Introduction: From Defensive Necessity to Competitive Advantage
For decades, business continuity planning (BCP) in the biomedical and research sector was often viewed through a narrow lens—a compliance-driven, defensive measure filed away in a binder, designed to tick a box for regulators and auditors. It was a cost center, a necessary evil focused on recovering from a hypothetical fire, flood, or power outage. But the landscape has irrevocably shifted. The cascading disruptions of the last decade—global pandemics, geopolitical shocks that fractured supply chains, sophisticated cyberattacks, and the increasing frequency of extreme weather events—have exposed the profound fragility of this old paradigm.1 The traditional, cost-optimized, “just-in-time” model, once lauded for its efficiency, has been revealed as dangerously brittle.
In this new era of perpetual volatility, resilience is no longer a defensive tactic; it is the ultimate competitive advantage. For biomedical and research organizations, where the stakes involve not just profits but patient lives, the ability to anticipate, withstand, and adapt to disruption is a core measure of value. It is the bedrock of trust with patients, regulators, investors, and partners. A recent global monitoring platform revealed a startling fact: the life sciences industry has suffered from the highest number of disruptions of any sector. This is not a temporary anomaly; it is the new normal.
This report is not another treatise on writing a static BCP. Instead, it is a strategic blueprint for embedding true organizational resilience into the very DNA of your company. We will journey beyond the fundamentals of planning to explore the specific, high-stakes vulnerabilities that define the biomedical and research world. We will deconstruct the methodologies that allow you to identify and protect your “crown jewels”—from irreplaceable cell lines in a research lab to the integrity of a global clinical trial. We will fortify the most critical links in your value chain, from the sourcing of active pharmaceutical ingredients (APIs) in a tense geopolitical climate to the exacting demands of cryogenic logistics.
Crucially, we will reframe risk management itself. We will demonstrate how to move from a reactive posture to a proactive, intelligence-driven strategy, leveraging everything from advanced risk assessment tools to competitive patent data to see around corners and anticipate the disruptions of tomorrow. This is a guide for leaders who understand that in the 21st-century biopharma landscape, the most resilient organizations will not just survive—they will lead. They will capture market share, accelerate innovation, and deliver on their ultimate promise: protecting and improving human health, no matter what challenges arise.
Part I: The Architectural Framework of Organizational Resilience
To build a structure that can withstand any storm, you must first understand the principles of architecture. Similarly, building a resilient organization requires moving beyond the simple checklist of a traditional BCP to embrace a more dynamic and holistic framework. It’s about cultivating a set of inherent capabilities, guided by internationally recognized standards, that allow your organization not just to recover, but to evolve and grow stronger from adversity.
Deconstructing Resilience: Beyond BCP to a Dynamic Capability
The term “resilience” is often used interchangeably with “business continuity,” but this is a fundamental misunderstanding. Business continuity is about coping—executing a plan to restore critical functions after a disruption. Organizational resilience is a far broader and more profound concept. It is the inherent ability of an organization to absorb stress, adapt, and thrive in the face of change and uncertainty.5 It’s less about a static plan and more about a dynamic, learned capability. This capability is built upon three core pillars.
The Three Pillars of Resilience: Anticipation, Coping, and Adaptation
Modern resilience theory defines a clear, three-stage process that separates truly resilient organizations from those that are merely prepared for known threats. This model provides a powerful lens through which to assess and build your organization’s capabilities.6
- Anticipation: This is the proactive, forward-looking pillar. It is the ability to anticipate potential threats and detect emerging problems before they escalate into full-blown crises. Anticipation is not about predicting the future with a crystal ball; it’s about robust environmental scanning, sophisticated risk assessment, and leveraging intelligence from a wide range of sources. For a biopharma company, this means monitoring geopolitical tensions that could affect API suppliers, tracking new cyber threats targeting clinical trial data, and even analyzing competitor patent filings for signs of disruptive new technologies. It’s about asking “What might go wrong?” and having the systems in place to find the answers.
- Coping: This is the domain of traditional business continuity and crisis management. It is the ability to effectively manage and absorb the shock of an adverse event while it is happening, maintaining critical functions under immense stress. When a hurricane makes landfall near your manufacturing facility or a critical supplier suddenly goes offline, your coping capability is what allows you to activate incident response teams, execute pre-defined continuity plans, and protect your people, assets, and operations. A well-rehearsed BCP is the essential playbook for the coping phase.
- Adaptation: This is arguably the most critical and often overlooked pillar. Adaptation is the capacity to learn from an adverse event and evolve. It is not about simply returning to the “old normal” but about emerging stronger, smarter, and better prepared for the future.5 If a cold chain failure resulted in the loss of a valuable shipment, adaptation means analyzing the root cause, implementing new monitoring technology, validating a new packaging solution, and fundamentally improving the process to prevent a recurrence. It is the mechanism by which an organization transforms a crisis from a pure loss into a strategic investment in future resilience.
The Role of Organizational Learning in Building Resilience
What fuels these three pillars? The single most important factor is organizational learning (OL). An organization’s ability to learn is inextricably linked to its ability to be resilient. Research has shown that learning is not just a byproduct of resilience; it is a fundamental precondition and an ongoing process that reinforces it at every stage.6
This learning takes several forms. It includes exploitative learning, which is the process of refining and improving existing processes based on experience—making your current operations more robust. It also includes exploratory learning, which is the search for new solutions, new technologies, and new ways of thinking, which is essential for adapting to novel, unforeseen threats.
Perhaps the most sophisticated form of organizational learning is the concept of “unlearning”. This is the critical and often difficult process of recognizing and discarding outdated assumptions, obsolete routines, and ingrained mental models that may have worked in the past but now actively hinder adaptation. A company that cannot unlearn its reliance on a single-source supplier, even after repeated disruptions, is a company that cannot truly become resilient.
This deep connection between learning and resilience has a profound implication for leadership. It demonstrates that an organization’s resilience is not determined solely by its operational plans or technical infrastructure, but by its culture. A hierarchical, siloed culture where information is hoarded, mistakes are punished, and bad news is suppressed actively inhibits the learning required for resilience. It prevents the organization from anticipating threats because information doesn’t flow freely. It hampers coping because cross-functional collaboration is weak. And it makes adaptation impossible because an honest assessment of failures cannot occur.
Conversely, a culture that fosters psychological safety, encourages cross-functional collaboration, empowers employees to raise concerns, and treats failures as learning opportunities is a culture that is inherently resilient.8 Therefore, building a resilient organization is not just a task for the Chief Risk Officer; it is a core responsibility of leadership and human resources. Investing in leadership development, collaborative tools, and a culture of continuous improvement is a direct investment in your company’s ability to withstand the next crisis.
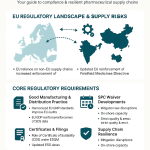
Anchoring Your Strategy: The Role of ISO 22301 and ICH Q9
While culture and learning provide the “software” for resilience, organizations also need a robust “operating system”—a structured framework to guide their efforts. For biomedical and research organizations, two standards are paramount: ISO 22301, the global benchmark for business continuity management, and ICH Q9, the definitive guide for quality risk management in the pharmaceutical industry. These are not competing standards; they are complementary frameworks that, when integrated, provide a powerful, auditable, and regulatorily sound foundation for resilience.
ISO 22301: The Global Standard for Business Continuity Management Systems (BCMS)
ISO 22301 provides a universal language and a systematic methodology for building, implementing, and improving a Business Continuity Management System (BCMS).11 It elevates business continuity from a series of disconnected plans into a cohesive, managed program that is embedded in the organization’s overall management structure.
At its core, the standard is built on the well-established Plan-Do-Check-Act (PDCA) cycle, a model for continuous improvement :
- Plan: This is the foundational phase. It involves understanding the organization’s context (its objectives, stakeholders, and regulatory environment), securing leadership commitment, and, most importantly, conducting a Business Impact Analysis (BIA) and risk assessment to identify critical processes and potential threats.
- Do: This is the implementation phase. Here, the organization develops and documents its business continuity plans, incident response procedures, and communication protocols based on the findings of the “Plan” phase.
- Check: This is the evaluation phase. A plan that hasn’t been tested is merely a theory. This phase mandates the regular testing of continuity plans through drills and exercises, conducting internal audits, and monitoring the performance of the BCMS to ensure it remains effective and fit for purpose.11
- Act: This is the improvement phase. Based on the results of tests, audits, and real-world incidents, the organization takes corrective actions to address any identified nonconformities and continually improve the BCMS.13
Adopting an ISO 22301 framework provides tangible benefits beyond just being prepared. It demonstrates to regulators, partners, and customers that your organization has a mature, internationally recognized approach to resilience. It can provide a significant marketing and competitive advantage, reduce dependence on a few key individuals, and ensure a structured, predictable response when a crisis hits.
ICH Q9: Quality Risk Management (QRM) in the Pharmaceutical Context
While ISO 22301 provides the “how-to” for a management system, ICH Q9: Quality Risk Management provides the specific philosophical underpinning required for the pharmaceutical industry.8 It ensures that all risk management activities are anchored in the principles that matter most to regulators and patients.
ICH Q9 is guided by two primary principles :
- The evaluation of risk to quality should be based on scientific knowledge and ultimately link to the protection of the patient. This is the non-negotiable core of pharma risk management. Every risk assessment, every BIA, every continuity plan must ultimately be able to answer the question: “How does this protect the patient?”
