Executive Summary
The escalating costs of biologic therapies present a significant and growing financial burden on patients, often leading to medication non-adherence and adverse health outcomes. Biosimilars, highly similar and equally effective versions of approved biologic drugs, offer a powerful solution to this challenge by introducing competition and driving down prices. While biosimilars have already generated substantial system-wide savings, their full potential for directly reducing individual patient out-of-pocket costs remains largely untapped. This report provides a comprehensive analysis of how biosimilars impact patient financial burdens, examining the mechanisms of cost reduction, proven real-world impacts, and the multifaceted barriers hindering greater patient savings. It concludes with actionable recommendations for various stakeholders to accelerate biosimilar adoption and ensure these benefits are fully realized by patients.
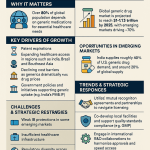
Key findings indicate that biosimilars primarily reduce costs through market competition, which lowers prices for both biosimilars and their reference products. This competition has led to significant savings in therapeutic areas such as oncology, immunology, and diabetes, improving patient access and adherence. However, widespread adoption and patient-level savings are impeded by a lack of education among healthcare professionals and patients, misaligned financial incentives within the healthcare system (including provider reimbursement models and pharmacy benefit manager rebate practices), and regulatory complexities such as patent litigation and the nuanced distinction between biosimilarity and interchangeability in the United States.
To maximize the benefits of biosimilars for patients, primary recommendations include implementing policy reforms to streamline approval processes and address patent thickets, fostering a unified standard for interchangeability, and legislating against copay accumulator programs. Furthermore, targeted education and awareness initiatives for both healthcare providers and patients are crucial to build confidence and overcome hesitancy. Finally, realigning financial incentives for payers and providers to reward the use of lower-cost biosimilars, alongside promoting a more competitive and transparent market, will be essential to ensure that the economic advantages of biosimilars directly translate into reduced out-of-pocket costs and enhanced access to life-changing therapies for patients.
1. Introduction: The Growing Burden of Biologic Costs and the Promise of Biosimilars
The Escalating Cost of Biologic Therapies
Biologic drugs represent a revolutionary advancement in medicine, offering life-changing treatments for a wide array of chronic and life-threatening conditions, including various cancers, autoimmune diseases like rheumatoid arthritis and Crohn’s disease, and diabetes.1 Despite their profound clinical benefits, these therapies come with exceptionally high price tags, contributing disproportionately to healthcare expenditures. In the United States, biologics, while accounting for a mere 2% of all prescriptions, consumed between 37% and 46% of net drug spending in 2021.1 By 2023, this share remained substantial, representing 38-40% of all pharmaceutical spending in the U.S. and 40% (€87.6 billion) in the European Union.5
The financial burden on individual patients is considerable. Annual out-of-pocket costs for biologic therapies can range from approximately $3,000 to $5,000 for conditions such as asthma and allergies, escalate to $10,000 to $30,000 for arthritis treatments, and can reach upwards of $100,000 or even $500,000 per year for certain oncology indications.1 This exorbitant cost frequently leads to significant financial toxicity for patients, a phenomenon characterized by the substantial economic burden and psychological distress associated with high healthcare expenses.9 The consequences are dire: studies indicate that high out-of-pocket costs are a primary driver of financial stress, often compounded by indirect expenses such as lost income and insurance-related barriers like high co-payments and limited reimbursement.11 A 2022 survey revealed that one in nine Medicare beneficiaries did not fill a physician’s prescription due to an inability to afford the medication, highlighting the direct link between cost and non-adherence.1 This non-adherence can lead to poorer health outcomes and, paradoxically, increased overall healthcare system costs in the long run due to complications arising from untreated or undertreated conditions.8
The inherent complexity and expensive development processes of biologics directly translate into these high list prices. Biologics are large, intricate molecules derived from living organisms, requiring specialized materials, equipment, and extensive research, development, and testing, often spanning a decade and costing billions of dollars to bring a single drug to market.7 This significant upfront investment is subsequently passed on to hospitals and, ultimately, to patients through high out-of-pocket costs.7 This direct causal relationship means that the initial high cost is not merely a financial inconvenience but has profound negative clinical consequences for patients and downstream economic effects for the broader healthcare system, as managing complications from non-adherence can be more expensive than the original treatment.
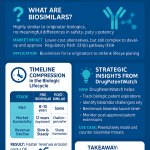
Defining Biosimilars
In response to the escalating costs of biologic drugs, biosimilars have emerged as a vital component of modern pharmaceutical innovation. A biosimilar is defined as a biological drug that is “very much like” an already approved reference biological drug, having demonstrated no clinically meaningful differences in terms of safety, purity, and potency.2 To receive approval from regulatory bodies like the U.S. Food and Drug Administration (FDA) or the European Medicines Agency (EMA), a biosimilar must be shown to be as safe, work as well as, and work in the same way as its reference drug, and must be used at the same dose and for the same conditions.14
It is crucial to differentiate biosimilars from generic drugs. While both offer more affordable alternatives to their brand-name counterparts, their fundamental nature differs significantly. Generic drugs are chemically synthesized small molecules with simple, identical structures to their reference products.20 Biosimilars, conversely, are complex large molecules produced from living organisms, which inherently introduces natural variability, similar to the variations observed between different batches of the originator biologic itself.2 Therefore, biosimilars are not exact copies but “highly similar” versions of originator biologics.16
The Promise of Affordability and Access
The introduction of biosimilars into the market, typically occurring after the patent expiration of the originator biologic, heralds a new era of affordability and expanded access to essential treatments.4 They are considered a powerful solution for fostering price competition and enhancing the affordability of biologic therapies, thereby increasing patient access to critical medications.2
The potential for cost savings from biosimilars is substantial. Estimates suggest that biosimilars could reduce healthcare spending by $54 billion between 2017 and 2026 8, with other projections indicating savings of $104 billion between 2020 and 2024 and $124 billion between 2021 and 2025 in the U.S. healthcare system.2 Since their initial introduction in 2015, biosimilars have already generated $36 billion in savings 27, demonstrating their proven capacity to lower healthcare expenditures. This financial relief is not just a theoretical benefit; it translates into tangible improvements in patient access and the sustainability of healthcare systems globally.
2. Regulatory Pathways and Market Dynamics
Rigorous Approval Processes (FDA and EMA)
The development and approval of biosimilars are governed by rigorous regulatory frameworks established by leading agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). Both agencies evaluate each biosimilar on a case-by-case basis, ensuring that these products are as safe, effective, and of the same high quality as their reference biologics.14 This stringent evaluation process is a cornerstone of regulatory oversight for all biological products.
