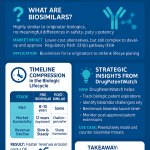
Executive Summary & The New Biologic Battleground
The global pharmaceutical landscape is undergoing a seismic shift, driven by the confluence of immense therapeutic innovation and unsustainable healthcare costs. At the epicenter of this transformation are biologic medicines—large, complex molecules derived from living organisms that have revolutionized the treatment of cancer, autoimmune diseases, and other chronic conditions.1 While their clinical impact is undeniable, their economic footprint is staggering. In the United States, biologics accounted for a mere 2% of prescriptions in 2023 yet constituted 46% of total pharmaceutical spending, a testament to their high price tags.2 This economic pressure has created an urgent and compelling market for biosimilars: highly similar, lower-cost versions of originator biologics that enter the market upon patent expiry.
This report frames the biosimilar market not merely as a source of cost savings but as a complex strategic battleground where scientific innovation, regulatory navigation, and intellectual property (IP) warfare converge. While the foundational premise—that approved biosimilars are clinically “just as good” as their reference products—is now firmly established by a mountain of regulatory and real-world evidence, commercial success is far from guaranteed. The path to market is fraught with challenges, from labyrinthine regulatory requirements and entrenched commercial interests to, most critically, the formidable legal fortresses erected by originator companies.
The central thesis of this analysis is that in the high-stakes biosimilar gambit, market success is ultimately determined by strategic acumen, with sophisticated patent intelligence serving as the primary weapon. Companies that master the art of deconstructing an originator’s IP portfolio, anticipating legal maneuvers, and leveraging this intelligence to inform their development and launch strategies will be the ones to capture market share and achieve commercial viability. Those that treat patent analysis as a mere checkbox exercise risk years of delays and hundreds of millions of dollars in squandered investment.
This document serves as a definitive strategic guide for decision-makers in the pharmaceutical, biotechnology, and life sciences investment sectors. It moves beyond a simple scientific comparison to deliver a nuanced analysis of the strategic, regulatory, and commercial landscape, with IP as the central pivot point. The report will deconstruct the science that differentiates biosimilars from generics, navigate the regulatory gauntlets of the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), quantify the economic impact of competition, and provide a deep dive into the patent warfare that defines this space. Ultimately, it provides a strategic framework for converting patent data into a tangible, sustainable competitive advantage.
Deconstructing the Molecules: Why Biosimilars Are Not Generics
To grasp the strategic complexities of the biosimilar market, one must first understand the fundamental scientific realities that distinguish them from traditional small-molecule generic drugs. This distinction is not merely academic; it is the central pivot upon which the entire regulatory, economic, and commercial framework for biosimilars is built. It dictates everything from development costs and timelines to the very nature of market competition.
The Science of Biologics: A World of Complexity
Biologic medicines are a class of drugs produced from or containing components of living organisms, such as animal cells, yeast, or bacteria.1 Unlike conventional drugs, which are chemically synthesized, biologics are grown through complex, proprietary manufacturing processes.5 This biological origin is the source of their immense therapeutic power and their inherent complexity.
The defining characteristic of a biologic is its size and structural intricacy. A small-molecule drug like aspirin consists of just 21 atoms, creating a simple, well-defined, and easily replicable chemical structure.5 In stark contrast, a biologic therapeutic protein can be composed of over 25,000 atoms, folded into a precise three-dimensional configuration that is essential for its function.5 Think of a small-molecule drug as a simple brick, easy to replicate with identical results every time. A biologic, however, is more akin to an intricately designed house, built with living materials and processes.8
Because biologics are produced in living systems, they are subject to natural variability. The process of growing cells and then extracting and purifying the desired protein is a multi-step, highly sensitive operation.5 Minor fluctuations in the manufacturing environment can lead to slight differences between batches of the very same product. These variations, such as post-translational modifications like glycosylation, are normal and expected, but they mean that no two batches of a biologic are ever perfectly identical.1 This inherent micro-heterogeneity is a critical scientific concept: if the originator manufacturer cannot produce an exact copy of its own product from one batch to the next, it is biologically impossible for a different company, using its own proprietary cell line and manufacturing process, to create an exact replica.1 This impossibility of exact replication is the scientific bedrock that necessitates a unique regulatory and commercial pathway for biosimilars.
Defining the Spectrum: Biologics, Biosimilars, and Interchangeable Products
The unique nature of biologics has led regulatory agencies like the FDA and EMA to establish a specific lexicon to categorize these products, each with distinct requirements and market implications.1
- Biologic (Reference Product): This is the original, innovative product approved by a regulatory authority through a “standalone” application.13 The manufacturer must submit a complete dossier of data from preclinical and extensive clinical trials (Phase 1, 2, and 3) to independently establish the product’s safety and efficacy for each intended use.14 This originator product serves as the benchmark—the “reference”—against which all subsequent biosimilars are compared.
- Biosimilar: A biosimilar is a biological product that is approved based on a demonstration that it is “highly similar” to an already-approved reference product and has “no clinically meaningful differences” from the reference product in terms of safety, purity, and potency (effectiveness).1 The goal of a biosimilar development program is not to independently prove the drug works, but to prove it is highly similar to a drug that has already been proven to work.13 This allows the biosimilar manufacturer to leverage the originator’s clinical data, avoiding the need to repeat costly and lengthy clinical trials.1
- Interchangeable Biosimilar (A US-Specific Designation): In the United States, a biosimilar can seek an additional designation of “interchangeable”.11 An interchangeable product is a biosimilar that meets further statutory requirements. The manufacturer must provide additional data demonstrating that the product is expected to produce the same clinical result as the reference product in any given patient.12 Furthermore, for a product administered more than once, the manufacturer must show that the risk of alternating or switching between the interchangeable product and the reference product is no greater than the risk of using the reference product without switching.12 This higher regulatory bar allows an interchangeable product to be substituted for the reference product at the pharmacy level without the intervention of the prescribing physician, much like a generic drug, subject to state pharmacy laws.4
It is a common misconception that the “interchangeable” designation implies a higher level of safety or efficacy than a standard biosimilar. The FDA has been clear that both biosimilars and interchangeable biosimilars are equally safe and effective and can be prescribed with the same level of confidence in place of the reference product.11 The distinction is primarily a regulatory one that impacts the logistics of substitution at the pharmacy.
The Critical Distinction from Small-Molecule Generics
The differences between biosimilars and small-molecule generics are profound and extend across every facet of their development, regulation, and commercialization. Understanding these distinctions is paramount for any stakeholder formulating a strategy in the biologics space.
- Molecular Structure and Size: Generics are chemically synthesized small molecules with low molecular weight and simple, well-defined structures.6 Biosimilars are biologically produced large molecules with high molecular weight and complex, heterogeneous structures that are difficult to fully characterize.6
- Regulatory Standard: The approval standard for a generic drug is “bioequivalence,” meaning it must contain the identical active pharmaceutical ingredient as the brand-name drug and perform in the same manner.5 The standard for a biosimilar is “biosimilarity,” a more complex assessment based on the “totality of the evidence” to prove it is highly similar with no clinically meaningful differences.1
- Development Cost and Timeline: The straightforward nature of generics allows for a relatively swift and inexpensive development process. A generic drug can be developed in about two years for approximately $1-4 million, as extensive clinical trials are not required.6 In stark contrast, the complexity of reverse-engineering a biologic and conducting the necessary comparative studies means developing a biosimilar is a far more arduous and capital-intensive endeavor. A typical biosimilar takes six to nine years to develop and costs between $100 million and $300 million.2
- Market Price Discount: The low development cost and high level of competition in the generic market lead to steep price reductions. Generics are often available at discounts of 80-85% or more compared to their brand-name counterparts.6 Due to their much higher development costs and more complex market dynamics, biosimilars typically launch with more modest price discounts, generally in the range of 15% to 50% of the reference product’s price.16
The initial scientific reality—the impossibility of creating an identical copy of a complex biologic—directly dictates a different business model, risk profile, and market dynamic for biosimilars. This explains why the “patent cliff” for biologics is a gentler, more contested slope than the precipitous drop-off seen with small-molecule drugs. The higher bar of proof for biosimilarity requires extensive analytical and clinical data, which in turn drives up development costs and timelines. This financial reality shapes everything from pricing strategy and market penetration expectations to the nature of the inevitable patent litigation that precedes market entry.