- The level of effort, formality, and documentation of the Quality Risk Management process should be commensurate with the level of risk. This principle provides crucial flexibility. It means you don’t need to apply the same exhaustive level of analysis to a low-risk process that you would to a critical manufacturing step that directly impacts product safety and efficacy.
This QRM process is not a one-time event but a continuous cycle that should be integrated throughout the product’s lifecycle, from early development through to commercial manufacturing and distribution.8
The true power of these frameworks is realized when they are integrated. A biopharma organization could, in theory, be ISO 22301 certified but still fail a regulatory inspection if its BIA prioritizes financial impact over patient safety. Conversely, a company could follow the principles of ICH Q9 but lack the overarching BCMS structure to handle non-quality disruptions like a major IT outage or a facility lockdown.
The most effective and resilient approach is to build an ISO 22301-compliant BCMS where the core processes—especially the BIA and risk assessment—are fundamentally driven by the patient-centric principles of ICH Q9. This creates a unified system that is both operationally robust across all types of disruptions and fully aligned with the stringent quality and safety expectations of the pharmaceutical world.
Part II: The Methodologies of Risk Assessment and Mitigation
A resilient architecture is built on a solid foundation of analysis. Before you can mitigate risks, you must first identify, understand, and prioritize them. In the biomedical world, this requires a suite of specialized analytical tools that go far beyond a simple checklist. These methodologies—Business Impact Analysis (BIA), Failure Mode and Effects Analysis (FMEA), and Hazard and Operability (HAZOP) studies—provide the structured, data-driven insights needed to make intelligent decisions about where to invest your resources for maximum resilience.
The Business Impact Analysis (BIA): Identifying Your Crown Jewels
The Business Impact Analysis is the cornerstone of any effective business continuity program. It is the systematic process of predicting the consequences of a disruption to your critical business functions and processes.19 In essence, it answers the fundamental question: “If something breaks, what hurts the most, and how quickly does it need to be fixed?” The output of a BIA is not the plan itself, but the critical information required to build an intelligent and prioritized plan.
The Purpose and Process of a BIA
A comprehensive BIA follows a structured process, typically involving a cross-functional team of subject matter experts (SMEs) from across the organization who have intimate knowledge of day-to-day operations.20 The key steps include 19:
- Determine Scope and Goals: Clearly define which parts of the organization the BIA will cover and what the primary objectives are.
- Identify Critical Functions: Through interviews and questionnaires, gather data from each department to identify the essential activities and services they perform.
- Understand Dependencies: Map the intricate web of dependencies for each critical function. This includes internal dependencies (e.g., a manufacturing process depending on the IT network) and external dependencies (e.g., reliance on a single raw material supplier or a contract research organization).
- Assess Impact: Analyze and quantify the potential impact of a disruption to each function over time. This assessment should cover multiple dimensions: financial (lost revenue, increased expenses), operational (production stoppage), reputational (damage to brand trust), and legal/regulatory (fines, compliance breaches).21
- Set Recovery Objectives: For each critical function, establish the key recovery metrics: the Recovery Time Objective (RTO) and the Recovery Point Objective (RPO). We will explore these in more detail later.
- Prioritize Functions: Based on the impact assessment and recovery objectives, rank the business functions in order of criticality. This prioritization is crucial for guiding response efforts and resource allocation during a crisis.
- Document and Report: Prepare a detailed report summarizing the findings, priorities, and recommendations. This document becomes the foundational evidence for developing and justifying the business continuity plan.
Tailoring the BIA for Biomedical Organizations
While the BIA process is universal, its application in a biomedical context requires a specialized focus. A generic BIA might prioritize functions based solely on revenue, but in the life sciences, the calculus is far more complex.
- Product Prioritization: The BIA must begin not with processes, but with products. A foundational activity is to prioritize the product portfolio based on patient impact and medical necessity.2 A life-saving oncology drug or a therapy for a rare disease with no alternatives may have a much higher continuity priority than a high-volume lifestyle product, regardless of their respective revenues. This prioritization, guided by the principles of ICH Q9, must be the North Star for the entire BIA.
- Identifying Critical Assets: A biopharma BIA must look beyond processes to identify unique and often irreplaceable assets. These are the physical and digital “crown jewels” of the organization. They include master and working cell banks stored in liquid nitrogen, unique biological specimens from long-term studies, decades of clinical trial data, highly specialized and calibrated equipment like bioreactors and mass spectrometers, and, of course, the animals in vivarium facilities.23 The loss of these assets can set back research by years or even decades, a consequence far exceeding any short-term financial loss.
- Assessing Pharma-Specific Impacts: The impact assessment must incorporate consequences unique to the industry. These include the compromise of patient safety, breaches of Good Clinical Practice (GCP) or Good Manufacturing Practice (GMP), significant regulatory fines or sanctions, the irretrievable loss of clinical trial data, and the ethical and reputational fallout from failing to supply a critical medicine.1
To make this tangible, consider a sample BIA for a fictional monoclonal antibody, “ResiliMab.”
| Critical Business Function | Key Dependencies | Impact of Disruption (within 72 hours) | Maximum Tolerable Downtime (MTD) | Recovery Time Objective (RTO) | Recovery Point Objective (RPO) | Existing Mitigations |
| Master Cell Bank (MCB) Maintenance | -80°C Freezer Farm, Backup Power, LN2 Supply, Temperature Monitoring System | Operational: Irreversible loss of irreplaceable cell line. Financial: Loss of entire product pipeline future. Patient Safety: Catastrophic long-term impact. | 8 hours (time to thaw) | 4 hours | N/A | Dual freezers on separate circuits, remote alarm system, backup generator. |
| Upstream Manufacturing (Bioreactor Run) | Single-Use Bioreactor Bags, Cell Culture Media, Water for Injection (WFI) System, MES | Operational: Loss of entire multi-million dollar batch. Financial: Significant revenue loss, potential drug shortage. | 2 hours (critical process window) | 1 hour | 15 minutes (for MES data) | Safety stock of single-use bags, qualified second media supplier. |
| Clinical Trial Data Collection | Electronic Data Capture (EDC) System, Site Internet Connectivity, Clinical Research Associates (CRAs) | Operational: Inability to capture critical patient data. Regulatory: Potential GCP violation, data integrity issues. | 24 hours | 4 hours | 5 minutes | Cloud-based EDC with high availability, offline data capture capability. |
Proactive Failure Prevention: Applying FMEA and HAZOP in Manufacturing and R&D
If the BIA tells you what to protect, FMEA and HAZOP tell you how things might break so you can fix them ahead of time. These are not just engineering tools; they are powerful business methodologies for proactively identifying and mitigating risks before they can cause a disruption.
Failure Mode and Effects Analysis (FMEA)
FMEA is a systematic, bottom-up technique for identifying all the potential ways a process or product could fail (the “failure modes”) and then analyzing the potential consequences of those failures (the “effects”).24 It is a proactive tool designed to prevent problems rather than react to them.
The FMEA process is a structured team exercise that involves 30:
- Breaking down a process into its individual steps.
- For each step, brainstorming potential failure modes (“What could go wrong here?”).
- Identifying the potential effects of each failure (e.g., compromised product quality, patient harm).
- Determining the potential root causes of each failure.
- Assigning numerical scores on a scale (typically 1-10) for three key factors:
- Severity (S): How severe is the consequence of the failure? (1 = insignificant, 10 = catastrophic).
- Occurrence (O): How likely is this failure to happen? (1 = extremely unlikely, 10 = almost certain).
- Detection (D): How likely are we to detect the failure before it causes harm? (1 = certain detection, 10 = cannot be detected).
- Calculating the Risk Priority Number (RPN) by multiplying the three scores: RPN=S×O×D. The RPN can range from 1 to 1000.
- Prioritizing and taking action on the failure modes with the highest RPNs, implementing controls or process changes to reduce their severity, occurrence, or improve their detection.
For example, in the synthesis of a peptide API, a potential failure mode could be “cross-contamination with another peptide sequence”. The effect could be a toxic impurity in the final drug product (Severity = 10). The cause might be inadequate cleaning of a shared reactor. If this has happened before, the Occurrence might be a 4. If the analytical methods to detect this specific contamination are poor, the Detection score might be a 7. This would yield a high RPN of 10×4×7=280, signaling an urgent need to improve reactor cleaning validation and develop more specific analytical tests.
Hazard and Operability (HAZOP) Study
A HAZOP study is another structured brainstorming technique, but it is typically applied to more complex systems like manufacturing facilities and equipment, often during the design phase.32 It works by systematically challenging the design intent of a system.
The HAZOP team, composed of multi-disciplinary experts, examines a process diagram (like a Piping and Instrumentation Diagram, or P&ID) node by node. For each node, they apply a set of standardized “guide words” to process parameters to explore potential deviations :
- Guide Words: NO/NOT, MORE, LESS, AS WELL AS, PART OF, REVERSE, OTHER THAN.
- Process Parameters: FLOW, TEMPERATURE, PRESSURE, LEVEL, CONCENTRATION.
By combining these, the team generates “what-if” scenarios. For example, applying “NO” to “FLOW” in a cooling water line to a bioreactor leads the team to analyze the causes (e.g., pump failure, closed valve) and consequences (e.g., temperature rise, cell death, batch loss) of a “no flow” deviation. This systematic approach ensures that all credible deviations are considered, uncovering hidden hazards and operability problems that might be missed by less structured reviews.