The development pathway for biosimilars is abbreviated compared to that of originator biologics. This abbreviated approach allows biosimilar manufacturers to rely, in part, on the FDA’s or EMA’s previous findings of safety and effectiveness for the reference product.2 The process begins with a comprehensive comparison of the analytical characteristics between the biosimilar and the reference product, forming the foundation of biosimilar development.15 Depending on the analytical findings, additional studies, such as animal studies, clinical pharmacology studies (to assess how the product moves through the body and its effects), and, if necessary, comparative clinical studies, may be required to confirm that there are no clinically meaningful differences.2 This tailored procedure, which focuses on demonstrating “biosimilarity” rather than independently establishing safety and effectiveness from scratch, generally leads to reduced development costs and faster market access for biosimilars.15
The rigorous regulatory scrutiny applied to biosimilars, while sometimes perceived as a burdensome process for manufacturers due to the extensive studies required 1, is in fact a critical foundation for their market acceptance and patient confidence. This high standard ensures that healthcare professionals and patients can trust the therapeutic equivalence of biosimilars to their reference products.16 Without this robust demonstration of similarity, widespread adoption would be significantly hampered, thereby undermining the potential for cost savings. Thus, the demanding nature of the approval process, far from being a mere impediment, is essential for building the trust necessary for biosimilars to fulfill their promise of affordability and access.
Biosimilarity vs. Interchangeability
A key distinction in the biosimilar landscape, particularly in the United States, lies between “biosimilarity” and “interchangeability.” Biosimilarity signifies that a product is highly similar to its reference product with no clinically meaningful differences in terms of safety, purity, and potency.2 This is the foundational requirement for all biosimilar approvals.
Interchangeability, on the other hand, is an additional regulatory designation in the U.S. that allows a biosimilar to be substituted for its reference product at the pharmacy level without the intervention of the prescribing healthcare professional, much like generic drugs are routinely substituted for brand-name medications.18 To achieve this designation, manufacturers must provide additional data demonstrating that switching between the interchangeable biosimilar and the reference product does not increase safety risks or decrease effectiveness.15 This often involves specific switching studies where patients alternate between the two products multiple times.19
In contrast to the U.S. approach, the European Medicines Agency (EMA) and the Heads of Medicines Agencies (HMA) have issued a joint statement confirming that all biosimilar medicines approved in the European Union (EU) are considered interchangeable from a scientific viewpoint.16 This means that a biosimilar can be used instead of its reference product, or vice versa, based on scientific evidence of their comparability, harmonizing the EU approach and providing greater clarity for healthcare professionals.16
The distinction and low rate of interchangeability designation in the U.S. currently acts as a significant systemic barrier to patient access and cost savings. As of November 2023, only seven biosimilars had received interchangeability designations in the U.S..46 This means that, unlike in the EU, pharmacists in most U.S. states cannot automatically substitute a biosimilar for a reference product without physician intervention, unless it has the specific interchangeable designation.18 This regulatory nuance directly translates into administrative hurdles, potential delays in access to lower-cost options, and reduced pharmacist-driven substitution, thereby diminishing the immediate out-of-pocket savings for patients. Some companies may not seek this designation for business reasons or if the medication is primarily administered in a hospital or clinic setting where pharmacy-level substitution is less relevant.18
Patent Exclusivity and Litigation
The market entry of biosimilars is heavily influenced by the intellectual property landscape surrounding originator biologics. Reference biologics are protected by patents for several years, a period intended to allow manufacturers to recoup their substantial research and development costs.1 In the U.S., the Biologics Price Competition and Innovation Act (BPCIA) of 2010 grants originator biologics 12 years of market exclusivity, during which competing biosimilars cannot be marketed.1
Beyond this initial exclusivity, patent thickets—numerous secondary patents covering aspects like methods of use, manufacturing, or formulation—can further extend monopoly rights and significantly delay biosimilar market entry.45 The BPCIA’s complex patent litigation framework, often referred to as the “patent dance,” can involve lengthy legal battles, potentially preventing biosimilars from entering the market even after primary patents expire.23 Biosimilar manufacturers often face the challenge of initiating patent litigation to clear weak or invalid patents only after submitting their Biologic License Application to the FDA, which occurs after extensive and costly clinical trials.48 This can lead to delays and uncertainty, as branded drug companies may seek preliminary injunctions to maintain market exclusivity during litigation.48
The interplay of patent exclusivity, patent thickets, and the BPCIA’s litigation framework creates a prolonged period of monopoly for originator biologics.1 This legal landscape, while ostensibly intended to incentivize innovation, inadvertently stifles timely biosimilar competition. The consequence of this is an artificial inflation of drug prices and a delay in the realization of significant out-of-pocket cost reductions for patients. However, it is worth noting that patent settlements between brand and generic/biosimilar manufacturers have been shown to accelerate patient access to these medicines by an average of over five years before patent expiration, highlighting a potential avenue for mitigating these delays.49
3. Mechanisms of Out-of-Pocket Cost Reduction
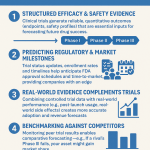
Competition Driving Down Prices
The introduction of biosimilars into the pharmaceutical market fundamentally alters the competitive landscape, serving as the most proven method to lower drug prices.1 This competitive dynamic is not merely about the biosimilar being a cheaper alternative; it exerts significant downward pressure on the prices of both the biosimilar itself and its corresponding brand biologic.26 For instance, competition from biosimilars has been observed to reduce the average sales price of their corresponding brand biologics by an average of 25%.39
The primary mechanism by which biosimilars reduce patient out-of-pocket costs is not solely their lower launch price, but the competitive pressure they exert on the entire market, including the originator product. This dynamic creates a “race to the bottom” in pricing, directly translating to lower base costs which then reduce patient cost-sharing amounts. Biosimilars typically launch with an average sales price that is 50% less than the reference brand biologic at the time of launch 39, with overall price reductions ranging from 15-30% or more.29 In some notable cases, biosimilars have launched with even steeper discounts, such as the first biosimilar version of Stelara, which entered the market at prices as much as 80-90% less than the brand 50, or biosimilar insulin Semglee, which launched at a 65% discount compared to Lantus.31 When the underlying wholesale acquisition cost (WAC) of both the brand and its biosimilar drops, the patient’s percentage-based cost-sharing (coinsurance) or fixed copayments (which are often tiered based on price) also decrease, leading to direct out-of-pocket savings.
Influence of Pharmacy Benefit Managers (PBMs) and Formulary Design
Pharmacy Benefit Managers (PBMs) play a pivotal role in shaping insurance formularies and preferred drug lists, which directly influence patient access to medications and their associated out-of-pocket costs.31 PBMs have the power to rapidly shift prescribing patterns through decisive formulary exclusion policies, leading to substantial cost savings for the healthcare system. A notable example is CVS Caremark’s decision to remove reference biologic adalimumab from its national commercial template formularies, which resulted in 97% of prescriptions being filled with preferred biosimilars.55 This demonstrates the significant leverage PBMs can wield in accelerating biosimilar adoption.
