[6] Schaeffer Center for Health Policy & Economics. (2021, April 23). Schaeffer Solutions: Developing Innovative Payment Models for Prescription Drugs. Retrieved from https://schaeffer.usc.edu/research/schaeffer-solutions-innovative-payment-models-for-prescription-drugs/
[7] American College of Physicians. (2025, January 6). Ensuring Prescription Drug Access and Affordability. Retrieved from https://www.acponline.org/advocacy/where-we-stand/2025-acp-priorities/ensuring-prescription-drug-access-and-affordability
[8] AHIP. (2024, June 21). Fact Check: Manufacturers Set High Drug Prices and Prevent Competition. Retrieved from https://www.ahip.org/news/articles/fact-check-manufacturers-set-high-drug-prices-and-prevent-competition