The outputs of FMEA and HAZOP analyses provide a critical, quantifiable basis for making investment decisions in resilience. When a leader needs to justify the capital expenditure for a redundant WFI system or the operational cost of qualifying a second supplier, the FMEA/HAZOP report provides the evidence. It translates abstract operational risks into a structured, data-driven argument, showing the calculated severity and likelihood of failure. This allows the cost of mitigation to be weighed directly against the potential cost of the unmitigated risk, turning risk management into a core part of the strategic budgeting and planning process.
Defining the Clock: Setting Realistic RTOs and RPOs for Critical Systems
Once the BIA has identified your critical functions, you need to define the timeline for their recovery. This is where two of the most important metrics in business continuity come into play: the Recovery Time Objective (RTO) and the Recovery Point Objective (RPO).
- Recovery Time Objective (RTO): This is the maximum acceptable amount of time that a system or process can be down before the disruption causes unacceptable consequences to the business.34 It answers the question,
“How fast do we need to recover?” An RTO could be measured in minutes, hours, or days. - Recovery Point Objective (RPO): This is the maximum acceptable amount of data loss, measured in time. It represents the point in time to which data must be recovered for operations to resume.34 It answers the question,
“How much data can we afford to lose?” An RPO of 15 minutes means the system must be recoverable to a state that is no more than 15 minutes old.
These objectives are not arbitrary technical settings; they are direct outputs of the BIA and are determined by the criticality of the business function they support.25 For example:
- A clinical trial’s Electronic Data Capture (EDC) system, which holds irreplaceable patient safety and efficacy data, would have a very aggressive RTO (minutes to a few hours) and a near-zero RPO (minutes or even seconds) to comply with GCP and protect data integrity.
- A manufacturing execution system (MES) controlling a live batch would have a low RTO (hours) to prevent the loss of a valuable product in process.
- The -80°C freezer holding your master cell bank has an RTO dictated by physics—the amount of time it takes for the internal temperature to rise to a critical threshold where the cells are damaged.
- An internal HR or finance system might have a much longer RTO (e.g., 24-48 hours), as its immediate downtime does not directly impact patient safety or core research and manufacturing operations.
It is crucial for business leaders to understand that there is a direct, and often exponential, relationship between the stringency of these objectives and their cost.37 An RTO of near-zero requires massive investment in high-availability architecture, real-time data replication, and automated failover systems. An RTO of 24 hours might be achievable with far less expensive periodic backups and a manual recovery process.
This reality makes the setting of RTOs and RPOs a critical strategic business decision, not just an IT task. The BIA process forces this essential conversation. It allows business leaders to work with their IT and operations counterparts to align recovery capabilities with business priorities, ensuring that the most significant investments in disaster recovery are targeted precisely where they deliver the most value and mitigate the most critical risks.
Part III: Fortifying the Value Chain: End-to-End Supply Chain Resilience
The biopharmaceutical value chain is a marvel of global interconnectedness, but this complexity is also its greatest vulnerability. A single point of failure—a contamination event at a raw material supplier, a geopolitical flare-up in a key manufacturing region, a customs delay for a temperature-sensitive shipment—can have cascading effects, leading to drug shortages, clinical trial delays, and direct harm to patients.3 Building resilience requires a deep, end-to-end focus on the most fragile links: API sourcing, single-use technologies, and the cold chain.
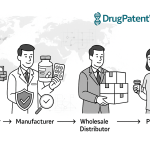
The API Lifeline: Managing Risk in a Geopolitically Complex World
The Active Pharmaceutical Ingredient (API) is the biological or chemical heart of any drug. The global supply chain for APIs is notoriously concentrated, with a heavy reliance on a few key countries, particularly China and India. This concentration creates immense geopolitical, logistical, and quality risks that have been starkly highlighted in recent years.
The risks are manifold and include sudden supplier failures due to financial or operational issues, quality deviations or cross-contamination events that can halt production , unexpected and dramatic price increases, and regulatory or political actions that can sever supply lines overnight. The passage of legislation like the BIOSECURE Act, which restricts U.S. federal funding for companies using certain China-based CDMOs, is a prime example of how quickly geopolitical tensions can translate into tangible supply chain risk.
Mitigating these risks requires a multi-pronged, proactive strategy:
- Dual and Multi-Sourcing: The most fundamental strategy is to move away from single-sourcing for critical APIs. Qualifying and maintaining active relationships with at least two suppliers in different geographic regions is essential to creating redundancy and avoiding a single point of failure.1 This provides an immediate backup if one supplier experiences a disruption.
- Robust Supplier Management: Treat your API suppliers as true partners, not just transactional vendors. This involves rigorous initial qualification and regular audits to ensure their quality systems are robust and compliant with current Good Manufacturing Practices (cGMP). Formal Quality Agreements should be in place to clearly define responsibilities, specifications, and change control procedures.
- Strategic Safety Stock: While lean inventory has its benefits, for critical APIs, maintaining a strategic safety stock is a crucial buffer against short-term disruptions. The decision on how much inventory to hold—often six months’ worth or more—is a strategic trade-off, balancing the carrying costs against the immense financial and reputational cost of a stock-out.
- Onshoring and Regionalization: There is a growing trend to re-evaluate and, where feasible, “reshore” or “regionalize” parts of the API supply chain.4 While potentially more expensive in the short term, manufacturing critical APIs closer to the end market can dramatically reduce lead times and insulate the supply chain from global geopolitical volatility.
The Single-Use Paradox: Balancing Flexibility with Supply Security
Single-Use Technologies (SUTs)—plastic bioreactor bags, tubing assemblies, filters, and connectors—have revolutionized modern biomanufacturing. They offer tremendous benefits in flexibility, speed, and cost, eliminating the need for complex cleaning and sterilization processes, reducing capital investment, and allowing for rapid changeover between products.45 This has enabled the rise of multi-product facilities and accelerated the timeline for bringing new therapies to market.
However, this flexibility creates a critical dependency, a “single-use paradox.” By outsourcing the “sterility” function to a supplier, biopharma companies have swapped one set of risks (in-house cleaning validation) for another: a deep and often fragile reliance on a highly specialized supply chain for irradiated plastics and custom-built assemblies. The risks are significant and include long lead times, raw material shortages (particularly for specialized plastic resins), a high degree of supplier concentration, and potential quality issues like extractables and leachables that can impact the final drug product.
Securing this critical supply chain requires a dedicated set of strategies:
- Suppliers as Strategic Partners: Your key SUT suppliers are not just vendors; they are an extension of your own manufacturing facility. A collaborative partnership is essential. This includes sharing long-range forecasts, conducting joint risk assessments, and, critically, performing due diligence to ensure your supplier has their own robust business continuity plan in place. Ask them: what is your plan if your primary resin supplier goes down, or if your gamma irradiation facility is unavailable?
- Component Standardization: The proliferation of custom, product-specific SUT assemblies can create a logistical nightmare with hundreds of unique SKUs. Where possible, organizations should drive a strategy of standardization, using common components (e.g., connectors, tubing types) across multiple processes and products. This increases interchangeability, simplifies inventory management, and provides more flexibility in a shortage.
- Strategic Inventory and Warehousing: Given the long lead times for many SUTs, holding strategic inventory is often necessary. However, many biopharma companies lack the specialized, climate-controlled warehouse space required for these bulky products. Partnering with suppliers or specialized third-party logistics (3PL) providers to maintain dedicated, localized inventory can be an effective way to buffer the supply chain and ensure quick access to critical components when needed.
The Cold Chain Imperative: Safeguarding Biologics from Lab to Patient
For a growing number of advanced therapies—including biologics, vaccines, and cell and gene therapies—the supply chain is a race against the clock and the thermometer. These products are exquisitely sensitive to temperature, and even a brief excursion outside their specified range can lead to denaturation, aggregation, and an irreversible loss of efficacy, posing a direct risk to patient safety.47
The World Health Organization (WHO) estimates that nearly 50% of vaccines are wasted globally every year, with a significant portion of this loss attributed to failures in temperature control during transport and storage.
The cold chain is not a single entity but a spectrum of tightly controlled environments:
- Refrigerated: 2°C to 8°C, for many vaccines and monoclonal antibodies.
- Frozen: -20°C to -80°C, for certain drug substances and therapies.
- Cryogenic: Below -150°C, typically using liquid nitrogen, for cell and gene therapies.
Each handoff point in the logistics journey—from the manufacturing site to a truck, from the truck to an airport tarmac, during customs inspection, and in the final last-mile delivery to a clinic or patient—is a potential point of failure.48
Building a resilient cold chain is a non-negotiable requirement, demanding a focus on three key areas:
- Validated Packaging and Labeling: This is the first line of defense. It involves using thermally qualified shipping containers (e.g., insulated boxes with phase-change materials or active, powered units) that have been rigorously tested and validated to maintain the required temperature for a specific duration under worst-case external conditions. Proper labeling that can withstand extreme temperatures is also critical for compliance and handling.