However, the underlying rebate system can create a systemic disincentive for PBMs to prioritize the lowest-cost option for patients. PBMs often receive higher rebates for placing higher-cost reference medicines on formularies, creating a “perverse incentive” to favor these originators over less expensive biosimilars.5 This practice can limit biosimilar formulary access despite their lower upfront costs. This means that even when a cheaper biosimilar exists, patients may not see the full benefit in their out-of-pocket costs if their plan’s formulary is structured to favor higher-rebate, higher-list-price brand drugs, effectively transferring the “savings” from the patient to the payer or PBM. This critical systemic barrier can prevent the full translation of biosimilar price reductions into direct patient savings.
Impact on Patient Cost-Sharing
The competitive pressure exerted by biosimilars generally translates into lower out-of-pocket costs for patients, including reduced copayments and coinsurance.4 For example, a rheumatoid arthritis patient’s annual copay could decrease from $5,000 to $3,000 with a biosimilar.26 Similarly, a breast cancer patient reported an immediate saving, with her copayment falling to $25 from hundreds after switching to a biosimilar.53 These direct savings can significantly alleviate the financial burden on individuals.
Furthermore, policy changes aim to cap patient out-of-pocket expenses. Beginning in 2025, Medicare beneficiaries with Part D coverage will have their annual out-of-pocket costs limited to $2,000, a measure projected to save nearly 19 million enrollees an average of $400 each year.13 This cap directly benefits patients by providing a predictable ceiling on their annual drug expenditures.
However, while biosimilars inherently offer lower list prices, the actual out-of-pocket savings for patients are significantly mediated by their insurance benefit design, particularly the presence of copay accumulator programs.60 These programs, often implemented by PBMs, prevent copay assistance provided by drug manufacturers from counting towards a patient’s annual deductible and out-of-pocket maximums.60 This means that even if a patient receives financial assistance to cover their copay for a biosimilar, that assistance may not help them meet their deductible or reach their out-of-pocket limit, forcing them to bear the full cost of the deductible later in the year.60 This systemic financial structure can directly undermine the patient-level benefits of biosimilar price reductions, creating unexpected financial burdens even when patients choose a lower-cost alternative. Recognizing this issue, legislation to ban these programs has been passed in 25 states, the District of Columbia, and Puerto Rico, requiring insurers to count copay assistance towards cost-sharing limits.60
4. Real-World Impact: Case Studies and Patient Outcomes
Overall System-Wide Savings
The introduction and increasing adoption of biosimilars have yielded substantial savings for healthcare systems globally. In the United States, generic and biosimilar medicines collectively generated a record $408 billion in savings for patients and the healthcare system in 2022, increasing to $445 billion in 2023.27 Since their initial entry into the market in 2015, biosimilars alone have contributed $36 billion in cumulative savings.27
These savings are particularly striking when considering the volume of prescriptions. Generics and biosimilars account for approximately 90% of all U.S. prescriptions filled, yet they represent only 13-17.5% of the country’s total prescription drug spending.27 This disproportionately high volume of prescriptions filled by generics and biosimilars relative to their share of total drug spending indicates that these medications are crucial for the sustainability of the healthcare system. Without these lower-cost alternatives, the financial burden of biologics would be even more unsustainable, potentially limiting access to innovative therapies for a broader patient population. This highlights that biosimilars are not just a cheaper alternative but a fundamental component of financial stability for healthcare systems, enabling them to continue funding expensive, innovative therapies and expanding access to necessary treatments.5
Specific Therapeutic Area Examples
Biosimilars have demonstrated significant cost-saving potential across various therapeutic areas, directly benefiting patients and healthcare systems.
- Oncology: Biosimilars have played a critical role in reducing the financial burden of cancer care. In 2021, the use of biosimilars generated over $17 billion in oncology savings, with the latest wave of oncology biosimilars contributing more than $2.4 billion in savings for treatments of brain, breast, cervical, colorectal, kidney, lung, and stomach cancers, as well as leukemia and non-Hodgkin lymphoma.53 Biosimilar competition has notably cut oncology spending growth in half since 2019.53 Specific examples include trastuzumab biosimilars, which slashed prices by up to 82% within three years of launch, and bevacizumab biosimilars, which also significantly reduced costs.26
- Immunology (e.g., Rheumatoid Arthritis, Crohn’s Disease): In the realm of immune-mediated inflammatory diseases, biosimilars have also delivered substantial savings. Infliximab biosimilars, for instance, have saved Canadians almost 50% compared to the originator product, Remicade.22 Adalimumab biosimilars, addressing one of healthcare’s highest drug expenditures, offer significant potential for cost reduction.61 Mandatory biosimilar substitution policies, such as for infliximab in Ontario, Canada, could yield savings of up to $645.9 million over three years.26
- Diabetes (Insulin): The introduction of biosimilar insulins, such as Semglee, has brought steep discounts, with Semglee launching at a 65% discount compared to its reference product, Lantus.31 Experts project that a competitive biosimilar insulin market could potentially reduce the annual cost of insulin for patients to $130 or less.31
- Supportive Care: Biosimilars in supportive care have seen particularly high adoption rates. Filgrastim biosimilars achieved 84.8% adoption, epoetin alfa 76.2%, and pegfilgrastim 52.6%.61 These biosimilars demonstrated mean wholesale acquisition cost reductions ranging from 35% to 55% compared to their reference products.61
Improved Patient Access and Adherence
Beyond direct financial savings, the increased affordability and access facilitated by biosimilars translate into improved health equity and better clinical outcomes. Lower costs reduce medication abandonment and enable earlier initiation of highly effective therapies, preventing disease progression and reducing the overall disease burden, particularly for underserved communities.6
The lower costs associated with biosimilars directly increase the availability of treatment options and expand patient access to essential biologic therapies.2 Biosimilar competition has supported hundreds of millions of incremental days of therapy—344 million by 2022 and 495 million by 2023—meaning that patients received care that might otherwise have been inaccessible due to cost.27
Studies have shown a direct correlation between lower out-of-pocket costs and improved patient adherence to medications. Patients utilizing biosimilars, who generally faced lower out-of-pocket expenses, exhibited higher adherence rates compared to those on reference products.59 For instance, high adherence to infliximab biosimilars was observed in both treatment-naïve patients and those who switched from the originator product.64 This indicates that when the financial barrier is reduced, patients are more likely to consistently take their prescribed medications, leading to better disease management and improved health outcomes.
The increasing use of real-time prescription benefit tools further exemplifies this trend. The selection of biosimilars as alternative treatments through these tools jumped by 166% from January-September 2022 to the same period in 2023, indicating that patients are gaining access to treatment faster, easier, and more affordably.52 This widespread adoption and the resulting increased adherence underscore that the financial benefit of biosimilars is not just about money saved; it initiates a cascading positive effect on public health. When drugs are affordable, patients are more likely to take them as prescribed, leading to better disease management, fewer complications, and a more equitable distribution of life-changing therapies, ultimately reducing the broader societal cost of illness.