The Regulatory Gauntlet: A Tale of Two Agencies (FDA vs. EMA)
The commercial viability of any biosimilar hinges on securing approval from key regulatory bodies, primarily the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). While both agencies are globally respected for their rigorous, science-based standards, they have distinct frameworks, histories, and nuances that create different strategic challenges and opportunities for manufacturers. A deep understanding of these regulatory pathways is not just a compliance requirement; it is a critical component of a successful global development and commercialization strategy.
The Foundation of Trust: The “Totality of the Evidence” Approach
Modern biosimilar regulation, as practiced by both the FDA and EMA, is built upon the foundational principle of the “totality of the evidence”.8 This approach moves away from the traditional model of requiring a full, standalone demonstration of a drug’s safety and efficacy. Instead, it relies on a comprehensive and cumulative evaluation of a wide range of comparative data, where each piece of evidence informs the next in a stepwise fashion, building a convincing case for biosimilarity.8
The process is often visualized as a pyramid. At the base, forming the widest and most critical foundation, are extensive analytical studies.13 These studies employ a battery of state-of-the-art techniques to conduct a deep physicochemical and biological characterization of both the proposed biosimilar and the reference product.8 Scientists meticulously compare attributes like primary amino acid sequence, higher-order protein structures, post-translational modifications (e.g., glycosylation), and biological activity (e.g., antigen binding).19 These analytical methods are incredibly sensitive and are often more capable of detecting minor structural differences than human clinical trials.20 A strong demonstration of analytical similarity at this foundational stage provides the greatest degree of confidence and can significantly reduce the amount of non-clinical and clinical data required by regulators.8
The subsequent steps in the pyramid—non-clinical animal studies and human clinical studies—are not designed to independently establish the safety and efficacy of the biosimilar. Rather, their purpose is to address any residual uncertainty that may remain after the exhaustive analytical comparison.8 Clinical data typically include:
- Pharmacokinetic (PK) and Pharmacodynamic (PD) Studies: These are human pharmacology studies, often conducted in healthy volunteers, to demonstrate that the biosimilar moves through the body (PK) and has the same effects on the body (PD) as the reference product.8
- Immunogenicity Assessment: Because all biologics have the potential to elicit an immune response, a comparative assessment of immunogenicity (the propensity to generate anti-drug antibodies) is a critical component of every biosimilar development program.8
- Comparative Clinical Efficacy and Safety Trial: In some cases, particularly for more complex biologics or where analytical or PK/PD data leave some uncertainty, regulators may require at least one comparative clinical trial in a sensitive patient population to confirm that there are no clinically meaningful differences in efficacy and safety.8
Navigating the Pathways: BPCIA in the U.S. vs. the Centralized Procedure in the EU
While sharing the same scientific philosophy, the FDA and EMA operate under distinct legal and procedural frameworks. The European Union has a significant head start, having established its biosimilar pathway in 2005 and approving the first biosimilar, Omnitrope, in 2006.1 This long history has resulted in a mature, well-trodden regulatory pathway and a more developed market.25 Biosimilar applications in the EU are typically reviewed via the Centralized Procedure, where a single application to the EMA results in a marketing authorization that is valid across all EU member states, streamlining market access.8
The United States established its abbreviated pathway for biosimilars much later, with the passage of the Biologics Price Competition and Innovation Act (BPCIA) as part of the Affordable Care Act in 2010.25 The first U.S. biosimilar was not approved until 2015.29 The BPCIA created the 351(k) pathway, which allows biosimilar applicants to rely in part on the FDA’s previous finding of safety and effectiveness for the reference product.13 Both frameworks include periods of data and market exclusivity for the originator biologic to ensure that innovation is rewarded before competition is allowed. In the EU, an originator biologic generally has eight years of data exclusivity and ten years of market exclusivity.1 The BPCIA provides the reference product with four years of data exclusivity and a total of 12 years of market exclusivity from the date of its first licensure.31
The Interchangeability Divide: A Critical Strategic Differentiator
One of the most significant differences between the U.S. and EU regulatory systems—and a point of major strategic importance—is the concept of “interchangeability.”
In the U.S., the BPCIA created a distinct, higher regulatory standard for a biosimilar to be designated as “interchangeable”.11 Historically, achieving this designation required manufacturers to conduct additional, often complex and expensive, clinical “switching studies”.13 These studies were designed to demonstrate that alternating between the reference product and the biosimilar was as safe and effective as remaining on the reference product alone. This two-tiered system created a significant barrier to entry for the interchangeability designation and allowed originator companies to create a perception that non-interchangeable biosimilars were somehow inferior, a narrative that has been used in misinformation campaigns to sow doubt among physicians and patients.33
However, reflecting over a decade of positive real-world experience from Europe and growing confidence in the robustness of the “totality of the evidence” approach, the FDA is now evolving its stance. Recent draft guidance indicates a move away from requiring dedicated switching studies for all products, which would substantially lower the barrier to achieving an interchangeability designation.2 This policy shift represents a major de-risking event for biosimilar developers. It will lower development costs, accelerate the path to an interchangeability designation, and neutralize a key marketing-based advantage held by originators. This signals a global regulatory convergence, suggesting that future competition will focus more intensely on price, manufacturing reliability, and market access rather than on a regulatory designation that was becoming scientifically redundant.
In sharp contrast, the EMA’s position is that any biosimilar approved through its centralized process is, from a scientific standpoint, interchangeable with its reference product.1 The EMA and the Heads of Medicines Agencies (HMA) have issued statements confirming that an approved biosimilar can be used instead of its reference product (or vice versa) or in place of another biosimilar of the same reference product.1 However, the EMA does not have the authority to dictate pharmacy-level substitution policies. That power is deferred to the national health authorities of individual EU member states, creating a fragmented landscape where substitution rules can vary significantly from one country to another.8
This fundamental difference in handling interchangeability has profound strategic implications. In the U.S., the battle is for a federal designation from the FDA. In Europe, the scientific interchangeability is a given upon approval; the subsequent battle for market access and automatic substitution must be fought on a country-by-country basis, requiring a more localized commercial and health policy strategy.
| Feature | U.S. FDA (BPCIA) | European Medicines Agency (EMA) |
| Year Framework Established | 2010 28 | 2005 25 |
| Regulatory Standard | Highly similar with no clinically meaningful differences 11 | Similar in quality, safety, and efficacy 1 |
| Interchangeability Designation | Yes, a separate, higher statutory standard 11 | No, all approved biosimilars are considered scientifically interchangeable 1 |
| Switching Study Requirement | Historically required for interchangeability; now being phased out 11 | Not required; interchangeability is a scientific conclusion 1 |
| Data Exclusivity (Originator) | 4 years 31 | 8 years 1 |
| Market Exclusivity (Originator) | 12 years 31 | 10 (+1) years 1 |
| Substitution Policy Control | Federal designation (FDA), but implementation varies by state law 4 | Delegated to individual EU member states 8 |
The Economic Imperative: Quantifying the Impact of Biosimilar Competition
The driving force behind the global development of biosimilar regulatory pathways is a straightforward economic imperative: to introduce competition into the most expensive sector of the pharmaceutical market and, in doing so, reduce healthcare spending and expand patient access to life-altering therapies. While the concept is simple, the real-world market dynamics are complex, shaped by powerful commercial interests, intricate reimbursement systems, and strategic pricing battles.