- End-to-End Visibility and Monitoring: You cannot manage what you cannot see. The use of real-time monitoring devices that track both location and internal temperature throughout the shipment’s journey is becoming the industry standard. These systems provide end-to-end visibility and can send automated alerts if a temperature excursion is imminent, allowing for proactive intervention to save a shipment before it is lost.48
- Proactive Contingency Planning: Hope is not a strategy. Resilient organizations pre-qualify alternate shipping lanes and backup carriers. They have clear, pre-defined protocols for what to do if a shipment is delayed or if a temperature alarm is triggered. This includes identifying locations where a shipment can be temporarily stored or “re-iced” to maintain its integrity.
Ultimately, these three pillars of supply chain resilience demonstrate a fundamental shift in the industry. Supply chain management is no longer a siloed logistics function focused on cost. A failure in the supply chain—whether it’s an API shortage, a defective single-use bag, or a broken cold chain—is now rightly understood as a quality failure, a regulatory failure, and a direct threat to patient safety. This means the principles of Quality Risk Management must be deeply embedded in every supply chain decision. The Chief Supply Chain Officer and the Head of Quality must work in lockstep, with an integrated governance model that extends quality oversight deep into the global supplier network. This vision is strongly supported by recent industry analyses from firms like Deloitte and McKinsey, which call for the creation of truly digitalized, visible, and integrated supply networks as the foundation for future resilience.51
Part IV: Protecting the Engine of Innovation: R&D and Clinical Trial Continuity
While the supply chain delivers today’s therapies, the research and development (R&D) engine is creating tomorrow’s. The assets within R&D labs and clinical trials are often unique, priceless, and irreplaceable. A disruption here doesn’t just impact quarterly revenue; it can erase decades of scientific progress and derail the future of the company. Building resilience in this environment requires highly specialized protocols that protect both the physical assets of research and the human subjects who make that research possible.
The Unfreezing Point: A Protocol for Laboratory and Vivarium Resilience
Research laboratories are complex ecosystems, highly dependent on specialized equipment, controlled environments, and highly skilled personnel. They are uniquely vulnerable to common disruptions like power outages, equipment failures, fires, or floods, which can have devastating and irreversible consequences.23
Safeguarding Irreplaceable Biological Assets
At the heart of many biomedical labs are collections of biological materials—cell lines, patient samples, antibodies, viruses—that represent years or even a lifetime of work. The loss of these assets is a catastrophic failure. A robust continuity plan for the lab must therefore have a laser focus on protecting them.
A prime example is the -80°C freezer failure protocol. Ultra-low temperature (ULT) freezers are the vaults that hold many of these biological crown jewels. A failure is not a matter of if, but when. A comprehensive protocol must address the entire lifecycle of risk:
- Prevention: This is the most critical step. It includes a rigorous program of regular preventative maintenance for all ULT freezers. Crucially, it involves installing robust temperature monitoring systems that are connected to a remote alarm service, capable of sending text or email alerts to designated on-call personnel 24/7.58 A simple local alarm that beeps in an empty building overnight is useless. The single most important preventative measure is to
never store 100% of an irreplaceable sample in a single freezer. Critical stocks must be split and stored in separate freezers, ideally located in different rooms or buildings and connected to separate electrical circuits. - Response: When an alarm is triggered, the response must be swift and organized. The lab’s BCP must include an up-to-date emergency contact list and a clear escalation path. There must be a pre-identified, designated backup freezer that is maintained, empty, and ready for use. The plan should detail the procedure for safely and quickly transferring materials from the failing freezer to the backup unit.58
- Decontamination: After a failure, the freezer must be properly decontaminated before being repaired or replaced. The protocol must consider the nature of the materials stored and provide clear instructions for cleaning up chemical, biological, or radioactive hazards, referencing Safety Data Sheets (SDSs) as needed.
Beyond freezer failure, general lab continuity planning involves identifying and prioritizing the lab’s essential functions, cross-training personnel on critical techniques and equipment operation, and ensuring that all experimental data is securely and regularly backed up to a separate location.61 The plan must cover not just samples, but also the maintenance of unique cell cultures and critical equipment that cannot be easily shut down.
Disaster Recovery for Animal Research Facilities (Vivariums)
Animal research facilities, or vivariums, present an even more complex continuity challenge due to the significant ethical and regulatory oversight involved. A disaster plan for a vivarium is not just good practice; it is a requirement under the Animal Welfare Act (AWA), Public Health Service (PHS) Policy, and for accreditation by bodies like AAALAC International.63
The core components of a vivarium disaster plan must include:
- Primacy of Human Safety: The plan must state unequivocally that in an emergency, human life takes precedence. Personnel should never place themselves in harm’s way to evacuate animals.
- Triage and Prioritization: Not all animals can be saved in a catastrophic event. Investigators, in collaboration with veterinary staff, must decide in advance which animal lines are the most critical due to their scientific value or irreplaceability. This triage plan is an essential and difficult part of the planning process.
- Shelter-in-Place vs. Evacuation: The plan must have detailed procedures for both scenarios. Shelter-in-place focuses on maintaining life-sustaining systems like HVAC, potable water, and food supplies.64 Evacuation plans must identify safe, pre-determined relocation sites and methods for transport.
- Humane Euthanasia: The plan must include a clear and humane protocol for euthanizing animals that are severely injured or cannot be protected from the consequences of the disaster.
- Essential Personnel: A list of essential personnel who are trained in the disaster plan and authorized to access the facility during an emergency must be maintained and shared with institutional security and local emergency responders.64
Safeguarding the Trial: Ensuring Patient Safety and Data Integrity Amidst Chaos
Clinical trials are the final and most critical stage of R&D, where a potential therapy is tested in human subjects. A disruption during a clinical trial—whether from a natural disaster, a pandemic, or geopolitical conflict—poses a dual threat: to the safety of the participants and to the integrity of the data that will determine the drug’s fate.
The Primacy of Patient Safety During Disruptions
The first, last, and only absolute priority during a clinical trial disruption is the safety and well-being of the trial participants.66 All continuity and recovery actions must be viewed through this lens. This includes the ethical obligation to ensure that patients have access to appropriate medical care and follow-up, even if their formal participation in the trial has to be suspended or terminated.
Recent events, from wildfires threatening research sites in California to the war in Ukraine impacting clinical trials across Eastern Europe, have underscored the need for flexibility, creativity, and compassion from research teams.66 It may no longer be safe or feasible for a patient to travel to a trial site, but they may wish to continue receiving the investigational product. The BCP must empower trial teams to make patient-centric decisions in these challenging circumstances.
Maintaining Data Integrity and Regulatory Compliance
Alongside patient safety is the critical need to maintain the integrity of the clinical trial data. The data collected is the evidence upon which regulatory agencies like the FDA and EMA will base their approval decisions. Compromised data can render a multi-billion dollar trial worthless.
Data integrity is defined by the “ALCOA+” principles: the data must be Attributable, Legible, Contemporaneous, Original, and Accurate, as well as Complete, Consistent, Enduring, and Available.70 FDA guidance for computerized systems used in clinical trials is explicit: sponsors must have validated systems, robust backup and recovery procedures, and documented contingency plans to protect against data loss and ensure data quality in the event of a system failure.73
This makes the security and resilience of the trial’s IT infrastructure paramount. Modern trials rely heavily on Electronic Data Capture (EDC) systems, which must be protected by stringent cybersecurity measures, including encryption, strict access controls, and immutable audit trails that document every single change made to the data.28
Adapting Trial Conduct: The Rise of Decentralized Models
The need to adapt trial conduct during a crisis has accelerated the adoption of Decentralized Clinical Trial (DCT) methodologies. These approaches, which were once niche, are now seen as an inherent resilience strategy. Instead of relying solely on patients traveling to physical sites, DCTs leverage digital tools and alternative service providers to bring the trial to the patient.
A proactive BCP for clinical research should build these flexible capabilities into trial protocols from the outset. This “toolbox” of strategies allows a trial to pivot efficiently when a disruption occurs, protecting both patients and data integrity.66
The following matrix outlines some key challenges and the corresponding preemptive and reactive strategies.
| Challenge | Preemptive Strategy (Proactive BCP) | Post-Disruption Response Options (Reactive) |
| Patients or staff unable to travel to research site | Incorporate options for remote/virtual visits (telemedicine) into the trial protocol from the start. | Transition to a decentralized trial model for affected sites/patients. Relocate patients to other local, unaffected sites if feasible. |
| Staff unavailable to dispense investigational drug on site | Establish and validate a direct-to-patient (DTP) drug delivery supply chain. | Activate the DTP shipment process for affected participants. |
| Limited resources for study lab draws; unable to ship samples to central lab | Pre-qualify and validate local laboratories in key regions. Contract with a mobile phlebotomy service. | Minimize non-essential lab draws, prioritizing safety and primary endpoint data. Pivot from central to local lab testing with clear documentation of the deviation. |
| Inability to collect certain endpoint data in person (e.g., a 6-minute walk test) | Embed validated patient-reported outcomes (PROs) or data from wearable devices as secondary or exploratory endpoints in the trial design. | Collect patient-reported outcomes and events via remote strategies (e.g., phone, app). Acquire source documents from local care providers to the extent possible. |
By proactively building this flexibility into the trial design, organizations can move from a state of reactive scrambling to one of structured, controlled adaptation, ensuring the continuity of their most critical research programs.
Part V: The Human Element: Crisis Communication and Reputation Management
In the midst of a disruption, the most sophisticated operational plans can fail if communication breaks down. A crisis is not just a logistical challenge; it is a test of trust. For a biomedical organization, where reputation is built on a foundation of scientific integrity and patient safety, managing the human element of a crisis is paramount. An effective crisis communication plan and a proactive approach to reputation management are not soft skills; they are core components of a resilient enterprise.