Table 1: Real-World Cost Savings from Biosimilar Adoption (Selected Examples)
| Therapeutic Area | Reference Product | Biosimilar(s) Example | Observed Price Reduction/Savings (%) | Source |
| Immunology | Remicade (Infliximab) | Inflectra/Renflexis | ~50% savings in Canada | 22 |
| Oncology | Stelara (Ustekinumab) | Ustekinumab biosimilars | 80-90% less than brand | 50 |
| Oncology | Herceptin (Trastuzumab) | Herzuma/Kanjinti | Up to 82% within 3 years | 26 |
| Immunology | Humira (Adalimumab) | Amjevita/Hyrimoz | 14% discount from 2020 net price | 34 |
| Diabetes | Lantus (Insulin Glargine) | Semglee | 65% discount at launch | 31 |
| Supportive Care | Neupogen (Filgrastim) | Zarxio | 55% WAC reduction | 38 |
| Supportive Care | Epogen (Epoetin Alfa) | Epoetin Alfa biosimilars | 51% WAC reduction | 61 |
| Supportive Care | Neulasta (Pegfilgrastim) | Pegfilgrastim biosimilars | 48% WAC reduction | 61 |
5. Barriers to Maximizing Patient Savings
Despite the clear benefits and potential of biosimilars, several significant barriers impede their widespread adoption and, consequently, limit the full realization of out-of-pocket cost reductions for patients. These challenges span physician and patient perceptions, misaligned financial incentives, and regulatory complexities.
Physician and Patient Hesitancy
A primary obstacle to biosimilar adoption stems from a pervasive lack of education and familiarity among both healthcare professionals (HCPs) and patients. This knowledge gap often leads to concerns regarding the safety, efficacy, and interchangeability of biosimilars.2 Many patients, for example, are concerned that biosimilars may not treat their disease as effectively as the reference product or could cause more adverse effects.33
A significant manifestation of this hesitancy is the reluctance to switch from a stable originator biologic to a biosimilar. Patients often express a strong desire to avoid such switches, particularly if their current biologic is working well, fearing a disruption in their continuity of care or potential negative outcomes.33 Physicians, too, may resist non-medical switching for patients already stabilized on a biologic therapy.47 This resistance is not always rooted in clinical evidence but can be influenced by the “nocebo effect,” where negative expectations about a treatment can lead to perceived negative outcomes.2
The “nocebo effect” and general human aversion to change, combined with a lack of clear, consistent education, create a significant psychological barrier to biosimilar adoption, even when robust clinical evidence supports their equivalence.33 This means that simply making biosimilars available and cheaper is often insufficient; addressing deeply ingrained perceptions and building trust through targeted, evidence-based communication is paramount for realizing patient savings. If patients perceive little or no difference in their out-of-pocket costs between the reference product and the biosimilar, their incentive to switch further diminishes, reinforcing the status quo.68
Misaligned Financial Incentives
The current financial architecture of the U.S. healthcare system presents a significant impediment to biosimilar adoption, as it often creates misaligned incentives that inadvertently favor more expensive originator biologics.
- Provider Reimbursement Models: Existing reimbursement models, such as the Average Sales Price (ASP) plus 6% model in Medicare Part B, can create a “perverse incentive” for providers.26 Under this model, the absolute dollar amount of the 6% add-on payment is higher for a more expensive drug. Consequently, a provider’s profit margin might shrink when prescribing a cheaper biosimilar, even if the percentage add-on is the same, incentivizing them to stick with the pricier originator biologic.26 This structure means that providers may not see direct financial benefits from prescribing biosimilars, leading to delayed adoption.66
- PBM Rebates: As previously discussed, Pharmacy Benefit Managers (PBMs) often negotiate substantial rebates with manufacturers of originator biologics in exchange for preferred formulary placement.5 These rebates can make a higher-list-price brand drug more financially attractive to the PBM, even if a biosimilar has a lower upfront cost but offers no comparable rebate.26 This practice limits biosimilar formulary access and can increase patient costs, as the “savings” from rebates are often retained by the PBM or payer rather than being passed directly to the patient in the form of lower out-of-pocket expenses.5
The current financial architecture of the U.S. healthcare system, particularly the interplay of provider reimbursement and PBM rebate practices, creates a fundamental misalignment of incentives that actively hinders the adoption of lower-cost biosimilars.5 This systemic flaw means that the theoretical savings from biosimilars are often not fully translated into lower out-of-pocket costs for patients, as financial benefits are captured elsewhere in the supply chain. This is not an accidental outcome; it is a direct consequence of how the financial system is structured, preventing the market from naturally driving down patient costs.
Regulatory Complexities and Market Uncertainties
Several regulatory and market-related factors also contribute to the slow adoption of biosimilars and limit their potential to reduce patient costs.
- High Development Costs: Bringing a biosimilar to market is a substantial financial undertaking, typically costing between $100 million and $300 million.1 This high investment makes market entry risky, particularly for biologics with lower sales volumes or smaller patient populations, as the projected return on investment may not justify the development expense.45
- Patent Thickets and Litigation: The complex patent landscape, characterized by numerous secondary patents, and the intricate litigation framework under the BPCIA, can significantly delay biosimilar market entry.23 These legal hurdles prolong the monopoly of originator biologics, thereby delaying competition and the associated price reductions that would benefit patients.
- Impact of Price Negotiation Policies: Well-intentioned government price negotiation policies, such as those introduced under the Inflation Reduction Act, can have unintended consequences. The threat of price negotiations may deter manufacturers from investing in and launching biosimilars, especially for high-sales biologics.32 This can lead to a “biosimilar void,” where many biologics scheduled to lose exclusivity in the coming years may not have biosimilar competition in development.32 This unpredictability directly undermines long-term patient affordability by stifling the very competition needed to drive down prices.
- Varying State Laws on Interchangeability: While the FDA grants a federal interchangeability designation, the actual dispensing and substitution of drugs at the pharmacy level are governed by varying state pharmacy laws.18 This patchwork of regulations adds complexity and inconsistency, hindering seamless substitution and limiting the immediate patient benefits that could arise from pharmacist-led transitions to lower-cost interchangeable biosimilars.