The Savings Projections vs. Reality
The potential for biosimilars to generate substantial savings for healthcare systems is immense and well-documented. Numerous economic analyses have projected that the increasing availability of biosimilars will bend the cost curve of biologic spending significantly. Projections from various sources estimate that biosimilars will reduce direct spending on biologic drugs in the U.S. by tens of billions of dollars annually, with cumulative savings expected to surpass $100 billion.36 One prominent analysis by Cardinal Health projected that biosimilars are on track to reduce U.S. drug expenditure by $133 billion by 2025.39 Since the first biosimilar approval in 2015, these products have already saved the U.S. healthcare system over $36 billion.29
These savings are not merely theoretical. They are realized through two primary market mechanisms. First, biosimilars enter the market at a lower price than the originator biologic, offering an immediate cost-effective alternative. Second, the very presence of this competition forces the originator manufacturer to lower its own price to defend its market share.16 This competitive pressure is a powerful force for price erosion. For instance, data shows that, on a weighted average basis, the inflation-adjusted prices for biologics that faced biosimilar competition declined by 56% over a five-year period, while prices for biologics without competition actually increased.16 In some oncology markets, the entry of multiple biosimilars has driven down net prices to 60-70% of the reference product’s pre-competition price.3
The benefits extend beyond budgetary savings. Lower drug costs directly translate into expanded patient access. By making these critical therapies more affordable, biosimilars enable more patients to receive treatment. Analysis has shown that biosimilar competition has facilitated over 344 million additional days of therapy for patients who might otherwise have been unable to access these medicines due to high costs.42 The introduction of filgrastim biosimilars, for example, led to a 20% increase in the number of dispensed doses, reflecting a significant expansion of care for cancer patients.42
The Rebate Wall and PBM Influence: The Hidden Market Distortions
Despite the clear value proposition of lower-cost, equally effective medicines, the uptake of biosimilars in the U.S. has often been slower than anticipated. This is not due to clinical or regulatory failures, but to powerful and often opaque commercial dynamics within the U.S. healthcare system, primarily the phenomenon known as the “rebate wall”.41
The U.S. drug pricing system is dominated by intermediaries called Pharmacy Benefit Managers (PBMs), who negotiate with drug manufacturers on behalf of health insurance plans to determine which drugs will be covered on their formularies.36 A key tool in these negotiations is the rebate. An originator biologic manufacturer with a high list price (also known as the Wholesale Acquisition Cost or WAC) can offer a substantial post-sale rebate back to the PBM and the health plan in exchange for preferred or exclusive placement on the formulary.3
This creates a significant barrier for a new biosimilar, even one with a much lower list price. The PBM’s decision is often based on which product provides the greatest financial return to the plan (and to the PBM itself), which is determined by the net price after rebates are factored in.43 An originator can leverage its high list price to offer a large enough rebate that its net price is competitive with, or even lower than, the biosimilar’s net price. Because PBM revenue models are often tied to a percentage of these rebates, a perverse incentive can arise: the PBM may be financially motivated to favor the high-list-price, high-rebate originator over the low-list-price, low-rebate biosimilar, even if the latter would result in lower overall costs to the healthcare system and lower out-of-pocket costs for patients.44
The 2023 launch of adalimumab (Humira) biosimilars provides a stark case study of this dynamic in action. AbbVie’s Humira was the world’s best-selling drug, with U.S. revenues of $18.6 billion in 2022.3 Multiple biosimilars launched with list prices discounted by as much as 85% from Humira’s WAC.3 Yet, in their first year, these lower-cost alternatives captured only a tiny fraction—around 3%—of the market share.3 The primary reason was that major PBMs chose to keep the high-rebate originator Humira in their preferred formulary positions, effectively blocking access to the less expensive biosimilars for millions of patients.3
This demonstrates that in the U.S. biosimilar market, competition is often not a straightforward contest based on the lowest price. It is a managed market where the financial incentives of powerful intermediaries like PBMs can override the potential for system-wide savings. For a biosimilar manufacturer, a successful go-to-market strategy requires more than just a low price; it demands a sophisticated plan to navigate, disrupt, or otherwise overcome this formidable “rebate wall.”
The Patent Thicket: Navigating IP as the Primary Barrier to Entry
While regulatory hurdles and commercial rebate walls present significant challenges, the most complex and intentionally constructed barrier to biosimilar competition is the intellectual property fortress known as the “patent thicket.” This strategy, perfected by originator biologic manufacturers, is designed to extend a product’s market monopoly long after its foundational patent has expired, transforming the biosimilar development process from a scientific and regulatory challenge into a high-stakes legal and financial gamble.46
Beyond the Primary Patent: The Fortress of Secondary Patents
A patent is a government-granted right that allows an inventor to exclude others from making, using, or selling their invention for a limited period, typically 20 years from the filing date.47 For a new biologic, the most important patent is the core composition-of-matter patent, which protects the molecule itself. In a rational market, the expiration of this patent would open the door to competition.
However, originator companies have developed a strategy of building a dense and overlapping web of dozens, or even hundreds, of secondary patents around a single blockbuster biologic.46 These “patent thickets” are not designed to protect a single core invention but to create a multi-layered legal minefield for any potential competitor. These secondary patents, often filed strategically throughout the drug’s lifecycle, cover a vast array of ancillary characteristics 47:
- Formulations: Patents on specific concentrations, excipients, or buffers used to stabilize the biologic.
- Manufacturing Processes: Patents on proprietary steps in the cell culture, purification, or production process.
- Delivery Devices: Patents on the design of the autoinjector pen or pre-filled syringe used to administer the drug.
- Methods of Use and Dosing: Patents covering the treatment of a specific disease or a particular dosing regimen.
The sheer volume of these patents creates a formidable barrier. The originator manufacturer for Humira (adalimumab), for example, amassed a portfolio of over 100 patents, effectively delaying biosimilar entry in the U.S. for years after it occurred in Europe. This strategy is explicitly designed to deter competition.
“There is no mistaking the intent behind originators’ efforts to obtain, on a single product, scores of patents with overlapping protections — many sought well after the product has launched. During his tenure as Food and Drug Administration (FDA) Commissioner, Scott Gottlieb (2018) described patent thickets around reference biologics as ‘purely designed to deter the entry of approved biosimilars.'” 47
The “Patent Dance”: A Complex and Costly Litigation Framework
The BPCIA established a unique, highly structured process for resolving patent disputes between originator and biosimilar manufacturers, colloquially known as the “patent dance”.31 This framework involves a series of confidential information exchanges and negotiation deadlines designed to identify the specific patents that will be the subject of litigation before the biosimilar launches.31
While the Supreme Court’s decision in Sandoz v. Amgen confirmed that participation in this dance is optional for the biosimilar applicant, engaging in the process can offer strategic advantages by narrowing the scope of potential litigation.31 However, when confronted with a patent thicket, this process can become overwhelmingly complex and costly. The biosimilar manufacturer is faced with the daunting task of assessing the validity and potential infringement of hundreds of patent claims and then engaging in protracted legal battles that can cost tens of millions of dollars and last for years.46
The patent thicket thus functions as a powerful financial weapon. The primary goal is not necessarily to win every court case on the merits. Instead, the objective is to create a risk-reward calculation for the biosimilar challenger that is so daunting it forces a settlement favorable to the originator. A biosimilar company, having already invested $100-300 million in development, must then weigh the massive, uncertain cost of litigating dozens of patents against the certainty of a settlement that allows for market entry on a specific, albeit delayed, date.2 This legal risk systematically erodes the projected value of the biosimilar project, often making a delayed launch the most financially prudent, if anti-competitive, outcome. This preserves a significant portion of the originator’s monopoly profits and delays patient access to lower-cost medicines.
Legislative and Regulatory Countermeasures
Recognizing the anti-competitive nature of patent thickets, policymakers and advocacy groups have proposed several reforms to level the playing field. These proposals aim to curb the abuse of the patent system without undermining the incentives for true innovation.46 Key proposed solutions include:
- Capping Asserted Patents: Legislation has been introduced in the U.S. Congress to limit the number of patents an originator can assert in BPCIA litigation to a more reasonable number, preventing them from overwhelming challengers with sheer volume.
- Strengthening Patent Quality: Reforms at the U.S. Patent and Trademark Office (USPTO) to apply greater scrutiny to secondary patent applications, reducing the issuance of weak or duplicative patents that primarily serve to thicken the legal portfolio.
- Providing Safe Harbor for “Skinny Labeling”: Creating clear legal protections for biosimilar manufacturers who “carve out” or omit patented indications from their product labeling, allowing them to launch for non-patented uses without risking infringement litigation on the patented methods of use.
These countermeasures reflect a growing awareness that for a robust biosimilar market to flourish, the rules of engagement must be rebalanced to prevent the patent system from being used as a tool to indefinitely suppress legitimate competition.