Mastering the Narrative: A Crisis Communication Blueprint for Pharma
When a crisis hits—be it a data breach, a manufacturing failure, or a product safety concern—a vacuum of information is created. If you do not fill that vacuum with timely, accurate, and empathetic communication, it will be filled by speculation, misinformation, and fear. The primary goals of a crisis communication plan are to minimize this chaos, maintain the trust of your stakeholders, and protect your hard-won reputation.
A robust plan is not something you improvise during an emergency. It is a pre-built and rehearsed playbook. The key steps to creating this blueprint include 77:
- Identify Potential Scenarios: Brainstorm the types of crises your organization could face, from product recalls and clinical trial halts to cybersecurity incidents and facility shutdowns.
- Define Communication Goals: For each scenario, what are you trying to achieve with your communication? Is it to ensure employee safety, reassure investors, provide clear instructions to patients, or correct misinformation in the media?
- Assign Roles and Responsibilities: Designate a core crisis communication team with clearly defined roles. This typically includes a Crisis Manager to oversee the strategy, a designated Spokesperson trained to handle media and public inquiries, and a communications team responsible for drafting and disseminating messages.
- Develop Pre-Approved Messaging: You cannot write the perfect press release in the heat of the moment. Develop messaging templates and holding statements for your most likely crisis scenarios. These should be clear, concise, and communicate what happened, the impact on stakeholders, the steps you are taking, and where to find more information.
- Establish Multi-Channel Communication: Your stakeholders consume information in different ways. Your plan must leverage multiple channels to ensure your message gets through, including mass notifications (email, SMS), social media platforms, the company website, press releases, and direct outreach to key partners.77
- Implement Monitoring Protocols: Set up tools to monitor media coverage and social media sentiment in real-time. This allows you to track the narrative, identify and correct misinformation quickly, and adjust your strategy based on public feedback.
Underpinning this entire process are a few core principles: Be proactive, not reactive. Act quickly, as delays breed speculation. And above all, be transparent and honest. Acknowledging the problem and being upfront about the steps you are taking is the fastest way to build and maintain trust.77
Engaging Key Stakeholders During a Crisis
A one-size-fits-all message is a message that resonates with no one. Effective crisis communication requires tailoring your messaging to the specific needs and concerns of your various stakeholder groups. For a biopharma company, the key audiences include:
- Patients and the Public: This is your most important audience. They need clear, empathetic, and jargon-free information about any potential risks to their health, what they should do, and where they can get help. Dedicated patient hotlines and clear, accessible information on your website are crucial.
- Healthcare Professionals (HCPs): Doctors, pharmacists, and nurses are on the front lines. They are the trusted intermediaries for patients. They must be provided with detailed, accurate, and timely information about the issue, its clinical implications, and any alternative treatments so they can advise their patients effectively.
- Regulatory Agencies (FDA, EMA, etc.): Regulators require immediate, comprehensive, and factual reporting. Communication with agencies must be handled with extreme care and precision, following all established protocols.
- Employees: Your employees should be among the first to be informed, not the last. Keeping them updated ensures consistent external messaging, maintains morale, and makes them ambassadors for the company’s responsible handling of the crisis.
- Investors and Shareholders: This group needs transparent communication about the potential financial and operational impacts of the crisis. A clear, confident response plan can help maintain investor confidence and stabilize stock value.
- The Media: Proactively managing media relations is essential to controlling the narrative. This means providing a trained, credible spokesperson who can communicate with empathy, accountability, and clarity, preventing misinformation from taking root.
Reputation Under Fire: Navigating the Aftermath of a Product Recall
A product recall is one of the most severe crises a pharmaceutical company can face. It is not merely a logistical exercise of retrieving products from the market; it is a profound threat to the company’s core asset: its reputation for quality and safety. The financial impacts are often staggering. Studies have shown that the loss in a firm’s value following a recall can be many times greater than the direct costs of the recall itself, reflecting the significant damage to the company’s goodwill and reputation.82
Interestingly, research suggests a “reputation as a liability” paradox: highly reputed firms may suffer more from a recall because the event represents a greater violation of the high expectations and trust placed in them. This makes the management of the recall and the subsequent communication strategy absolutely critical.
Navigating this minefield requires a strategy focused on long-term reputation recovery:
- Take Full Accountability: Where the company is at fault, a sincere and public apology is often the necessary first step. Acknowledging the problem and taking responsibility demonstrates accountability and a commitment to doing the right thing.
- Communicate Corrective Actions: It’s not enough to say you’re sorry. You must clearly and repeatedly communicate the concrete steps you are taking to investigate the root cause, fix the problem, and, most importantly, prevent it from ever happening again.
- Conduct a Rigorous Post-Mortem: A crisis is a terrible thing to waste. Once the immediate situation is stabilized, the organization must conduct a thorough post-mortem analysis to understand what went wrong—not to assign blame, but to learn.78 Were the initial warning signs missed? Were communication protocols effective? Did the crisis management framework hold up?
- Embed the Lessons Learned: The final step is to use the findings from the post-mortem to improve. This means revising protocols, enhancing training programs, updating risk assessment tools, and fostering a culture that is more vigilant and better prepared for the future. This is the mechanism by which a crisis, painful as it is, becomes a catalyst for building greater resilience.
Part VI: The Strategic Edge: Leveraging Intelligence for Proactive Resilience
True resilience is not just about reacting well to unforeseen events; it’s about seeing them coming. The most mature organizations are moving beyond traditional risk registers and historical data to embrace a more forward-looking, intelligence-driven approach. In the hyper-competitive and rapidly innovating biopharma landscape, one of the most powerful—and often underutilized—sources of strategic intelligence is the global patent system. By systematically analyzing patent data, you can build a powerful early warning system that transforms your resilience posture from reactive to predictive.
The Patent Horizon: Using Competitive Intelligence for Strategic Risk Assessment
Why is patent data so valuable for risk assessment? Because it offers a unique, time-stamped window into your competitors’ most secret and strategic R&D activities.
Why Patent Data is a Powerful Early Warning System
In most jurisdictions, patent applications are published 18 months after they are first filed. This predictable timeline creates an incredible intelligence opportunity. It means you can see the technologies, molecular targets, and manufacturing processes your competitors are investing in years before a product ever enters clinical trials or appears in a press release.
This foresight allows you to move beyond reacting to market shifts and start anticipating them. It enables a proactive form of strategic risk assessment, allowing you to 86:
- Evaluate the potential impact of a competitor’s emerging technology on your existing product portfolio.
- Assess “freedom-to-operate” risks for your own pipeline products, identifying potential patent roadblocks long before they become costly legal battles.
- Identify opportunities to challenge or invalidate a competitor’s weak patents.
- Develop strategic contingency plans for the eventual market entry of a disruptive competitive product.
How to Use Patent Data for Risk Assessment with Tools like DrugPatentWatch
Manually sifting through millions of patent documents is an impossible task. This is where specialized competitive intelligence platforms become essential. Services like DrugPatentWatch aggregate, analyze, and organize this vast sea of data, making it accessible and actionable for strategic decision-making.86 A systematic approach to using such a tool for risk assessment involves several key activities:
- Monitoring Competitor Pipelines: You can set up automated alerts to notify you whenever a key competitor files a new patent in your therapeutic areas of interest. This provides a real-time feed of their R&D direction, allowing you to track their progress and anticipate their next moves.86
- Identifying Disruptive Technology Trends: By analyzing the patent landscape as a whole, you can identify broader technological shifts. Are competitors moving from small molecules to biologics for a particular class of targets? Are new drug delivery platforms or manufacturing technologies gaining traction? Spotting these trends early allows you to assess the risk of your own technology platform becoming obsolete and to plan your R&D investments accordingly.
- Assessing Supply Chain Risk: Patent data can even provide clues about future supply chain vulnerabilities. For example, if a competitor patents a novel, highly efficient manufacturing process for a key raw material that you also use, they could potentially dominate the supply or drive up prices, creating a strategic risk for your operations.
The Patent Cliff: Turning a Known Risk into a Strategic Opportunity
Perhaps the most well-known strategic risk in the pharmaceutical industry is the “patent cliff”—the dramatic and predictable loss of revenue that occurs when a blockbuster drug’s primary patent expires, opening the floodgates to low-cost generic competition.90 This is not an unknown “black swan” event; it is a known risk with a specific date.
