Part I: The Diagnosis – Why the Old Playbook is Obsolete
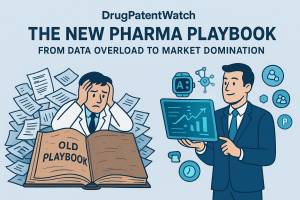
The pharmaceutical industry stands at a pivotal juncture. The commercial model that defined decades of success—a predictable and highly profitable engine built on blockbuster drugs, extended patent exclusivity, and vast field sales forces—is not merely aging; it is systemically failing. Companies that continue to operate from this legacy playbook, treating the profound structural shifts in the market as temporary headwinds, will find themselves unable to compete in a world that demands precision, personalization, and demonstrable value.1 The future of market leadership will be determined not by the scale of a company’s sales force or the volume of its advertising, but by the sophistication of its data intelligence and its ability to build new commercial models from the ground up. This analysis serves as a comprehensive guide to this new landscape, beginning with a clear-eyed diagnosis of why the old ways are no longer sufficient and quantifying the existential threats that mandate a fundamental transformation.
Section 1.1: The End of an Era: Deconstructing the Failures of the Blockbuster-Centric Commercial Model
For generations, the pharmaceutical commercial model was a masterclass in value capture. It was predicated on the development of “blockbuster” drugs—typically small-molecule treatments for common, mass-market conditions—which were protected by long periods of patent-enforced market exclusivity.1 This exclusivity allowed for premium pricing, generating revenues that funded not only shareholder returns but also the high-risk research and development (R&D) for the next generation of medicines. This economic engine was supported by armies of in-person sales representatives whose primary function was to build relationships with physicians and ensure brand awareness and preference.1
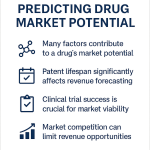
Today, every pillar of this model is crumbling. While blockbuster drugs, defined as those with over $1 billion in annual sales, still account for more than 80% of gross revenue for the average large-cap pharmaceutical company, the pathway to achieving this status has been irrevocably altered.1 The classic blockbuster, treating a widespread condition like hypertension or high cholesterol, faces immense resistance from payers who are under relentless pressure to control healthcare costs. These payers are increasingly unwilling to grant premium formulary access to new drugs that offer only marginal improvements over existing, often generic, therapies.1
Consequently, the new path to blockbuster status lies not in the mass market, but in high-value specialty therapies. These treatments target smaller, more precisely defined patient populations in complex fields like oncology, rare diseases, and immunology.1 This shift from a “one-size-fits-all” to a “nichebuster” approach demands a fundamentally different commercial strategy. A massive sales force is inefficient for reaching a dispersed group of specialists, and mass-media advertising is irrelevant for a drug treating a rare genetic disorder. This new paradigm requires a deep, data-driven understanding of the patient journey, the diagnostic process, and the specific clinical needs of a highly targeted physician audience.
This strategic reorientation also exposes a core historical vulnerability of the traditional model: its profound lack of genuine patient centricity. The industry’s historical focus was manufacturer-centric, prioritizing revenue generation, market dominance, and regulatory compliance above all else.3 Marketing strategies were aggressive and aimed primarily at influencing physician prescribing habits, with the patient’s perspective often being a secondary or tertiary consideration, filtered through the lens of healthcare providers (HCPs) and insurers.3 This approach is no longer tenable in an era where patients are empowered with information and demand a more active role in their healthcare decisions.1
Section 1.2: Confronting the $300 Billion Cliff: The Unprecedented Financial Threat of Patent Expirations
The most immediate and quantifiable threat forcing the industry’s hand is the looming patent cliff. A drug patent typically provides 20 years of protection from the filing date, but due to the lengthy R&D and regulatory approval process, the effective period of market exclusivity is often much shorter.1 The expiration of this exclusivity, known as Loss of Exclusivity (LOE), triggers a catastrophic and rapid decline in revenue as lower-priced generic or biosimilar competitors flood the market.