From Data to Dominance: A Playbook for Competitive Intelligence
In the high-stakes, legally complex world of biosimilars, success is not merely a function of scientific capability; it is a direct result of strategic foresight. The companies that thrive are those that can accurately anticipate market events, competitor actions, and legal challenges years in advance. The key to this foresight lies in a disciplined and sophisticated approach to competitive intelligence (CI), with the analysis of patent and regulatory data at its core. Passive observation is insufficient; winning requires an active, intelligence-driven strategy that transforms raw data into a decisive competitive advantage.48
The Strategic Value of Patent Intelligence
A superficial approach to IP analysis—simply noting the expiration date of a reference product’s primary composition-of-matter patent—is a recipe for failure. A winning strategy requires a deep, analytical dive into the entire IP landscape of a target molecule. This involves mapping the originator’s defensive fortress, identifying its strongest and weakest points, and using that intelligence to chart the most efficient path to market.49
Effective patent intelligence allows a company to:
- Deconstruct the Patent Thicket: Systematically identify, categorize, and analyze every patent associated with a reference biologic, including secondary patents for formulations, manufacturing processes, and methods of use.47
- Assess Litigation Risk: Evaluate the relative strength of each patent by examining its prosecution history, prior art, and the outcomes of similar patent challenges in the U.S. and other jurisdictions like the EU.31
- Anticipate Originator Strategy: Use the timing and nature of patent filings to infer the originator’s lifecycle management plans and predict which patents they are most likely to assert in litigation.48
- Inform “At-Risk” Launch Decisions: Make a data-driven assessment of the legal risks associated with launching a biosimilar before all patent litigation is fully resolved—a high-risk, high-reward strategy that can secure a significant first-mover advantage.
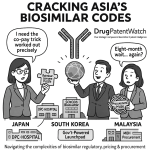
Leveraging Specialized Tools: The Role of DrugPatentWatch
Conducting this level of analysis requires specialized tools and expertise. Comprehensive business intelligence platforms are indispensable for aggregating and analyzing the vast amounts of patent, regulatory, and clinical trial data necessary for strategic planning. A service like DrugPatentWatch provides a centralized, real-time database that is critical for this work.31 Such platforms empower strategic teams by:
- Tracking the Entire IP and Regulatory Landscape: They provide up-to-the-minute information on patent expirations, new patent filings, patent litigation status (including challenges at the Patent Trial and Appeal Board, or PTAB), and regulatory milestones like FDA approvals and clinical trial updates.31
- Mapping the Competitive Field: These tools allow a company to identify all other biosimilar developers targeting the same reference product, monitor their clinical trial progress, and analyze their public statements and IP strategies. This is crucial for forecasting the level of competition and future pricing pressure upon market entry.49
- Facilitating Strategic Decision-Making: By integrating disparate data streams—legal, regulatory, and commercial—these platforms provide the holistic view needed to make critical go/no-go decisions on development programs, prioritize targets, formulate legal strategies, and negotiate more favorable settlement terms.48
Case Study: Strategic Planning for a Hypothetical Biosimilar Launch
To illustrate the practical application of CI, consider a mid-sized biotech company (“BioChallenge”) evaluating the development of a biosimilar for “InnovateMab,” a blockbuster monoclonal antibody with a primary patent expiring in five years.
- Initial Screen (The Data): Using a platform like DrugPatentWatch, BioChallenge’s CI team immediately discovers that InnovateMab is protected not by one patent, but by a thicket of over 60 secondary patents covering formulations, delivery devices, and specific indications.47
- Landscape Analysis (The Intelligence): The platform reveals that two larger competitors, “Goliath Pharma” and “Global Bio,” are already in Phase 3 clinical trials for their InnovateMab biosimilars.53 This signals a crowded and highly competitive future market.
- Deep Dive and Opportunity Identification (The Insight): The CI team digs deeper. They find that one of the key formulation patents, set to expire eight years from now, was successfully invalidated in Germany during a recent legal battle with Goliath Pharma.50 The German court’s reasoning, based on prior art, appears directly applicable under U.S. patent law. Simultaneously, they note that the originator’s delivery device patent is considered very strong, with no obvious path to invalidation.
- Strategic Pivot (The Action): Armed with this intelligence, BioChallenge’s leadership team makes a series of strategic decisions. They decide not to compete head-to-head with Goliath and Global Bio on the standard pre-filled syringe presentation. Instead, they pivot their development strategy to focus on a vial-and-syringe presentation for hospital use, designing around the device patent. They also direct their legal team to build an invalidity case against the U.S. formulation patent, using the German decision as a roadmap. This CI-driven strategy allows them to enter a less crowded market segment with a clearer, de-risked legal pathway, transforming a high-risk proposition into a calculated strategic entry.
This integrated analysis transforms raw data into predictive intelligence, allowing a company to proactively shape its strategy rather than reactively responding to the originator’s moves.
| Reference Product (Brand Name) | Active Ingredient | Key Therapeutic Area | Annual Sales (USD, approx.) | Primary Patent Expiry (U.S.) | Number of Known Biosimilars in Development | Status of Leading Biosimilar Candidate(s) |
| Keytruda | Pembrolizumab | Oncology | ~$25 Billion | 2028 | 14+ 55 | Multiple in Phase 3 trials (e.g., Samsung Bioepis SB27) 55 |
| Stelara | Ustekinumab | Immunology | ~$10 Billion | 2023 | 5+ Approved | Multiple launched (e.g., Amjevita, Wezlana) |
| Eylea | Aflibercept | Ophthalmology | ~$6 Billion | 2023 | 2 Approved | Approvals granted (e.g., Yesafili, Opuviz) 46 |
| Opdivo | Nivolumab | Oncology | ~$9 Billion | 2028 | In Development | Early-to-mid stage clinical trials |
| Dupixent | Dupilumab | Immunology | ~$11 Billion | ~2031 | 0 55 | Pre-clinical / Not yet in clinical development 55 |
| Prolia/Xgeva | Denosumab | Bone Health | ~$6 Billion | 2025 | 2 Approved | Approvals granted (e.g., Jubbonti, Wyost) 46 |
Winning Hearts and Minds: Overcoming Commercial and Clinical Adoption Hurdles
Securing regulatory approval and navigating the patent minefield are monumental achievements, but they only get a biosimilar to the starting line. The final, crucial battle is for market adoption—winning the confidence of the physicians who prescribe these medicines and the patients who take them. Despite a robust body of evidence confirming their safety and efficacy, biosimilars face significant commercial and clinical hurdles rooted in uncertainty, misinformation, and ingrained habits. Overcoming these barriers requires a proactive strategy centered on education and the powerful validation of real-world evidence (RWE).
The Confidence Gap: Addressing Physician and Patient Hesitancy
Even with the FDA’s and EMA’s stamps of approval, a “confidence gap” can persist among stakeholders.56 Physicians, accustomed to years of experience with a reference biologic, may be hesitant to switch a stable patient to a new product, fearing a loss of efficacy or an unexpected adverse event.56 Patients, in turn, may be anxious about switching, especially if the change is driven by insurance mandates rather than a direct clinical need. This anxiety can sometimes manifest as the “nocebo” effect, where negative expectations about a treatment lead to the perception of negative outcomes, regardless of the drug’s actual pharmacological effect.57
These concerns are often fueled by a lack of understanding of the rigorous science underpinning biosimilar approval. A 2022 survey in South Korea found that while 66% of patients had heard of biosimilars, 55% were unfamiliar with their definition, and 50% lacked confidence in their safety and efficacy.60 Similarly, surveys of U.S. and European healthcare providers have revealed knowledge gaps and concerns that limit prescribing, particularly for patients already stable on a biologic.58
Combating Misinformation
This confidence gap is often exploited and widened by misinformation campaigns, which can be driven or funded by brand manufacturers seeking to protect their market share.33 These campaigns frequently seize on the scientifically accurate but easily misinterpreted fact that biosimilars are “not identical” to their reference products to sow doubt about their equivalence in performance.62 They may also leverage the FDA’s two-tiered system to imply that a biosimilar without an “interchangeable” designation is somehow less safe or effective, a claim the FDA has explicitly refuted.33 Former FDA Commissioner Scott Gottlieb directly addressed this issue, stating he was “worried that there are either deliberate or unintentional efforts by branded companies to create confusion about the safety and effectiveness of unbranded biologic drugs”.33 This misinformation can slow adoption, undermine trust in regulatory bodies, and ultimately limit patient access to more affordable care.
The Power of Real-World Evidence (RWE)
The most potent antidote to misinformation and clinical uncertainty is robust, transparent real-world evidence. While randomized controlled trials (RCTs) are the gold standard for regulatory approval, they are conducted in controlled settings with specific patient populations. RWE, gathered from large patient registries, insurance claims databases, and routine clinical practice, demonstrates how a medicine performs in the messy, diverse reality of healthcare.64 For biosimilars, RWE serves a dual strategic purpose: it is a clinical tool to validate long-term safety and efficacy and a commercial tool to neutralize the primary non-economic barriers to adoption.