Patent expiration data, which is meticulously tracked and made easily accessible by platforms like DrugPatentWatch, is therefore one of the most critical inputs for long-range financial and strategic planning. It allows an organization to quantify future revenue at risk—analysts project over $200 billion in revenue is at risk in the next five years alone—and develop proactive mitigation strategies long before the cliff arrives.54
These strategies, informed by patent intelligence, include:
- Strategic Pipeline Management: The most fundamental strategy is to ensure your R&D pipeline is robust enough to deliver new, innovative products that can replace the revenue from expiring blockbusters. Patent data helps you see where the scientific “white space” is and where competitors are not yet active.86
- Proactive Lifecycle Management: This involves finding ways to build on an existing product to generate new intellectual property. By developing and patenting new formulations (e.g., a long-acting injectable version), new methods of use for different diseases, or new combination therapies, companies can create a “patent thicket” that extends a product’s market exclusivity well beyond the original expiration date. This strategy, sometimes called “evergreening,” is a core part of modern pharma strategy.90
- Targeted M&A and In-Licensing: Patent landscape analysis is a powerful tool for corporate development. By mapping the patent activity in a therapeutic area, you can identify smaller biotech companies that have developed promising, strongly-patented technologies. This allows you to surgically target them for acquisition or in-licensing, bringing in external innovation to fill the gaps in your own pipeline before a patent cliff hits.86
Integrating this level of competitive and patent intelligence into your organization’s Enterprise Risk Management (ERM) framework is the hallmark of a truly mature and strategically resilient company. A traditional BCP prepares for a fire in your warehouse. A strategically resilient plan prepares for a competitor’s new drug launch five years from now. It means your risk register should contain not only operational risks (“-80°C Freezer Failure”) but also strategic risks identified through intelligence (“Competitor X patents novel CAR-T therapy targeting our lead indication,” or “Blockbuster Drug Y patent expires in Q3 2028”). This requires breaking down the silos between the Head of Risk, the Head of R&D, and the Head of Intellectual Property. In the modern biopharma landscape, patent strategy is risk management, and risk management must be informed by patent strategy.
Conclusion: Weaving a Resilient Future
We stand at a pivotal moment for the biomedical and research industry. The era of predictable, linear progress and stable, efficient systems has given way to a new reality defined by volatility, complexity, and unprecedented speed of change. In this environment, the old models of business continuity—static, siloed, and seen as a cost of doing business—are no longer sufficient. They are artifacts of a world that no longer exists.
The journey we have taken through this report demonstrates that true organizational resilience is something far more profound. It is a dynamic, integrated, and culturally embedded capability that must permeate every facet of the enterprise. It begins with a shift in mindset, reframing resilience not as a defensive shield but as a strategic enabler of growth, innovation, and trust.85
It is built on an architectural framework of anticipation, coping, and adaptation, fueled by a culture of continuous learning that is not afraid to challenge its own assumptions. It is operationalized through rigorous, data-driven methodologies like Business Impact Analysis and FMEA, which translate abstract risks into quantifiable priorities and justify intelligent investment.
This resilience extends deep into the value chain, fortifying the fragile lifelines of APIs, single-use technologies, and the cold chain against a backdrop of geopolitical and logistical uncertainty. It protects the very engine of innovation—the irreplaceable assets in our laboratories and the invaluable human subjects in our clinical trials—by embedding flexibility and patient-centricity into the core of R&D. And it recognizes the critical human element, mastering the narrative through transparent crisis communication to protect the organization’s most precious asset: its reputation.
Finally, the most forward-thinking organizations are pushing the boundaries even further, leveraging strategic intelligence from sources like the patent landscape to see over the horizon and prepare not just for the disruptions of today, but for the competitive and technological shifts of tomorrow.
Weaving this resilient future is not a simple task. It requires leadership commitment, cross-functional collaboration, and sustained investment. But the alternative—clinging to the brittle models of the past—is a far greater risk. For the biomedical and research organizations that embrace this holistic vision, resilience will become more than a plan. It will be the defining characteristic that allows them to navigate the storms ahead, deliver on their promises to patients, and lead the future of healthcare.
Key Takeaways
- Resilience is a Strategic Advantage, Not a Cost Center: Shift the organizational mindset from viewing business continuity as a defensive compliance activity to seeing it as a core driver of competitive advantage, market trust, and long-term value.
- Culture is the Foundation of Resilience: A company’s ability to anticipate, cope, and adapt is fundamentally determined by its culture. A culture of psychological safety, cross-functional collaboration, and organizational learning is more critical to resilience than any written plan.
- Integrate Frameworks for a Holistic Approach: Combine the management system structure of ISO 22301 with the patient-centric risk philosophy of ICH Q9 to create a single, unified resilience framework that is both operationally robust and regulatorily sound.
- Use Data-Driven Methodologies to Prioritize: Employ tools like Business Impact Analysis (BIA), FMEA, and HAZOP to move risk discussions from subjective to objective. Use the outputs (like Risk Priority Numbers) to justify investments in resilience and target resources where they will have the greatest impact.
- Focus on the Most Fragile Links in the Value Chain: Dedicate specific, robust strategies to de-risk the three most vulnerable areas of the biopharma supply chain: API sourcing, single-use technology dependencies, and cold chain logistics.
- Protect the Irreplaceable Assets of R&D: Develop highly specialized continuity protocols for laboratories and clinical trials. This includes detailed plans for -80°C freezer failures, vivarium disaster response, and ensuring patient safety and data integrity during trial disruptions.
- Master Crisis Communication and Stakeholder Engagement: Prepare a multi-channel crisis communication plan with pre-approved messaging tailored to key stakeholders (patients, HCPs, regulators, investors, employees). Proactive, transparent communication is essential for managing reputation, especially during a product recall.
- Leverage Intelligence for Proactive Risk Assessment: Integrate competitive intelligence, particularly from patent data platforms like DrugPatentWatch, into your Enterprise Risk Management framework. Use this foresight to anticipate competitive threats and strategic risks like the “patent cliff” years in advance.
Frequently Asked Questions (FAQ)
1. How can we get executive buy-in and secure funding for a comprehensive resilience program that goes beyond basic compliance?
Securing executive buy-in requires translating resilience from an operational concept into a strategic and financial one. Instead of focusing on the cost of the program, frame it as an investment that protects revenue and enables growth. Use the outputs of your Business Impact Analysis (BIA) and FMEA to quantify the potential financial losses from a disruption to a critical product line or the loss of a key R&D asset. Present case studies of competitors who suffered significant market share or reputational damage from a failure. Link resilience investments directly to strategic objectives, such as ensuring a successful product launch or entering a new market. Show how a resilient supply chain can become a competitive differentiator that attracts partners and customers. Ultimately, the argument is that the cost of building resilience is a fraction of the cost of a single, unmitigated catastrophic failure.
2. For a small biotech start-up with limited resources, what are the absolute most critical “first steps” to take in building a BCP?
For a resource-constrained start-up, the focus should be on the “80/20” rule—addressing the 20% of risks that could cause 80% of the damage. The critical first steps are:
- Identify Your Crown Jewels: What is the one thing that, if lost, would kill the company? This is likely your core intellectual property, your master cell bank, or your preclinical data.
- Protect Your Critical Assets: Your first investment should be in protecting these jewels. This means off-site, secure data backups and splitting your critical biological samples into at least two separate, geographically distinct freezers with independent power and remote temperature monitoring.
- Create a “Go-Bag” BCP: Develop a simple, actionable plan that includes an emergency contact list for all staff and key vendors, a communication plan for how you will reach everyone in a crisis, and clear instructions for who is responsible for what in your top 3-5 most likely disaster scenarios (e.g., power outage, lead scientist is unavailable).
- Know Your Key Suppliers: Identify your most critical suppliers (e.g., for a key reagent or CRO service) and have a conversation with them about their own BCP. At a minimum, know who your alternative options would be.
3. How do you test a BCP effectively without causing major disruption to ongoing operations?
Full-scale disaster simulations that involve shutting down operations are rare and often impractical. The most effective and common method for testing is the tabletop exercise. This is a guided discussion where the crisis management team and key stakeholders gather in a conference room to walk through a simulated crisis scenario (e.g., “Our main manufacturing site has been hit by a tornado,” or “We’ve just discovered a major data breach in our clinical trial database”). A facilitator presents the scenario and injects new information over time, forcing the team to work through their response plans, make decisions, and identify gaps, communication breakdowns, or flawed assumptions in their BCP—all without impacting real-world operations. These exercises are invaluable for building “muscle memory” and refining plans in a low-risk environment.
4. What is the role of AI and machine learning in the future of business continuity and risk sensing?
AI and machine learning (ML) are poised to revolutionize business continuity by enhancing the “anticipation” pillar of resilience. While traditional BCP is largely based on known risks, AI/ML can analyze vast, unstructured datasets to identify novel threats and predict disruptions before they occur. Potential applications include:
- Predictive Supply Chain Monitoring: AI algorithms can monitor global shipping data, weather patterns, social media, and news feeds to predict port slowdowns, supplier disruptions, or geopolitical instability that could impact your supply chain.41
- Advanced Cybersecurity: AI-powered security tools can detect anomalous patterns in network traffic that signal a sophisticated cyberattack in its earliest stages, allowing for a much faster response.
- Process Anomaly Detection: In manufacturing, ML models can monitor sensor data from equipment in real-time to predict potential failures before they happen, enabling proactive maintenance and preventing costly downtime.
- Automated BIA: AI could potentially automate parts of the BIA process by analyzing internal communications and operational data to identify critical processes and dependencies that might be missed by human analysis.
5. Our key single-use technology (SUT) supplier was just acquired by a major competitor. What are the immediate BCP actions we should take?
This is a significant strategic risk that requires immediate action. The BCP should trigger the following steps:
- Activate the Crisis/Risk Management Team: Assemble a cross-functional team including representatives from Supply Chain, Legal, Quality, Manufacturing, and Finance.
- Review All Contracts and Quality Agreements: The legal team must immediately review all existing agreements with the acquired supplier to understand your rights, supply guarantees, pricing terms, and any change-of-control clauses.