The scale of the current patent cliff is without precedent. Projections indicate that patent expirations will put approximately $300 billion in annual global revenue at risk through 2030, with a staggering $200 billion of that exposure occurring in the next five years alone.1 Other analyses reinforce this dire forecast, estimating that
$236 billion in revenue is at risk between 2025 and 2030, and over $400 billion by 2033 as patents on top-selling drugs like Keytruda and Eliquis expire.6
The velocity of this revenue erosion is just as alarming as its scale. Upon the entry of the first generic competitor, a brand-name small-molecule drug can lose 80% to 90% of its market share within the first year.1 This precipitous financial event, which can erase billions in revenue almost overnight, creates immense pressure on a company’s stock price and its ability to fund future innovation.9 It transforms the effectiveness of a drug’s launch and marketing strategy during its protected years into a matter of existential importance; every dollar of revenue must be maximized before the cliff arrives.1
This intense financial pressure is a primary catalyst reshaping the industry’s structure. It forces companies into a frantic race to innovate and acquire new assets to offset the inevitable losses. According to a 2025 outlook from Deloitte, this looming patent expiration is a key driver of heightened interest in mergers and acquisitions (M&A), with 77% of surveyed executives expecting M&A activity to increase.10 The patent cliff is not merely a line item on a financial statement; it is a force of nature compelling a strategic evolution. The sheer magnitude of the revenue at risk makes the inefficiencies of the old mass-market commercial model untenable. Companies can no longer afford the high cost and low precision of blanketing the market with sales reps and advertising. They are being forced by economic necessity to adopt more efficient and effective commercial models that promise a higher return on investment (ROI) through data-driven precision and a focus on demonstrable value.11
Section 1.3: The New Power Brokers: How Empowered Patients and Overwhelmed Physicians are Forcing a Paradigm Shift
Concurrent with the industry’s internal financial pressures, a profound power shift is occurring among its key external stakeholders. Both patients and physicians are demanding a new mode of engagement, rendering the traditional, top-down communication model obsolete.
Today’s patients are no longer passive recipients of care. Fueled by unprecedented access to information and a proliferation of digital health tools, they have become active, informed participants in their own health journeys.1 They are increasingly acting as the “CEOs of their health,” demanding more control over their healthcare decisions and expecting the same kind of seamless, personalized, and transparent digital experiences from healthcare that they receive in every other aspect of their lives.3 This evolution from passive patient to empowered health consumer requires a fundamental rewiring of pharmaceutical marketing, moving away from a focus on the physician as the sole decision-maker to a model that engages, supports, and empowers the end user of the medicine.3
At the same time, the industry’s traditional target—the physician—is facing a crisis of their own. HCPs are severely time-constrained and suffering from information overload, inundated with a constant stream of new clinical data, treatment guidelines, and pharmaceutical promotions.1 The classic model of in-person sales rep “detailing” is rapidly losing its effectiveness. An unsolicited visit from a sales representative is often seen as a disruption rather than a service. HCPs now require information to be delivered with surgical precision and relevance, integrated seamlessly into their clinical workflow at the moments it is most valuable—such as during treatment planning or when reviewing new trial data.16 The focus must shift from
how often a brand can reach an HCP to how meaningful and valuable each interaction is.16
This new reality has created a critical disconnect between pharmaceutical companies and their most important customers. A revealing Deloitte survey found that while over 80% of pharma executives expressed satisfaction with their current customer engagement strategy, only about one-third of HCPs reported that a pharmaceutical company’s customer-facing resources actually meet their needs.13 This chasm between the industry’s perception and the customer’s reality represents both a significant threat to incumbents and a massive opportunity for companies that can successfully bridge the gap with a more intelligent, responsive, and value-driven approach.
| Attribute | Traditional Model (The Past) | New Playbook (The Future) |
| Key Data Source | Clinical Trial Data (Phase III) 1 | Real-World Data (RWD), Patient-Generated Health Data (PGHD) 1 |
| Success Metric | Total Prescriptions (TRx), Sales Volume 1 | Patient Outcomes, Demonstrable Value, Adherence 1 |
| Dominant Channel | In-Person Sales Rep Detailing 1 | Optichannel Digital Engagement, Tele-detailing 11 |
| Marketing Approach | Mass Marketing, Brand Awareness 1 | Hyper-Personalization, Precision Targeting 1 |
| Economic Model | Fee-for-Service (Payment per Pill) 12 | Value-Based (Payment for Outcomes) 1 |
| Stakeholder Focus | Physician-Centric 3 | Patient-Centric, Ecosystem-wide 3 |
| IP Strategy Focus | Defensive Shield, Legal Necessity 18 | Offensive Commercial Weapon, Strategic Asset 18 |
Part II: The New Fuel & Engine – Powering the Modern Pharma Enterprise
The transformation of the pharmaceutical commercial model is being powered by two interconnected forces: an exponential increase in the volume and variety of health data, and the maturation of artificial intelligence (AI) capable of turning that data into a strategic asset. This section explores this new data ecosystem—the “fuel”—and the advanced analytical capabilities—the “engine”—that together form the foundation of the modern, intelligence-driven pharmaceutical enterprise. Mastering these elements is no longer a competitive advantage; it is a prerequisite for survival and success in the coming decade.