Table 2: Key Barriers to Biosimilar Adoption and Their Impact on Patient Costs
| Barrier Category | Specific Barrier | Impact on Patient Costs/Access | Relevant Stakeholders Affected | Source |
| Education & Perception | Lack of HCP/Patient Education | Delays adoption, reduces confidence in biosimilars, limits informed choices, perpetuates higher costs. | Patients, Providers, Payers | 2 |
| Patient Reluctance to Switch | Leads to non-medical switching avoidance, maintaining use of higher-cost reference products. | Patients, Providers | 33 | |
| Perceived Lack of Financial Benefit to Patient | Diminishes patient incentive to switch, even if system-level savings exist. | Patients | 68 | |
| Financial Incentives | Misaligned Provider Reimbursement | Incentivizes use of higher-cost originators, reducing provider motivation to prescribe biosimilars. | Providers, Patients | 26 |
| PBM Rebate Practices | Favors higher-list-price drugs with larger rebates, limiting biosimilar formulary access and potentially increasing patient out-of-pocket costs. | Payers, Patients | 5 | |
| Copay Accumulator Programs | Prevents manufacturer copay assistance from counting towards deductibles, increasing patient out-of-pocket burden. | Patients, Payers | 60 | |
| Regulatory & Market | High Development Costs | Creates high market entry barriers, especially for low-sales biologics, limiting competition. | Biosimilar Manufacturers, Patients | 1 |
| Patent Thickets & Litigation | Delays biosimilar market entry, prolonging originator monopolies and delaying price reductions. | Biosimilar Manufacturers, Originator Manufacturers, Patients | 23 | |
| Price Negotiation Policies (IRA) | Increases market uncertainty for biosimilar developers, potentially leading to a “biosimilar void” and reduced future competition. | Biosimilar Manufacturers, Policymakers, Patients | 32 | |
| Lack of Interchangeability (U.S.) | Requires prescriber intervention for substitution, adding administrative burden and delaying patient access to cheaper options. | Patients, Providers, Pharmacists, Policymakers | 18 |
6. Strategies for Enhanced Patient Affordability and Access
To fully unlock the potential of biosimilars in reducing patient out-of-pocket costs and improving access to essential therapies, a multi-faceted approach involving policy reforms, robust education, and realignment of financial incentives is imperative.
Policy Reforms
Strategic policy interventions can significantly accelerate biosimilar adoption and ensure direct patient cost savings. This indicates that legislative and regulatory bodies hold substantial power to unlock the full patient benefit of biosimilars.
- Streamlining Approval and Addressing Patent Thickets: Expediting prior authorizations for biosimilars can simplify administrative processes and enable immediate patient access.66 Furthermore, streamlining the regulatory approval process itself can accelerate biosimilar entry into the market.34 Addressing the issue of “patent thickets” and promoting patent litigation settlements are crucial steps, as settlements have been shown to accelerate generic and biosimilar market entry by over five years before patent expiration.32
- Incentivizing Biosimilar Use: Policymakers can implement measures that directly incentivize the use of biosimilars. For instance, increasing Medicare reimbursement for biosimilars, as proposed by the BIOSIM Act, which suggests an 8% add-on payment for biosimilars compared to 6% for reference products, can encourage practitioners to prescribe these more affordable options.70
- Harmonizing Interchangeability Standards: Unifying the standard so that all FDA-approved biosimilars are considered interchangeable with their reference products, similar to the approach taken in the EU, would significantly boost adoption and simplify pharmacy-level substitution.16 This would remove a key administrative barrier and allow patients to more readily access lower-cost alternatives.
- Addressing Copay Accumulators: Legislative action requiring copay assistance to count towards patients’ deductibles and out-of-pocket maximums is crucial.60 Such policies ensure that the financial assistance provided by manufacturers directly benefits patients in meeting their cost-sharing obligations, rather than being absorbed by insurers.
Education and Awareness Initiatives
Educational initiatives are not merely about disseminating information; they are crucial for bridging the knowledge-action gap that exists among both providers and patients.2 By building confidence and trust through evidence-based communication, these programs empower individuals to make informed decisions that align with cost-effective care, directly translating to greater patient savings and adherence.
- Targeted Education for Healthcare Professionals (HCPs): Programs specifically designed for prescribers that focus on biosimilar safety, efficacy, real-world evidence, and interchangeability data are critical to increasing prescriber confidence.2 This includes providing clear information on the scientific basis for biosimilarity and addressing concerns about extrapolation of indications and switching patients.
- Comprehensive Patient Education: Providing easy-to-understand materials about biosimilar safety, efficacy, and cost benefits can effectively overcome patient hesitancy and build trust.24 Healthcare providers, particularly infusion nurses, are well-positioned to inform patients about the potential benefits of biosimilars, address any concerns, and facilitate treatment switches.2
- Addressing Misconceptions: Actively countering misinformation and clarifying the fundamental differences between biosimilars and generic drugs is essential to prevent confusion and foster acceptance.24
Realigning Financial Incentives for Payers and Providers
Realigning financial incentives across the healthcare ecosystem—from PBMs to providers—is not merely about shifting costs but about optimizing the system to reward value and efficiency.25 By ensuring that all stakeholders benefit from biosimilar adoption, rather than being disincentivized, the system can naturally steer towards more affordable options, directly benefiting patients through reduced out-of-pocket expenses and improved access.
- Reduce Patient Cost-Sharing: Actively decreasing out-of-pocket costs for patients who use biosimilars, through lower copays or coinsurance, provides a direct and tangible incentive for patients to choose these more affordable options.29
- Adjust Provider Reimbursement: Implement changes to provider reimbursement models that increase the financial incentive for prescribing biosimilars. This could involve fee schedule adjustments or other benefits that make biosimilar use more financially attractive for healthcare practices.66 Additionally, shifting towards value-based payments that tie reimbursement to patient outcomes rather than just drug choice can encourage the use of cost-effective therapies.26
- PBM Transparency and Accountability: Encourage greater transparency in PBM practices and hold them accountable for ensuring that negotiated rebates translate into lower costs for patients.26 This could involve regulatory oversight to prevent practices that favor higher-cost drugs due to larger rebate opportunities.
- Value-Based Care Models: Promote the widespread adoption of value-based care models that incentivize the use of high-value, lower-cost therapies like biosimilars across the healthcare system.25
Fostering a More Competitive and Transparent Market
A robust biosimilar market requires continuous efforts to enhance competition and transparency.
- Promote Multiple Biosimilar Entrants: Encouraging several biosimilar competitors for each reference biologic is vital, as increased competition consistently drives greater price reductions.1
- Leverage Data Tools and Insights: Utilizing advanced analytics and data tools is essential for tracking market movements, identifying cost-saving opportunities, and supporting informed decision-making by businesses and healthcare systems.25
- Cross-Stakeholder Collaboration: Fostering collaboration and open dialogue among policymakers, pharmaceutical companies (both originator and biosimilar), payers, healthcare providers, and patient advocacy groups is crucial to collectively address existing barriers and accelerate biosimilar adoption.29
7. Conclusion: Unlocking the Full Potential for Health Equity
Biosimilars represent a critical innovation in modern healthcare, offering a powerful mechanism to manage the escalating costs of biologic therapies, ensure the sustainability of healthcare systems, and expand access to life-changing treatments.2 Their proven ability to introduce competition and drive down drug prices has already generated billions in savings for the healthcare system and, in many cases, directly reduced patient out-of-pocket costs.