- Open Communication: Proactively reach out to your contacts at both the acquired supplier and the acquiring competitor. Seek assurances of supply continuity and clarification on their future plans. Document everything.
- Accelerate Second-Source Qualification: If you have a qualified second source, immediately increase your orders with them to begin building a safety stock. If you do not have one, qualifying an alternative supplier becomes the number one priority for your supply chain and quality teams.
- Conduct an Urgent Risk Assessment: Perform a rapid FMEA on the situation. What are the failure modes? (e.g., Competitor de-prioritizes your orders, raises prices exorbitantly, discontinues your specific assembly). Assess the severity and likelihood and develop immediate mitigation plans. This situation highlights why proactive supplier risk management and dual-sourcing are critical components of a resilient supply chain.
References
- Ensuring Business Continuity in Your Pharmaceutical Commercial …, accessed July 28, 2025, https://www.pharm-int.com/resources/ensuring-business-continuity-in-your-pharmaceutical-commercial-supply/
- Business Continuity in Pharma: the role of Risk Management – ValGenesis, accessed July 28, 2025, https://www.valgenesis.com/blog/business-continuity-in-pharma-the-role-of-risk-management
- Building Resilient Pharma Supply Chains in an Uncertain World, accessed July 28, 2025, https://www.pharmasalmanac.com/articles/building-resilient-pharma-supply-chains-in-an-uncertain-world
- Healthcare Supply Chain Resilience: Lessons Learned from the Pandemic and Strategies for the Future – News-Medical.net, accessed July 28, 2025, https://www.news-medical.net/health/Healthcare-Supply-Chain-Resilience-Lessons-Learned-from-the-Pandemic-and-Strategies-for-the-Future.aspx
- Organizational Resilience in Healthcare Organizations: A Research in the Public and Private Sector – ResearchGate, accessed July 28, 2025, https://www.researchgate.net/publication/361428291_Organizational_Resilience_in_Healthcare_Organizations_A_Research_in_the_Public_and_Private_Sector
- Building Organizational Resilience Through … – Frontiers, accessed July 28, 2025, https://www.frontiersin.org/journals/communication/articles/10.3389/fcomm.2022.837386/full
- Organizational resilience in healthcare: a review and descriptive narrative synthesis of approaches to resilience measurement and assessment in empirical studies – PubMed Central, accessed July 28, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10113996/
- Business Continuity Planning to Prevent Drug Shortages …, accessed July 28, 2025, https://ispe.org/pharmaceutical-engineering/january-february-2021/business-continuity-planning-prevent-drug
- Enhancing Organizational Resilience: The Transformative Influence of Strategic Human Resource Management Practices and Organizational Culture – MDPI, accessed July 28, 2025, https://www.mdpi.com/2071-1050/16/10/4315
- Risk assessment strategies for life sciences manufacturing – CRB Group, accessed July 28, 2025, https://www.crbgroup.com/insights/risk-assessment-strategies-for-life-sciences-manufacturing
- ISO 22301 | Business Continuity Management Systems – Intertek, accessed July 28, 2025, https://www.intertek.com/assurance/iso-22301/
- What is the ISO 22301 standard and what is it for? – GlobalSuite Solutions, accessed July 28, 2025, https://www.globalsuitesolutions.com/what-is-iso22301-standard-what-is-its-purpose/
- ISO 22301 – The Business Continuity Management Standard | ISMS …, accessed July 28, 2025, https://www.isms.online/iso-22301/
- ISO 22301 Certification | A-LIGN Compliance & Assessments, accessed July 28, 2025, https://www.a-lign.com/service/iso-22301
- ISO 22301 Business Continuity – New version 2019 | GSS – GlobalSuite Solutions, accessed July 28, 2025, https://www.globalsuitesolutions.com/iso-22301-business-continuity-new-version-2019/
- Risk Management in Life Sciences: Proactive QMS Strategies – PSC Software, accessed July 28, 2025, https://pscsoftware.com/mastering-risk/
- Q9 Briefing Pack – ICH, accessed July 28, 2025, https://ich.org/page/q9-briefing-pack
- Best Practices in Quality Risk Management for Life Sciences Professionals, accessed July 28, 2025, https://srg4people.com/best-practices-in-quality-risk-management-for-life-sciences-professionals/
- How to Conduct a Business Impact Analysis – Riskonnect, accessed July 28, 2025, https://riskonnect.com/business-continuity-resilience/how-to-conduct-a-business-impact-analysis/
- What Is Business Impact Analysis (BIA)? [2025] – Asana, accessed July 28, 2025, https://asana.com/resources/business-impact-analysis
- Business Impact Analysis | Ready.gov, accessed July 28, 2025, https://www.ready.gov/business/planning/impact-analysis
- Business Impact Analysis, accessed July 28, 2025, https://cdn.ttgtmedia.com/searchSecurityChannel/downloads/443_Disaster_04_(2).pdf
- Guide for Lab Research Continuity Planning – Emergency, accessed July 28, 2025, https://emergency.wwu.edu/docs/Guide_for_%20Lab_Research_Continuity_Planning.docx
- Guidance for Performing Failure Mode and Effects Analysis with Performance Improvement Projects – CMS, accessed July 28, 2025, https://www.cms.gov/medicare/provider-enrollment-and-certification/qapi/downloads/guidanceforfmea.pdf
- Business Impact Analysis – WWT, accessed July 28, 2025, https://www.wwt.com/assessment/business-impact-analysis
- Business Continuity Plans and FAQs – Office of Research – University of Alabama at Birmingham, accessed July 28, 2025, https://www.uab.edu/research/home/business-continuity-plan
- Business Continuity for Laboratories and Research Facilities | Emergency Management, accessed July 28, 2025, https://emergency.yale.edu/planning/business-continuity-planning/laboratories-research-facilities
- Data Integrity in Clinical Research | CCRPS, accessed July 28, 2025, https://ccrps.org/clinical-research-blog/data-integrity-in-clinical-research
- What is FMEA? Failure Mode & Effects Analysis – ASQ, accessed July 28, 2025, https://asq.org/quality-resources/fmea
- Failure Modes and Effects Analysis (FMEA), accessed July 28, 2025, https://www.med.unc.edu/ihqi/wp-content/uploads/sites/463/2022/02/QIToolkit_FailureModesandEffectsAnalysis-2.pdf
- FMEA: A process for risk assessment in the pharmaceutical industry – Bachem, accessed July 28, 2025, https://www.bachem.com/articles/blog/fmea-a-process-for-risk-assessment/
- HAZOP Guide, accessed July 28, 2025, https://pqri.org/wp-content/uploads/2015/08/pdf/HAZOP_Training_Guide.pdf
- What is HAZOP? Hazard and Operability Study | SafetyCulture, accessed July 28, 2025, https://safetyculture.com/topics/hazop/
- What is Recovery Time Objective (RTO) and How to Calculate It | Blog – Commvault, accessed July 28, 2025, https://www.commvault.com/blogs/what-is-recovery-time-objective-rto-and-how-to-calculate-it
- What Is Recovery Time Objective? – Comarch, accessed July 28, 2025, https://www.comarch.com/trade-and-services/ict/knowledge/what-is-recovery-time-objective/
- What is Recovery Time Objective (RTO)? – ilert, accessed July 28, 2025, https://www.ilert.com/glossary/what-is-recovery-time-objective-rto
- What Is a Recovery Time Objective? – JumpCloud, accessed July 28, 2025, https://jumpcloud.com/it-index/what-is-a-recovery-time-objective
- Recovery time objective: What it is and how to improve it – Rewind Backups, accessed July 28, 2025, https://rewind.com/blog/recovery-time-objective-what-it-is-and-how-to-improve-it/
- Current Risk in the Supply Chain for the Active Pharmaceutical Ingredients Business | Universal Journal of Pharmacy and Pharmacology – Scientific Publications, accessed July 28, 2025, https://www.scipublications.com/journal/index.php/ujpp/article/view/906
- Operational Risk Management in Global Supply Scenarios | Pharmaceutical Engineering, accessed July 28, 2025, https://ispe.org/pharmaceutical-engineering/november-december-2020/operational-risk-management-global-supply
- BioPharma Outlook: 2025+ Supply Chain Resilience for Global Health, accessed July 28, 2025, https://www.leading-minds-network.com/en/article/2025-supply-chain-resilience-for-global-health
- Minimizing API Supply Chain Risks – AbbVie Contract Manufacturing, accessed July 28, 2025, https://www.abbviecontractmfg.com/news-and-insights/minimizing-api-supply-chain-risks.html
- Expert guide: Single-use supply chain risk management – Cleanroom Technology, accessed July 28, 2025, https://cleanroomtechnology.com/expert-guide-single-use-supply-chain-risk-management-148917
- Risk Management Practices To Address Pharmaceutical Sourcing Challenges, accessed July 28, 2025, https://lgmpharma.com/blog/risk-management-practices-to-address-pharmaceutical-sourcing-challenges/
- Key Concepts Driving The Future Of Single-Use In Biopharmaceutical Production, accessed July 28, 2025, https://www.advancingrna.com/doc/key-concepts-driving-the-future-of-single-use-in-biopharmaceutical-production-0001