The accumulated RWE for first-generation biosimilars is overwhelming and provides a powerful narrative of success that can be leveraged for future launches.
- Case Study 1: Infliximab (Remicade) Biosimilars: The introduction of infliximab biosimilars was a critical test case. The landmark NOR-SWITCH study, a large, randomized, double-blind trial, was specifically designed to test the safety of switching patients from the reference product Remicade to the biosimilar CT-P13. The study met its primary endpoint, demonstrating that switching was not inferior to remaining on the originator.65 This pivotal trial, combined with extensive subsequent data from national registries like the DANBIO registry in Denmark, provided a mountain of evidence that gave clinicians and health systems the confidence to broadly adopt infliximab biosimilars, leading to massive cost savings.65
- Case Study 2: Adalimumab (Humira) Biosimilars: As adalimumab biosimilars have rolled out, RWE has been crucial in validating their performance. A large European cross-sectional study involving over 1,200 patients with various autoimmune diseases found that both patients initiating an adalimumab biosimilar (ABP 501) and those switching from Humira experienced positive treatment outcomes.66 Critically, both physicians and patients reported high levels of satisfaction with the biosimilar’s disease control, even when the switch was mandated by insurance for non-clinical, financial reasons.66 This RWE directly addresses the core concern of switching stable patients, showing that outcomes are maintained.
- Case Study 3: Etanercept (Enbrel) Biosimilars: Real-world cohort studies comparing reference etanercept to its biosimilars have consistently reinforced the findings from approval-level RCTs. A study comparing the biosimilar GP2015 to Enbrel in rheumatoid arthritis patients found no statistically significant differences in effectiveness, as measured by disease activity scores (DAS28-CRP), remission rates, or low disease activity rates over 52 weeks.68 Furthermore, treatment persistence—a key indicator of a drug’s long-term effectiveness and tolerability in the real world—was nearly identical, with drug survival rates of 82% for the originator and 80% for the biosimilar.68
This wealth of RWE across multiple molecules and therapeutic areas confirms a consistent pattern: approved biosimilars perform as expected in the real world, and switching from an originator is safe and effective. For a biosimilar manufacturer, investing in the generation and dissemination of RWE is not just a post-marketing requirement; it is a critical commercial strategy to accelerate uptake, build a moat of clinical confidence, and effectively counter the fear, uncertainty, and doubt that can impede market access.
The Next Decade for Biosimilars: Future Trends and Strategic Outlook
The first decade of the biosimilar era has been a period of foundation-building, characterized by scientific validation, regulatory pathway development, and the first waves of market entry. The next decade promises to be one of acceleration and expansion, where the full economic and clinical potential of biosimilars may be unleashed. However, this future is not guaranteed. It will be shaped by evolving regulatory philosophies, the increasing complexity of biologic targets, and the critical question of long-term market sustainability. Companies that can anticipate and adapt to these trends will be positioned for success.
The Evolving Regulatory Environment
A key trend shaping the future is the global regulatory convergence toward more streamlined, science-driven approval pathways. Regulators, armed with over a decade of positive experience, are increasingly confident in the power of advanced analytical techniques to determine biosimilarity. This is leading to a re-evaluation of the need for large, duplicative clinical efficacy trials. The EMA has long championed a “tailored clinical approach,” and recent actions by the FDA, such as the move to eliminate the requirement for switching studies to achieve interchangeability, signal a strong alignment with this philosophy.2
As Gillian Woollett, a leading regulatory expert at Samsung Bioepis, has noted, eliminating unnecessary clinical trial requirements could potentially halve the time and cost of developing a biosimilar.70 This regulatory evolution is perhaps the most significant tailwind for the industry, as it lowers the formidable barriers to entry, reduces development risk, and could encourage more manufacturers to invest in the biosimilar pipeline.
New Frontiers: Expansion and Complexity
The next wave of biosimilar competition will move beyond the initial targets in immunology and supportive cancer care into new and more complex therapeutic areas. Experts anticipate significant growth in biosimilars for ophthalmology (e.g., biosimilars to Eylea), bone health (e.g., biosimilars to Prolia), and even orphan diseases, a market with $33 billion in annual revenue from biologics facing patent expiry in the next decade.71
Simultaneously, the complexity of the biologic targets themselves will increase. The looming patent expirations for first-generation immuno-oncology blockbusters like Keytruda (pembrolizumab) present both a massive commercial opportunity and a profound scientific challenge.55 Developing a biosimilar for a complex monoclonal antibody that works by modulating the patient’s own immune system will require an even higher degree of manufacturing precision and analytical sophistication.
The Sustainability Question: Ensuring a Viable Market
Despite the immense opportunity—an estimated $234 billion in sales from biologics losing patent protection over the next ten years—there are serious questions about the long-term sustainability of the biosimilar market.71 The challenges are significant. As Dracey Poore of Cardinal Health points out, of the 118 biologics set to lose exclusivity in the coming decade, only 10% currently have biosimilars in the development pipeline.71
Several factors threaten the economic viability that is necessary to encourage investment:
- Market Barriers: Persistent challenges, including patent thickets and the “rebate wall” in the U.S., can delay or limit market access to such an extent that the return on a $100-300 million investment becomes uncertain.45
- Price Erosion: While beneficial for payers, intense competition among multiple biosimilar players can drive prices down to a level where manufacturing becomes unprofitable, potentially leading to market withdrawals and future drug shortages, similar to the dynamics seen in the small-molecule generics market.41
- Policy Headwinds: New policies, such as the Medicare Drug Price Negotiation Program in the U.S., could fundamentally alter the economics of the pharmaceutical market. By allowing the government to set prices for certain high-spend drugs, including biologics, these programs could significantly reduce the revenue potential for both originators and the biosimilars that would eventually compete with them, thereby undermining the financial incentive to develop biosimilars in the first place.70
Concluding Analysis
The future of the biosimilar market rests on a delicate and dynamic balance. Continued progress requires a multi-pronged effort from all stakeholders. Regulators must continue to advance streamlined, science-based pathways that lower barriers to entry without compromising safety. Policymakers must enact effective measures to counteract anti-competitive IP strategies and commercial practices that stifle competition. Payers and health systems must create reimbursement and formulary structures that incentivize the use of lower-cost, high-value biosimilars.
For manufacturers, the path forward is clear, if challenging. Success will demand more than just scientific excellence. It will require regulatory fluency to navigate evolving global standards. It will demand commercial savvy to overcome entrenched market barriers. And most importantly, it will require a mastery of strategic IP and competitive intelligence to successfully challenge patent fortresses and carve out a viable market position. The companies that can integrate these three pillars—science, regulation, and strategy—will not only survive but will lead the next wave of biosimilar innovation, delivering value to patients, payers, and their shareholders alike.
Key Takeaways
- Biosimilars Are Not Generics: The fundamental scientific difference—”highly similar” vs. “identical”—drives a completely distinct regulatory, economic, and commercial model. This results in far higher development costs ($100M-$300M) and more modest price discounts (15-50%) for biosimilars compared to generics.
- Regulatory Approval is Rigorous and Trustworthy: Both the FDA and EMA use a “totality of the evidence” approach, founded on extensive analytical data, to ensure biosimilars have no clinically meaningful differences from their reference products. Accumulated real-world evidence from millions of patient-days confirms their safety and efficacy.
- Patent Thickets are the Primary Barrier to Competition: Originator companies strategically build dense webs of secondary patents to create prohibitive legal and financial risks for biosimilar developers. This tactic is the single greatest impediment to timely market entry and must be the central focus of any competitive strategy.
- Patent Intelligence is the Key to Competitive Advantage: Success in the biosimilar market is less about the science of replication and more about the strategy of litigation and market timing. Proactive, sophisticated use of competitive intelligence tools like DrugPatentWatch to deconstruct patent thickets and anticipate competitor moves is not optional—it is essential for survival and success.
- Commercial Hurdles Can Override Price Advantages: In the U.S. market, the “rebate wall” created by PBMs can block access to lower-list-price biosimilars in favor of high-rebate originators. A successful launch strategy must address these commercial dynamics and cannot rely on a low price alone.
- Real-World Evidence is a Powerful Commercial Tool: Beyond satisfying regulatory requirements, generating and disseminating real-world evidence is a critical strategy to build physician and patient confidence, counter misinformation from competitors, and accelerate market adoption.