The increased affordability and access facilitated by biosimilars extend beyond mere financial relief; they directly contribute to improved health equity and better clinical outcomes. By reducing financial toxicity—the economic burden and psychological distress associated with high healthcare costs—and improving medication adherence, biosimilars enable more patients to receive and continue necessary treatments.9 This is particularly impactful for vulnerable populations, including women, seniors, and low-income individuals, who are disproportionately affected by the high costs of biologics.35 Lower costs reduce medication abandonment and enable earlier initiation of highly effective therapies, which can prevent disease progression and reduce the overall disease burden, ultimately leading to a more equitable distribution of life-changing treatments.
However, the full potential of biosimilars remains largely unrealized due to a complex interplay of market dynamics, regulatory hurdles, and behavioral factors. Overcoming physician and patient hesitancy, rectifying misaligned financial incentives, and navigating regulatory complexities are essential steps. Realizing the maximum benefits of biosimilars for patients requires a concerted, multi-stakeholder effort. This collaborative approach will pave the way for a healthcare landscape where cost is less of a barrier to essential, high-quality care, fostering improved patient outcomes and a more sustainable system for the future.
8. Recommendations
To maximize the role of biosimilars in reducing out-of-pocket costs for patients and enhancing access to critical therapies, a coordinated effort across all healthcare stakeholders is imperative. The following actionable recommendations are proposed:
Table 3: Actionable Recommendations for Stakeholders to Improve Biosimilar Access and Affordability
| Stakeholder | Recommendation | Rationale/Expected Impact on Patient Out-of-Pocket Costs & Access | Source |
| Policymakers | Streamline Regulatory Process & Address Patent Thickets: Expedite biosimilar approval pathways and implement policies to mitigate patent thickets and litigation delays. | Accelerates market entry of lower-cost biosimilars, increasing competition and driving down prices faster. | 32 |
| Harmonize Interchangeability Standards: Unify federal and state regulations to consider all FDA-approved biosimilars as interchangeable. | Simplifies pharmacy-level substitution, reducing administrative burdens and allowing patients immediate access to cheaper options. | 16 | |
| Ban Copay Accumulator Programs: Enact and enforce legislation requiring copay assistance to count towards patient deductibles and out-of-pocket maximums. | Ensures manufacturer assistance directly benefits patients in meeting cost-sharing, preventing unexpected financial burdens. | 60 | |
| Incentivize Biosimilar Use in Reimbursement: Adjust Medicare and other payer reimbursement models to provide stronger financial incentives for providers to prescribe biosimilars. | Encourages provider adoption by aligning financial benefits with lower-cost options, potentially leading to lower patient costs. | 26 | |
| Pharmaceutical Companies (Originator) | Engage in Responsible Patent Practices: Avoid excessive secondary patenting that unduly delays biosimilar entry. | Fosters earlier competition, leading to faster price reductions and increased patient access. | 42 |
| Participate in Patent Settlements: Pursue timely and fair patent settlements with biosimilar manufacturers. | Accelerates market entry of biosimilars, bringing competition and affordability to patients sooner. | 49 | |
| Pharmaceutical Companies (Biosimilar) | Invest in Interchangeability Studies: Prioritize seeking interchangeability designation where feasible and impactful for patient access. | Enables broader pharmacy-level substitution, making it easier for patients to access lower-cost alternatives. | 18 |
| Offer Competitive Pricing Strategies: Continue to launch biosimilars with significant discounts and explore innovative pricing models. | Drives down overall drug costs and directly reduces patient out-of-pocket expenses. | 31 | |
| Payers (Insurance Plans/PBMs) | Prioritize Biosimilars on Formularies: Design formularies that favor biosimilars and ensure their competitive pricing translates into lower patient cost-sharing. | Directs patients to more affordable options, reducing their out-of-pocket expenses and improving adherence. | 29 |
| Increase Transparency of Rebates: Ensure that rebates negotiated with manufacturers translate into direct savings for patients through lower premiums or out-of-pocket costs. | Aligns financial incentives with patient benefit, preventing “perverse incentives” that favor higher-cost drugs. | 26 | |
| Implement Value-Based Care Models: Develop and adopt payment models that reward the use of high-value, cost-effective therapies like biosimilars. | Incentivizes efficient resource allocation, leading to overall system savings that can be passed to patients. | 25 | |
| Healthcare Providers (Physicians, Pharmacists, Nurses) | Enhance Biosimilar Education: Actively seek and participate in educational programs on biosimilar safety, efficacy, and interchangeability. | Increases prescriber confidence, leading to greater willingness to prescribe and recommend biosimilars. | 2 |
| Engage in Patient Counseling: Proactively discuss biosimilar options with patients, addressing concerns about switching and highlighting financial benefits. | Builds patient trust, reduces hesitancy, and empowers informed decisions that lead to lower out-of-pocket costs. | 2 | |
| Streamline Internal Processes: Optimize prior authorization processes and pharmacy inventory management for biosimilars. | Reduces administrative barriers, ensuring smoother transitions and timely access to treatment. | 66 | |
| Patient Advocacy Groups | Advocate for Policy Reforms: Support legislation that addresses patent thickets, harmonizes interchangeability, and bans copay accumulators. | Drives systemic changes that directly reduce patient out-of-pocket costs and improve access. | 60 |
| Develop Accessible Educational Materials: Create and disseminate clear, evidence-based information about biosimilars for patients and the public. | Empowers patients to understand and accept biosimilars, overcoming hesitancy and promoting informed choices. | 24 | |
| Amplify Patient Voices: Share real-world patient experiences of financial toxicity and the benefits of biosimilars to inform policymakers and industry. | Highlights the direct human impact of drug costs and the potential for biosimilars to alleviate financial burden. | 9 |
Works cited
- Federal Barriers Make Biologic Drugs Unaffordable | Issue Brief | Healthcare, accessed July 26, 2025, https://americafirstpolicy.com/issues/federal-barriers-make-biologic-drugs-unaffordable