- From Niche to Necessity: How Single-Use Transformed Biomanufacturing, accessed July 28, 2025, https://www.pharmasalmanac.com/articles/from-niche-to-necessity-how-single-use-transformed-biomanufacturing
- Biopharma Supply Chain Resilience → Term – Fashion → Sustainability Directory, accessed July 28, 2025, https://fashion.sustainability-directory.com/term/biopharma-supply-chain-resilience/
- Biologic Medications and the Specialty Pharmacy – Sensitech, accessed July 28, 2025, https://www.sensitech.com/zh/media/BioMed_Specialty_Pharma_WP_Web_28Feb2019_tcm971-132240.pdf
- Critical Role of Cold Chain Logistics – Patheon pharma services, accessed July 28, 2025, https://www.patheon.com/us/en/insights-resources/blog/critical-role-of-cold-chain-logistics.html
- Building Resilience in Life Science Supply Chains – Biocair, accessed July 28, 2025, https://www.biocair.com/en/blog/building-resilience-in-life-science-supply-chains?hsLang=en
- Pharma’s Simplification Imperative: From McKinsey’s Vision to Implementation Reality, accessed July 28, 2025, https://medium.com/@laurence.grisel/pharmas-simplification-imperative-from-mckinsey-s-vision-to-implementation-reality-c8bfe20a4a19
- Simplification for success: Rewiring the biopharma operating model | McKinsey, accessed July 28, 2025, https://www.mckinsey.com/industries/life-sciences/our-insights/simplification-for-success-rewiring-the-biopharma-operating-model
- Emerging from disruption: The future of pharma operations strategy – McKinsey, accessed July 28, 2025, https://www.mckinsey.com/capabilities/operations/our-insights/emerging-from-disruption-the-future-of-pharma-operations-strategy
- Trends Shaping Biopharma in 2025 | Deloitte US, accessed July 28, 2025, https://www.deloitte.com/us/en/Industries/life-sciences-health-care/blogs/health-care/trends-shaping-biopharma.html
- Pharma Supply Chains in Digitalisation Push – Deloitte Study, accessed July 28, 2025, https://supplychaindigital.com/digital-supply-chain/pharma-supply-chains-in-digitalisation-push-deloitte-study
- Biopharma Embraces Supply Chain Digitalization: Deloitte Survey, accessed July 28, 2025, https://supplychain360.io/biopharma-embraces-supply-chain-digitalization-deloitte-survey/
- Digitalized supply chains are essential to biopharma’s future – Deloitte, accessed July 28, 2025, https://www2.deloitte.com/us/en/insights/industry/health-care/end-to-end-digitalization-of-biopharma-supply-chain.html
- Freezer Maintenance Guidelines – BusFin@osu.edu – The Ohio State University, accessed July 28, 2025, https://busfin.osu.edu/sites/default/files/freezer_maintenance_guidelines_2021.pdf
- Laboratory Freezers | Environmental Health and Safety | The University of Vermont, accessed July 28, 2025, https://www.uvm.edu/safety/laboratory-freezers
- Fridge and Freezer Safety | NSTA, accessed July 28, 2025, https://www.nsta.org/blog/fridge-and-freezer-safety
- Research Continuity Planning Guide, accessed July 28, 2025, https://researchservices.cornell.edu/news/research-continuity-planning-guide
- Business Continuity Planning: Ensure Your Laboratory is Prepared for a Crisis, accessed July 28, 2025, https://eheinc.com/insights/blog/business-continuity-planning-ensure-your-laboratory-is-prepared-for-a-crisis/
- Disaster Planning with Animals | National Agricultural Library – USDA, accessed July 28, 2025, https://www.nal.usda.gov/animal-health-and-welfare/disaster-planning-animals
- Disaster Resilience and Animal Research Programs – NCBI, accessed July 28, 2025, https://www.ncbi.nlm.nih.gov/books/NBK464167/
- Emergency and Disaster Plan for Animal Facilities | Research, Scholarship, Innovation, and Creativity, accessed July 28, 2025, https://research.olemiss.edu/disaster-plan
- Catastrophic Disruptions in Clinical Trials | Circulation – American Heart Association Journals, accessed July 28, 2025, https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.060541
- Catastrophic Disruptions in Clinical Trials – American Heart Association Journals, accessed July 28, 2025, https://www.ahajournals.org/doi/pdf/10.1161/CIRCULATIONAHA.122.060541
- Patient Safety in Clinical Trials: A CRWF Guide (2025), accessed July 28, 2025, https://www.crwf.com/blog/why-patient-safety-matters-in-clinical-trials/
- Business Continuity Planning for Investigative Sites – Avoca, a WCG company, accessed July 28, 2025, https://www.theavocagroup.com/business-continuity-planning-for-investigative-sites/
- How to Ensure Data Integrity in Clinical Research: A Step-by-Step Guide – bioaccess, accessed July 28, 2025, https://www.bioaccessla.com/blog/how-to-ensure-data-integrity-in-clinical-research-a-step-by-step-guide
- Ensuring Data Integrity in Clinical Trials: Key Considerations – JAF Consulting, Inc., accessed July 28, 2025, https://jafconsulting.com/blog/ensuring-data-integrity-in-clinical-trials-key-considerations/
- What Is Data Integrity in Clinical Trials and Why It Matters | Power, accessed July 28, 2025, https://www.withpower.com/guides/data-integrity-in-clinical-trials
- Guidance for Industry – COMPUTERIZED SYSTEMS USED IN CLINICAL TRIALS | FDA, accessed July 28, 2025, https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/fda-bioresearch-monitoring-information/guidance-industry-computerized-systems-used-clinical-trials
- Business Continuity and Disaster Recovery in FDA-Regulated Industries – ValGenesis, accessed July 28, 2025, https://www.valgenesis.com/blog/business-continuity-and-disaster-recovery-in-fda-regulated-industries
- Cybersecurity threats in clinical trials – Paubox, accessed July 28, 2025, https://www.paubox.com/blog/cybersecurity-threats-in-clinical-trials
- Best Practices for Sponsors to Ensure Data Integrity in Clinical Research – Zenovel, accessed July 28, 2025, https://zenovel.com/sponsors-to-ensure-data-integrity-in-clinical-research/
- How to Create a Crisis Communication Plan – Everbridge, accessed July 28, 2025, https://www.everbridge.com/blog/crisis-communication-plan/
- Crisis Management Strategies for Pharmaceutical Firms – Maple Valley Pharmacy, accessed July 28, 2025, https://www.maplevalleyrx.com/crisis-management-strategies-for-pharmaceutical-firms.html
- Effectively Communicating with Stakeholders in a Crisis – APCO Worldwide, accessed July 28, 2025, https://apcoworldwide.com/blog/effectively-communicating-with-stakeholders-in-a-crisis/
- Crisis Communication in the Pharmaceutical Industry: PR Strategies for Drug Recalls and Safety Issues – Gayle Pohl Iowa, accessed July 28, 2025, https://gaylepohliowa.com/crisis-communication-in-the-pharmaceutical-industry-pr-strategies-for-drug-recalls-and-safety-issues/
- Engaging Stakeholders in Pharmaceutical Company Decisions, accessed July 28, 2025, https://www.maplevalleyrx.com/engaging-stakeholders-in-pharmaceutical-company-decisions.html
- Product Recalls and Firm Reputation: – CUNY Graduate Center, accessed July 28, 2025, https://www.gc.cuny.edu/sites/default/files/2021-07/recalls-final.pdf
- Treating the Symptoms of a Drug Recall – Marsh, accessed July 28, 2025, https://www.marsh.com/content/dam/marsh/Documents/PDF/asia/en_asia/Life_Sciences_Risk_Study_Aug2018.pdf
- The Liability of Good Reputation: A Study of Product Recalls in the U.S. Automobile Industry, accessed July 28, 2025, https://pubsonline.informs.org/doi/10.1287/orsc.1050.0175
- Meeting the Moment: ESG Strategy and the Business of Resilience, accessed July 28, 2025, https://www.pharmexec.com/view/meeting-the-moment-esg-strategy-and-the-business-of-resilience
- How to Track Competitor R&D Pipelines Through Drug Patent Filings – DrugPatentWatch, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/how-to-track-competitor-rd-pipelines-through-drug-patent-filings/
- Patent research as a tool for competitive intelligence in brand protection – RWS, accessed July 28, 2025, https://www.rws.com/blog/patent-research-as-a-tool/
- DrugPatentWatch not only saved us valuable time in tracking patent …, accessed July 28, 2025, https://www.drugpatentwatch.com/
- Competitive Intelligence & Market Analysis | Juristat – Patent Analytics, accessed July 28, 2025, https://resources.juristat.com/competitive-intelligence
- The Impact of Patent Expirations on SEC Filings and Investor Relations – PatentPC, accessed July 28, 2025, https://patentpc.com/blog/the-impact-of-patent-expirations-on-sec-filings-and-investor-relations
- Understanding the Financial Implications of Patent Expirations – Qualifyze, accessed July 28, 2025, https://www.qualifyze.com/resources/understanding-the-financial-implications-of-patent-expirations/
- The Impact of Drug Patent Expiration: Financial Implications, Lifecycle Strategies, and Market Transformations – DrugPatentWatch, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/the-impact-of-drug-patent-expiration-financial-implications-lifecycle-strategies-and-market-transformations/
- Leading resilience by example: Not your average inspirational poster quote | BCI, accessed July 28, 2025, https://www.thebci.org/news/leading-resilience-by-example-not-your-average-inspirational-poster-quote.html