- The Market is at a Critical Juncture: While the next decade holds over $230 billion in biosimilar opportunities, significant headwinds related to market sustainability, policy changes, and originator tactics threaten long-term viability. Strategic alignment among all stakeholders is required to realize the full cost-saving and access-expanding potential of biosimilars.
Frequently Asked Questions (FAQ)
1. If a biosimilar is “highly similar” but not “identical,” how can we be sure it’s just as safe and effective?
Regulators like the FDA and EMA approve a biosimilar only after a rigorous scientific evaluation based on the “totality of the evidence”.8 This process starts with extensive analytical studies that compare the molecular structure and biological function of the biosimilar and its reference product. These tests are highly sensitive and establish a foundational level of similarity. This is followed by clinical pharmacology studies to ensure both medicines behave the same way in the human body. If any uncertainty remains, a comparative clinical trial may be required. The goal is to demonstrate that there are “no clinically meaningful differences” in safety, purity, and potency.11 Decades of experience in Europe and nearly a decade in the U.S. have shown that this process is robust, and approved biosimilars can be used with the same confidence as their reference products.1
2. Why do biosimilars cost more than generic drugs?
The cost difference is a direct result of their underlying complexity. Generic drugs are exact chemical copies of small-molecule drugs and can be developed in about two years for $1-4 million because they do not require extensive clinical testing.6 Biologics, however, are large, complex molecules made in living cells that cannot be copied exactly. Developing a biosimilar is a far more complex and expensive process, requiring reverse-engineering the product, developing a unique manufacturing process, and conducting extensive analytical and clinical studies to prove biosimilarity. This process typically takes six to nine years and costs between $100 million and $300 million.2 These much higher development costs necessitate a higher market price to ensure a viable return on investment.
3. What is a “patent thicket,” and why is it the biggest challenge for biosimilar competition?
A “patent thicket” is a defensive strategy used by originator companies where they file dozens or even hundreds of secondary patents around a single biologic drug.46 These patents cover not just the core molecule but also formulations, manufacturing methods, delivery devices, and dosing regimens. This creates a dense, overlapping legal barrier designed to make it prohibitively expensive and time-consuming for a biosimilar manufacturer to challenge in court.46 The goal is not always to win every lawsuit but to create so much legal risk and uncertainty that the biosimilar company is forced to either abandon its project or agree to a settlement that delays its market launch for several years, thereby extending the originator’s monopoly.47
4. What is the difference between a “biosimilar” and an “interchangeable biosimilar,” and does it matter for patient outcomes?
Both a biosimilar and an interchangeable biosimilar are proven to be equally safe and effective as the reference product, with no clinically meaningful differences.11 There is no difference in expected patient outcomes between them. The distinction is a regulatory one specific to the U.S. that governs how the medicine can be dispensed. A standard biosimilar must be prescribed by name. An “interchangeable” biosimilar has met additional regulatory requirements that allow a pharmacist to substitute it for the reference product without consulting the prescriber, similar to how generics are substituted for brand-name drugs (subject to state laws).4 The FDA is currently streamlining the process to obtain an interchangeable designation, reflecting the strong safety record of all biosimilars.34
5. How can my company use patent data from a service like DrugPatentWatch to gain a competitive advantage in the biosimilar market?
A platform like DrugPatentWatch transforms patent data from a simple compliance check into a powerful strategic weapon. A company can use it to:
- Identify Opportunities and Threats: Get a comprehensive, real-time view of the entire patent landscape for a target biologic, including all secondary patents and their expiration dates.51
- Analyze Competitors: Track all other biosimilar developers for a given target, monitoring their clinical trial progress and regulatory filings to anticipate the level of competition and timing of market entry.49
- De-Risk Legal Strategy: Analyze the outcomes of prior patent litigation and PTAB challenges for similar patents to assess the likelihood of successfully invalidating key patents in the thicket, thereby informing legal strategy and settlement negotiations.31
- Inform Strategic Decisions: Integrate IP, regulatory, and commercial data to make more informed decisions on which products to pursue, when to launch, and how to position the product for maximum market access.48 This turns static data into actionable intelligence for market dominance.
References
- Biosimilar medicines: Overview | European Medicines Agency (EMA), accessed July 30, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/biosimilar-medicines-overview
- The FDA’s Biosimilar Burden—and How Congress Can Lift It | Cato at Liberty Blog, accessed July 30, 2025, https://www.cato.org/blog/fdas-biosimilar-burden-how-congress-can-lift-it
- Sustaining competition for biosimilars on the pharmacy benefit: Use it or lose it – JMCP.org, accessed July 30, 2025, https://www.jmcp.org/doi/10.18553/jmcp.2024.30.6.600
- Biosimilar and Interchangeable Biologics: More Treatment Choices – FDA, accessed July 30, 2025, https://www.fda.gov/consumers/consumer-updates/biosimilar-and-interchangeable-biologics-more-treatment-choices
- Understanding Biologic and Biosimilar Drugs, accessed July 30, 2025, https://www.fightcancer.org/policy-resources/understanding-biologic-and-biosimilar-drugs
- Biosimilar vs Generic Drugs: Key Differences in Healthcare – Medical Packaging Inc, accessed July 30, 2025, https://medpak.com/biosimilar-vs-generic-drugs/
- How Similar Are Biosimilars? What Do Clinicians Need to Know …, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5669137/
- An Overview of Biosimilar Regulatory Approvals by the EMA and …, accessed July 30, 2025, https://www.drugpatentwatch.com/blog/the-biosimilar-landscape-an-overview-of-regulatory-approvals-by-the-ema-and-fda/
- Biosimilar vs. Generic Drugs: 4 Similarities and Differences You Should Know – GoodRx, accessed July 30, 2025, https://www.goodrx.com/drugs/biologics/biosimilar-vs-generic
- Exploring Biosimilars as a Drug Patent Strategy: Navigating the Complexities of Biologic Innovation and Market Access – DrugPatentWatch, accessed July 30, 2025, https://www.drugpatentwatch.com/blog/exploring-biosimilars-as-a-drug-patent-strategy-navigating-the-complexities-of-biologic-innovation-and-market-access/
- 9 Things to Know About Biosimilars and Interchangeable Biosimilars – FDA, accessed July 30, 2025, https://www.fda.gov/drugs/things-know-about/9-things-know-about-biosimilars-and-interchangeable-biosimilars
- Biological Product Definitions | FDA, accessed July 30, 2025, https://www.fda.gov/files/drugs/published/Biological-Product-Definitions.pdf
- Biosimilar Product Regulatory Review and Approval | FDA, accessed July 30, 2025, https://www.fda.gov/files/drugs/published/Biosimilar-Product-Regulatory-Review-and-Approval.pdf
- Differentiating Biosimilars From Generic Drugs – American Journal of Managed Care, accessed July 30, 2025, https://www.ajmc.com/view/differentiating-biosimilars-from-generic-drugs
- Review and Approval – FDA, accessed July 30, 2025, https://www.fda.gov/drugs/biosimilars/review-and-approval
- Biosimilars Often Reduce Prices by 50 Percent or More – Pacific Research Institute, accessed July 30, 2025, https://www.pacificresearch.org/biosimilars-often-reduce-prices-by-50-percent-or-more/
- The Cost Savings Potential of Biosimilar Drugs in the United States – RAND Corporation, accessed July 30, 2025, https://www.rand.org/content/dam/rand/pubs/perspectives/PE100/PE127/RAND_PE127.pdf
- Biosimilars and Generic Drugs in Cancer Care: What to Know, accessed July 30, 2025, https://www.cancercenter.com/community/blog/2024/07/biosimilars-generic-drugs-cancer