- Biosimilars: From Production to Patient – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10786443/
- Biosimilars Market Size to Hit $76.2 Billion by 2030 – Driving Value-Based Care for Drugmakers, Regulators & Emerging Markets | The Research Insights – PR Newswire, accessed July 26, 2025, https://www.prnewswire.com/news-releases/biosimilars-market-size-to-hit-76-2-billion-by-2030—driving-value-based-care-for-drugmakers-regulators–emerging-markets–the-research-insights-302495541.html
- The Real Cost of Biologic Drugs, accessed July 26, 2025, https://biologicmeds.org/biologic-basics/the-real-cost-of-biologic-drugs/
- The Cost Savings of Biosimilars Can Help Increase Patient Access and Lift the Financial Burden of Health Care Systems | Request PDF – ResearchGate, accessed July 26, 2025, https://www.researchgate.net/publication/357429703_The_Cost_Savings_of_Biosimilars_Can_Help_Increase_Patient_Access_and_Lift_the_Financial_Burden_of_Health_Care_Systems
- Beyond Cost: Observations on Clinical and Patient Benefits of Biosimilars in Real-World Settings – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12185555/
- 5 Reasons Biologics Remain Expensive, accessed July 26, 2025, https://medicalaffairsspecialist.org/blog/5-reasons-biologics-remain-expensive
- Why Are Biosimilars Not Living up to Their Promise in the US? – AMA Journal of Ethics, accessed July 26, 2025, https://journalofethics.ama-assn.org/article/why-are-biosimilars-not-living-their-promise-us/2019-08
- An Arm and a Leg: The Rising Cost of Cancer Drugs and Impact on Access, accessed July 26, 2025, https://ascopubs.org/doi/10.1200/EDBK_100028
- Same Treatment, Lower Price: How Biosimilar Medications Are Making Healthcare More Affordable, accessed July 26, 2025, https://www.bcbsks.com/employers/resources/same-treatment-lower-price-how-biosimilar-medications-are-making-healthcare-more-affordable
- Financial toxicity related to biological medications – a scoping review of evidence – Helda, accessed July 26, 2025, https://helda.helsinki.fi/items/0d48f6b3-a057-4e91-9dc1-73231b26ea87
- The effect of cost on adherence to prescription medications in Canada – CMAJ, accessed July 26, 2025, https://www.cmaj.ca/content/184/3/297
- Following the Money: Untangling U.S. Prescription Drug Financing, accessed July 26, 2025, https://www.americanprogress.org/article/following-the-money-untangling-u-s-prescription-drug-financing/
- Definition of biosimilar drug – NCI Dictionary of Cancer Terms, accessed July 26, 2025, https://www.cancer.gov/publications/dictionaries/cancer-terms/def/biosimilar-drug
- Biosimilar Product Regulatory Review and Approval | FDA, accessed July 26, 2025, https://www.fda.gov/files/drugs/published/Biosimilar-Product-Regulatory-Review-and-Approval.pdf
- Biosimilar medicines: Overview – EMA – European Union, accessed July 26, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/biosimilar-medicines-overview
- Q&A Biosimilars – Health Professionals 1. What are biologic drugs? Biologic drugs, commonly referred to as “Biologics”, accessed July 26, 2025, https://www.gov.nl.ca/hcs/files/Frequently-Asked-Questions-Health-Professionals.pdf
- 9 Things to Know About Biosimilars and Interchangeable Biosimilars – FDA, accessed July 26, 2025, https://www.fda.gov/drugs/things-know-about/9-things-know-about-biosimilars-and-interchangeable-biosimilars
- Biosimilar Regulatory Review and Approval – FDA, accessed July 26, 2025, https://www.fda.gov/media/151061/download
- www.goodrx.com, accessed July 26, 2025, https://www.goodrx.com/drugs/biologics/biosimilar-vs-generic#:~:text=Generics%20are%20small%20molecule%20drugs,be%20substituted%20in%20this%20way.
- Difference between generic drugs and biosimilar drugs | Gouvernement du Québec, accessed July 26, 2025, https://www.quebec.ca/en/health/medications/biosimilar-drugs/difference-between-generic-drugs-and-biosimilar-drugs
- Biosimilars or Biologics: What’s the difference? – Therapeutics Letter – NCBI Bookshelf, accessed July 26, 2025, https://www.ncbi.nlm.nih.gov/books/NBK598450/
- The Economics of Biosimilars – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4031732/
- Biosimilars Education and Advocacy AiArthritis, accessed July 26, 2025, https://www.aiarthritis.org/biosimilars
- Transforming healthcare with biosimilars: lower costs, greater access, smarter solutions, accessed July 26, 2025, https://www.wolterskluwer.com/en/expert-insights/transforming-healthcare-biosimilars-lower-costs-smarter-solutions
- The impact of biosimilars on biologic drug reimbursement models – DrugPatentWatch, accessed July 26, 2025, https://www.drugpatentwatch.com/blog/the-impact-of-biosimilars-on-biologic-drug-reimbursement-models/
- The U.S. Generic & Biosimilar Medicines Savings Report, accessed July 26, 2025, https://accessiblemeds.org/wp-content/uploads/2025/01/AAM-2024-Generic-Biosimilar-Medicines-Savings-Report.pdf
- Data Snapshot: Biosimilar Cost and Use Trends in Medicare Part B, accessed July 26, 2025, https://oig.hhs.gov/reports/all/2024/data-snapshot-biosimilar-cost-and-use-trends-in-medicare-part-b/
- Decoding the biosimilar paradox: Policy reforms, increased transparency and patient education – Medical Economics, accessed July 26, 2025, https://www.medicaleconomics.com/view/decoding-the-biosimilar-paradox-policy-reforms-increased-transparency-and-patient-education
- Biosimilars Through the Years: Transforming Access and Cost in Biologics, accessed July 26, 2025, https://www.pharmasalmanac.com/articles/biosimilars-through-the-years-transforming-access-and-cost-in-biologics
- Insulin Prices are Rising Unchecked. New Biosimilar Insulins May Cost You Less., accessed July 26, 2025, https://beyondtype1.org/biosimilar-insulin-cost-savings/
- Medicare Price Negotiations Will Slow Biosimilar Momentum, Widening Market Gap, accessed July 26, 2025, https://www.centerforbiosimilars.com/view/medicare-price-negotiations-will-slow-biosimilar-momentum-widening-market-gap
- Analyzing biosimilar market dynamics in different patient populations – DrugPatentWatch, accessed July 26, 2025, https://www.drugpatentwatch.com/blog/analyzing-biosimilar-market-dynamics-in-different-patient-populations/
- Biosimilars in Focus: Advancing Implementation in Health Care Systems, accessed July 26, 2025, https://www.ajmc.com/view/biosimilars-in-focus-advancing-implementation-in-health-care-systems
- Understanding Biosimilars – Achieving a sustainable health equity – Biocon, accessed July 26, 2025, https://www.biocon.com/businesses/biosimilars/understanding-biosimilars/
- Part 1: Unlocking the Potential of Biosimilars to Improve Health Equity, accessed July 26, 2025, https://www.centerforbiosimilars.com/view/part-1-unlocking-the-potential-of-biosimilars-to-improve-health-equity
- The Case for Biosimilars – Biospecialized, accessed July 26, 2025, https://www.biospecialized.com/case-for-biosimilars/