- The biosimilar approval process: how different is it? – Considerations In Medicine, accessed July 30, 2025, https://considerations.bmj.com/content/1/1/3
- Biosimilar Medicines: From Development Process to Marketing …, accessed July 30, 2025, https://www.mdpi.com/2076-3417/14/17/7529
- Data Requirements for Biosimilars – YouTube, accessed July 30, 2025, https://www.youtube.com/watch?v=xHvU4rZtWa4
- Fact sheet 3: Introduction to Biosimilars & Regulatory Requirements – IFPMA, accessed July 30, 2025, https://www.ifpma.org/wp-content/uploads/2023/01/i2023_factsheet3.pdf
- Scientific Considerations in Demonstrating Biosimilarity to a Reference Product Guidance for Industry – FDA, accessed July 30, 2025, https://www.fda.gov/media/82647/download
- How the U.S. Compares to Europe on Biosimilar Approvals and Products In the Pipeline (UPDATED) | JD Supra, accessed July 30, 2025, https://www.jdsupra.com/legalnews/how-the-u-s-compares-to-europe-on-3189962/
- What Is a Biosimilar? FDA vs. EMA Approval Requirements Compared – Patsnap Synapse, accessed July 30, 2025, https://synapse.patsnap.com/article/what-is-a-biosimilar-fda-vs-ema-approval-requirements-compared
- Lessons for the United States from Europe’s Biosimilar Experience, accessed July 30, 2025, https://biosimilarscouncil.org/wp-content/uploads/2020/06/EuropeBiosimilars_June_2020.pdf
- Biosimilars: The Debate Continues – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3200229/
- Biosimilarity and Interchangeability in the Biologics Price Competition and Innovation Act of 2009 and FDA’s 2012 Draft Guidance for Industry – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3827854/
- Biosimilars improve patient access to quality medicines – FDA, accessed July 30, 2025, https://www.fda.gov/media/161628/download
- Understanding Interchangeable Biosimilars at the Federal and State Levels, accessed July 30, 2025, https://www.ajmc.com/view/understanding-interchangeable-biosimilars-at-the-federal-and-state-levels
- Predicting Patent Litigation Outcomes for Biosimilars: Navigating the Complex Landscape of Pharmaceutical Innovation for Biosimilars – DrugPatentWatch, accessed July 30, 2025, https://www.drugpatentwatch.com/blog/predicting-patent-litigation-outcomes-for-biosimilars/
- Challenges for the regulation of biosimilars, accessed July 30, 2025, https://gabionline.net/biosimilars/research/Challenges-for-the-regulation-of-biosimilars
- Misinformation on Biosimilars Costs Billions, Harms Patients, and Sows Unnecessary Doubt Around FDA-Approved Products, accessed July 30, 2025, https://biosimilarscouncil.org/resource/misinformation-biosimilars-costs-billions-harms-patients-sows-unnecessary-doubt-fda-approved-products/
- Draft FDA Guidance No Longer Requires Biosimilar Switching Studies – The Rheumatologist, accessed July 30, 2025, https://www.the-rheumatologist.org/article/draft-fda-guidance-no-longer-requires-biosimilar-switching-studies/
- Difference between us and eu biosimilar markets | Insights – ICON plc, accessed July 30, 2025, https://www.iconplc.com/insights/blog/2020/05/27/the-differences-between-the-us-and-eu-biosimilar-markets
- Biosimilar Cost Savings in the United States: Initial Experience and Future Potential – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6075809/
- Projected US Savings From Biosimilars, 2021-2025 – American Journal of Managed Care, accessed July 30, 2025, https://www.ajmc.com/view/projected-us-savings-from-biosimilars-2021-2025
- Increase Patient Access to Biosimilars in 2022, accessed July 30, 2025, https://biosimilarscouncil.org/resource/increase-patient-access-to-biosimilars-in-2022/
- Impact of Biosimilars on Treatment Landscape in US and EU – Aranca, accessed July 30, 2025, https://www.aranca.com/knowledge-library/articles/business-research/impact-of-biosimilars-on-treatment-landscape-in-us-and-eu
- 2022 Biosimilars Report: The U.S. Journey and Path Ahead – Cardinal Health, accessed July 30, 2025, https://www.cardinalhealth.com/content/dam/corp/web/documents/Report/cardinal-health-2022-biosimilars-report.pdf
- The U.S. Generic & Biosimilar Medicines Savings Report, accessed July 30, 2025, https://accessiblemeds.org/wp-content/uploads/2025/01/AAM-2024-Generic-Biosimilar-Medicines-Savings-Report.pdf
- Biosimilars in Focus: Advancing Implementation in Health Care Systems, accessed July 30, 2025, https://www.ajmc.com/view/biosimilars-in-focus-advancing-implementation-in-health-care-systems
- The Rebate War: How Originator Companies Are Fighting Back Against Biosimilars, accessed July 30, 2025, https://www.centerforbiosimilars.com/view/the-rebate-war-how-originator-companies-are-fighting-back-against-biosimilars
- AHIP’s latest misinformation campaign & what it’s trying to hide – PhRMA, accessed July 30, 2025, https://phrma.org/blog/ahips-latest-misinformation-campaign-and-what-its-trying-to-hide
- Navigating Biosimilars: Expert Perspectives on Integration …, accessed July 30, 2025, https://www.ajmc.com/view/navigating-biosimilars-expert-perspectives-on-integration-challenges-and-future-trends-within-health-systems
- Clearing the Thicket: New Report Outlines Legislative Fixes to Boost …, accessed July 30, 2025, https://www.centerforbiosimilars.com/view/clearing-the-thicket-new-report-outlines-legislative-fixes-to-boost-biosimilar-access
- How Patent Thickets Constrain the US Biosimilars Market and Domestic Manufacturing – Matrix Global Advisors, accessed July 30, 2025, https://getmga.com/wp-content/uploads/2022/04/PatentThickets_May2021_FINAL.pdf
- Why Competitive Intelligence Is My Secret Weapon in the …, accessed July 30, 2025, https://www.proactiveworldwide.com/resources/healthcare-pulse/why-competitive-intelligence-is-my-secret-weapon-in-the-biosimilars-battle/
- Optimally Leveraging Biosimilars Competitive Intelligence in the Pharma Industry, accessed July 30, 2025, https://www.biopharmavantage.com/biosimilars-competitive-intelligence
- Biosimilars patent litigation in the EU and the US: a comparative strategic overview – GaBIJ, accessed July 30, 2025, https://gabi-journal.net/biosimilars-patent-litigation-in-the-eu-and-the-us-a-comparative-strategic-overview.html
- Online Course: Business intelligence for bio/pharma drugs – DrugPatentWatch from Udemy, accessed July 30, 2025, https://www.classcentral.com/course/udemy-generic-drug-portfolio-branded-drug-lifecycle-management-401093
- The Coming of Age of Biosimilars: A Personal Perspective – OUCI, accessed July 30, 2025, https://ouci.dntb.gov.ua/en/works/4LgAYd67/
- Biosimilars (US and EU) Strategic Pharmaceutical CI Insights – DataMintelligence, accessed July 30, 2025, https://www.datamintelligence.com/strategic-insights/biosimilars-us-and-eu
- Case Study: Competitive Intelligence on Clinical Trials for Biosimilar Drug to Treat Multiple Sclerosis – Emerging Strategy, accessed July 30, 2025, https://www.emerging-strategy.com/case-study-competitive-intelligence-on-clinical-trials-for-biosimilar-drug-to-treat-multiple-sclerosis/
- Application error: a client-side exception has occurred, accessed July 30, 2025, https://www.pharmacytimes.com/view/the-future-of-top-selling-biologics-biosimilars-on-the-rise
- ASHP Midyear: Biosimilars Offer Cost Savings, But Barriers to Adoption Remain, accessed July 30, 2025, https://www.clearwayhealth.com/post/ashp-midyear-biosimilars-offer-cost-savings-but-barriers-to-adoption-remain
- Identification of Barriers Preventing Biosimiliar Oncology Medication …, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9696566/
- Provider and Patient Knowledge Gaps on Biosimilars: Insights From Surveys, accessed July 30, 2025, https://www.ajmc.com/view/biosimilarssuppl-insightssurveys
- Adalimumab Double Take: The Unexpected Return to Reference Humira, accessed July 30, 2025, https://www.centerforbiosimilars.com/view/adalimumab-double-take-the-unexpected-return-to-reference-humira
- Unaware and unpowered: evaluating patient perceptions and preferences of biosimilars in South Korea – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11949777/
- Misinformation on Biosimilars Undermines Patient and Prescriber Confidence, accessed July 30, 2025, https://biosimilarscouncil.org/resource/misinformation-on-biosimilars-undermines-patient-and-prescriber-confidence/
- Correct Patient Misconceptions Around Biosimilars – Pharmacy Times, accessed July 30, 2025, https://www.pharmacytimes.com/view/correct-patient-misconceptions-around-biosimilars
- Biosimilar considerations for prescribers – Accord BioPharma, accessed July 30, 2025, https://www.accordbiopharma.com/biosimilar-for-prescribers/
- What role for real-world evidence in market access of biosimilars? – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11891046/
- Clinical trial and ‘real-world’ data support switching from a bio …, accessed July 30, 2025, https://ard.bmj.com/content/79/4/e44
- Real-World Experience with an Adalimumab Biosimilar (ABP 501) in …, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12084434/
- European Data Confirm Real-World Benefits of Adalimumab Biosimilars, accessed July 30, 2025, https://www.centerforbiosimilars.com/view/european-data-confirms-real-world-benefits-of-adalimumab-biosimilars
- Real-world effectiveness and persistence of reference … – Frontiers, accessed July 30, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.980832/full
- Real-world effectiveness and persistence of reference etanercept versus biosimilar etanercept GP2015 among rheumatoid arthritis patients: A cohort study – PubMed, accessed July 30, 2025, https://pubmed.ncbi.nlm.nih.gov/36263118/
- Ep. 89 – Delivering on the biosimilars promise, a conversation with Gillian Woollett, accessed July 30, 2025, https://www.youtube.com/watch?v=yLMBOgbp8DI
- Expert: Navigating the Next Decade of Market Growth and Innovation for Biosimilars, accessed July 30, 2025, https://www.pharmacytimes.com/view/expert-navigating-the-next-decade-of-market-growth-and-innovation-for-biosimilars
- The Future of Biosimilars: Q&A with Matt Erick – Pharmaceutical Executive, accessed July 30, 2025, https://www.pharmexec.com/view/future-biosimilars-matt-erick
- Assessing the Biosimilar Void in the U.S. – IQVIA, accessed July 30, 2025, https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/assessing-the-biosimilar-void-in-the-us
- Interviews – Center for Biosimilars, accessed July 30, 2025, https://www.centerforbiosimilars.com/interviews
- Biologics, Biosimilars, and Interchangeable Biosimilars—What is the Difference?, accessed July 30, 2025, https://www.arthritis-health.com/treatment/medications/biologics-biosimilars-and-interchangeable-biosimilars-what-difference
- Difference between generic drugs and biosimilar drugs | Gouvernement du Québec, accessed July 30, 2025, https://www.quebec.ca/en/health/medications/biosimilar-drugs/difference-between-generic-drugs-and-biosimilar-drugs
- Biosimilars in Clinical Trials: A Comprehensive Guide – Number Analytics, accessed July 30, 2025, https://www.numberanalytics.com/blog/ultimate-guide-biosimilars-clinical-trials
- Assessment of Availability, Clinical Testing, and US Food and Drug Administration Review of Biosimilar Biologic Products – PubMed Central, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7536628/
- Industry Information and Guidance – FDA, accessed July 30, 2025, https://www.fda.gov/drugs/biosimilars/industry-information-and-guidance
- Scientific Considerations in Demonstrating Biosimilarity to a Reference Product – FDA, accessed July 30, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/scientific-considerations-demonstrating-biosimilarity-reference-product
- Biosimilar Product Development Guidance; Establishment of a Public Docket; Request for Information and Comments – Regulations.gov, accessed July 30, 2025, https://www.regulations.gov/document/FDA-2024-N-3228-0001
- Life Finds A Way: The FDA Releases Draft Guidance for Labeling and Advertising Biological and Biosimilar Products | Crowell & Moring LLP, accessed July 30, 2025, https://www.crowell.com/en/insights/client-alerts/life-finds-a-way-the-fda-releases-draft-guidance-for-labeling-and-advertising-biological-and-biosimilar-products
- Labeling for Biosimilar and Interchangeable Biosimilar Products September 2023 – FDA, accessed July 30, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/labeling-biosimilar-and-interchangeable-biosimilar-products
- The Economics of Biosimilars – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4031732/
- The Economic Impact of Biosimilars, accessed July 30, 2025, https://www.centerforbiosimilars.com/view/the-economic-impact-of-biosimilars
- Biosimilars Drug Market Isn’t Broken After All, USC Schaeffer Study Finds – June 6, 2023, accessed July 30, 2025, https://schaeffer.usc.edu/research/biosimilars-drug-market-isnt-broken-after-all/
- US commercial plans increase choice of biosimilar and originator products; market net prices decrease – Center for the Evaluation of Value and Risk in Health, accessed July 30, 2025, https://cevr.tuftsmedicalcenter.org/publications/us-commercial-plans-increase-choice-of-biosimilar-and-originator-products-market-net-prices-decrease
- Biosimilars: From Production to Patient – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10786443/
- (PDF) DIFFERENCES IN BIOSIMILARS APPROVAL BETWEEN THE USA AND EUROPEAN UNION – ResearchGate, accessed July 30, 2025, https://www.researchgate.net/publication/358271622_DIFFERENCES_IN_BIOSIMILARS_APPROVAL_BETWEEN_THE_USA_AND_EUROPEAN_UNION
- Combating Barriers to Biosimilar Use – U.S. Pharmacist, accessed July 30, 2025, https://www.uspharmacist.com/article/combating-barriers-to-biosimilar-use
- Implementation Strategies of Biosimilars in Healthcare Systems: The Path Forward, accessed July 30, 2025, https://www.ahdbonline.com/issues/2022/june-2022-vol-15-no-2/implementation-strategies-of-biosimilars-in-healthcare-systems-the-path-forward
- Comparison of Biosimilar Reimbursement Policies in the US and Select European Markets – ISPOR, accessed July 30, 2025, https://www.ispor.org/docs/default-source/intl2024/ispor24stylianouhpr20poster139394-pdf.pdf?sfvrsn=634b990_0
- REALIZING THE BENEFITS OF BIOSIMILARS: What the U.S. Can Learn from Europe, accessed July 30, 2025, https://healthpolicy.duke.edu/publications/realizing-benefits-biosimilars-what-us-can-learn-europe
- The Biosimilar Revolution: Assessing the European Union’s Approach to Biosimilarity, Interchangeability, Patient Access, and Its Market Analysis – PubMed Central, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11438530/
- Innovative Formulation Strategies for Biosimilars: Trends Focused on Buffer-Free Systems, Safety, Regulatory Alignment, and Intellectual Property Challenges – PMC – PubMed Central, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12196224/
- A Study of the Real-world Use of an Adalimumab Biosimilar and Evaluation of Nutritional Status on the Therapeutic Response | ClinicalTrials.gov, accessed July 30, 2025, https://clinicaltrials.gov/study/NCT05051943
- Uptake of Biosimilar Infliximab in the UK, France, Japan, and Korea: Budget Savings or Market Expansion Across Countries? – Frontiers, accessed July 30, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00970/full
- Addressing supply chain challenges for biosimilar products – DrugPatentWatch, accessed July 30, 2025, https://www.drugpatentwatch.com/blog/addressing-supply-chain-challenges-for-biosimilar-products/
- Adalimumab, Etanercept Biosimilars Deliver Real-World Results for Juvenile Idiopathic Arthritis – American Journal of Managed Care, accessed July 30, 2025, https://www.ajmc.com/view/adalimumab-etanercept-biosimilars-deliver-real-world-results-for-juvenile-idiopathic-arthritis
- AB1501 SAFETY AND EFFECTIVENESS OF ETANERCEPT BIOSIMILAR LBEC0101 FOR RHEUMATIC DISEASES IN SOUTH KOREA: REAL-WORLD POST-MARKETING SURVEILLANCE DATA, accessed July 30, 2025, https://ard.bmj.com/content/83/Suppl_1/2120.1
- Strategies for Overcoming Barriers to Adopting Biosimilars and Achieving Goals of the Biologics Price Competition and Innovation Act: A Survey of Managed Care and Specialty Pharmacy Professionals – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10397695/
- A Multistakeholder Consensus on Challenges and Solutions to the Adoption of Biosimilars, accessed July 30, 2025, https://www.ahdbonline.com/supplements/2525-a-multistakeholder-consensus-on-challenges-and-solutions-to-the-adoption-of-biosimilars
- Top 5 Challenges Faced By Biosimilars: Navigating the Complex Landscape, accessed July 30, 2025, https://www.drugpatentwatch.com/blog/top-5-challenges-faced-biosimilars/
- Overcoming barriers to biosimilar adoption: real-world perspectives from a national payer and provider initiative, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10391006/
- Prescriber Perspectives on Biosimilar Adoption and Potential Role of Clinical Pharmacology: A Workshop Summary – PMC, accessed July 30, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10099086/