- Case Studies on Successful Biosimilar Launches: Transforming Healthcare – Genefic, accessed July 26, 2025, https://genefic.com/case-studies-on-successful-biosimilar-launches-transforming-healthcare/
- Report: 2023 U.S. Generic and Biosimilar Medicines Savings Report, accessed July 26, 2025, https://accessiblemeds.org/resources/reports/2023-savings-report-2/
- Biosimilar and interchangeable: Inseparable scientific concepts? – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6848899/
- Biosimilar medicines can be interchanged – EMA – European Union, accessed July 26, 2025, https://www.ema.europa.eu/en/news/biosimilar-medicines-can-be-interchanged
- REALIZING THE BENEFITS OF BIOSIMILARS: – Duke-Margolis Institute for Health Policy, accessed July 26, 2025, https://healthpolicy.duke.edu/sites/default/files/2021-04/Realizing%20the%20Benefits%20of%20Biosimilars.pdf
- What role for real-world evidence in market access of biosimilars? – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11891046/
- Biosimilar medicines: marketing authorisation – EMA – European Union, accessed July 26, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/biosimilar-medicines-marketing-authorisation
- The Biosimilar Void: 90% of Biologics Coming Off Patent Will Lack Biosimilars, accessed July 26, 2025, https://www.centerforbiosimilars.com/view/the-biosimilar-void-90-of-biologics-coming-off-patent-will-lack-biosimilars
- 5 Things Worth Knowing About Biosimilars and Interchangeability – Pfizer, accessed July 26, 2025, https://www.pfizer.com/news/articles/5_things_worth_knowing_about_biosimilars_and_interchangeability
- Provider and Patient Knowledge Gaps on Biosimilars: Insights From Surveys, accessed July 26, 2025, https://www.ajmc.com/view/biosimilarssuppl-insightssurveys
- Accelerating biosimilar market access: the case for allowing earlier standing | Journal of Law and the Biosciences | Oxford Academic, accessed July 26, 2025, https://academic.oup.com/jlb/article/12/1/lsae030/7942247
- New Report on Patent Litigation Settlements Says that they are Critically Necessary to Ensure Prompt Generic and Biosimilar Market Entry – FDA Law Blog, accessed July 26, 2025, https://www.thefdalawblog.com/2025/06/new-report-on-patent-litigation-settlements-says-that-they-are-critically-necessary-to-ensure-prompt-generic-and-biosimilar-market-entry/
- Competition Beats Price Controls — and Patients Pay the Price When We Forget It, accessed July 26, 2025, https://biosimilarscouncil.org/resource/competition-beats-price-controls-and-patients-pay-the-price-when-we-forget-it/
- New IQVIA Report: Biosimilars Driving Lower Prices and Greater Savings, accessed July 26, 2025, https://biosimilarscouncil.org/news/new-iqvia-report-biosimilars-driving-lower-prices-and-greater-savings/
- Biosimilars Are Changing the Game – Surescripts, accessed July 26, 2025, https://surescripts.com/insights/prescription-data-biosimilar-medications
- Savings Report Shows the Value of Biosimilars for Patients with Cancer, accessed July 26, 2025, https://biosimilarscouncil.org/resource/savings-report-shows-the-value-of-biosimilars-for-patients-with-cancer/
- Oncology Biosimilars Offer Potential Relief From Financial Burden of Cancer Care, accessed July 26, 2025, https://www.ajmc.com/view/oncology-biosimilars-offer-potential-relief-from-financial-burden-of-cancer-care
- The Biosimilar Shift: How PBMs Are Reshaping Formularies, accessed July 26, 2025, https://www.ajmc.com/view/the-biosimilar-shift-how-pbms-are-reshaping-formularies
- The Big Three PBMs’ 2025 Formulary Exclusions: Humira, Stelara, Private Labels, and the Shaky Future for Pharmacy Biosimilars – Drug Channels, accessed July 26, 2025, https://www.drugchannels.net/2025/01/the-big-three-pbms-2025-formulary.html
- Expert Insights on Overcoming Patient Education Gaps, Biosimilar Financial Hurdles, accessed July 26, 2025, https://www.centerforbiosimilars.com/view/overcoming-patient-education-gaps-biosimilar-financial-hurdles-in-focus-with-canavan-o-dell
- How do drug plans work? | Medicare, accessed July 26, 2025, https://www.medicare.gov/health-drug-plans/part-d/what-plans-cover/how-drug-plans-work
- Real-World Evidence on Biosimilar Adherence and Adoption, accessed July 26, 2025, https://www.ajmc.com/view/real-world-evidence-on-biosimilar-adherence-and-adoption
- Copay accumulators and programs that harm access to healthcare – PAN Foundation, accessed July 26, 2025, https://www.panfoundation.org/protecting-your-access-to-medications/
- Inpatient Biosimilar Use Grows, Offering Cost-Saving Opportunities for Health Systems, accessed July 26, 2025, https://www.pharmacytimes.com/view/inpatient-biosimilar-use-grows-offering-cost-saving-opportunities-for-health-systems
- Cost Savings Potential Associated With the Use of Biosimilars, accessed July 26, 2025, https://www.ajmc.com/view/cost-savings-potential-associated-with-the-use-of-biosimilars
- Production costs and potential prices for biosimilars of human insulin and insulin analogues, accessed July 26, 2025, https://gh.bmj.com/content/3/5/e000850
- Utilization and Adherence Among Infliximab Biosimilar Initiators in a US National Commercial Insurance Database – The Oncology Pharmacist, accessed July 26, 2025, https://theoncologypharmacist.com/special-issues/2020-year-in-review-biosimilars/utilization-and-adherence-among-infliximab-biosimilar-initiators-in-a-us-national-commercial-insurance-database
- (PDF) Understanding the factors influencing the adoption of biosimilars; an innovation theory perspective – ResearchGate, accessed July 26, 2025, https://www.researchgate.net/publication/393001211_Understanding_the_factors_influencing_the_adoption_of_biosimilars_an_innovation_theory_perspective
- Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10391006/
- Identification of Barriers Preventing Biosimiliar Oncology Medication Adoption – PMC, accessed July 26, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9696566/
- Biosimilar Adoption & Barriers to Success: Current and Future Considerations – FDA, accessed July 26, 2025, https://www.fda.gov/media/143990/download
- Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative | Journal of Managed Care & Specialty Pharmacy – JMCP.org, accessed July 26, 2025, https://www.jmcp.org/doi/10.18553/jmcp.2021.27.8.1129
- Patient Advocacy Groups Offer Support for BIOSIM Act – Center for Biosimilars, accessed July 26, 2025, https://www.centerforbiosimilars.com/view/patient-advocacy-groups-offer-support-for-biosim-act
- Championing biosimiars – Boehringer Ingelheim, accessed July 26, 2025, https://pro.boehringer-ingelheim.com/us/payor/strategiesforqualitycare/bipdf/championing-biosimiars
- Biosimilars USA : Pharmaceuticals : North America – SAE Media Group, accessed July 26, 2025, https://www.smgconferences.com/pharmaceuticals/northamerica/conference/biosimilars-north-america