Section 2.1: Beyond the Clinical Trial: Harnessing the Power of Real-World Data (RWD) and Patient-Generated Health Data (PGHD)
For decades, the gold standard of evidence in pharmaceuticals was the data generated within the tightly controlled environment of a Randomized Controlled Trial (RCT). While essential for regulatory approval, RCT data provides a limited and often incomplete picture of how a drug performs in the complexities of the real world.1 The new playbook is fueled by a much richer and more diverse ecosystem of data that extends far beyond the clinical trial.
The new fuel for growth is the explosion of data from sources like Electronic Health Records (EHRs), insurance claims databases, wearable devices, and genomic sequencing.1 This torrent of information is broadly categorized into two critical types:
- Real-World Data (RWD): This refers to data relating to patient health status and/or the delivery of health care routinely collected from a variety of sources. RWD is transformed into Real-World Evidence (RWE) through analysis. For pharmaceutical companies, RWE is revolutionizing both R&D and commercial functions. In R&D, it can be used to design more efficient trials and support regulatory submissions. For market access teams, RWE provides the crucial evidence needed to demonstrate a new drug’s value and cost-effectiveness to payers, answering their fundamental question: “How will this drug perform in our specific member population?”.1
- Patient-Generated Health Data (PGHD): This includes data created, recorded, or gathered by or from patients (or family members or other caregivers) to help address a health concern. It encompasses information from sources like wearable fitness trackers, home monitoring devices, and patient-reported outcome surveys. PGHD provides an unprecedented, direct line of sight into the patient’s daily life, offering invaluable insights into treatment adherence, quality of life, and the real-world challenges patients face in managing their condition.1
This expansion of the data universe does not render clinical trial data obsolete; rather, it reimagines its utility. Progressive organizations now view their clinical trials as the first source of rich commercial intelligence. By analyzing trial data through a commercial lens from the outset, marketing teams can identify which subgroups of patients responded best to the treatment, uncover the key decision points in the clinician and patient journey, and begin building the foundational value proposition long before the drug is launched.1
Section 2.2: The Intelligence Engine: Activating Data with AI, Machine Learning, and Predictive Analytics
If RWD and PGHD are the raw fuel, then artificial intelligence and advanced analytics are the high-performance engine that converts that fuel into strategic horsepower. The sheer volume and complexity of modern health data are beyond the capacity of human analysis alone. AI and machine learning (ML) provide the essential technological layer to process this data overload, identify hidden patterns, and generate the actionable insights that drive the new commercial models.1
The strategic importance of this intelligence engine is reflected in the market’s trajectory. The market for AI in healthcare marketing is projected to grow to a staggering $187.95 billion by 2030, and a survey by Invoca found that 93% of marketers are already leveraging AI-powered strategies.16 This is not a future trend; it is a present-day reality. The value AI can unlock for the pharmaceutical industry is immense, with a McKinsey Global Institute report estimating that generative AI alone could produce
$60 to $100 billion in value, with commercial applications accounting for the largest share of that opportunity ($18 to $30 billion).20
The applications of this intelligence engine span the entire commercialization lifecycle:
- Hyper-Personalization and Precision Engagement: AI algorithms can analyze vast, anonymized datasets to understand HCP prescribing patterns, specialties, and clinical workflows. This allows marketing content to be adapted and delivered through the most effective channel at the precise moment it is most valuable to the clinician, transforming marketing from a broadcast medium into a personalized decision-support service.16
- Predictive Analytics for Market Forecasting: By synthesizing disparate data sources—from prescribing patterns and payer data to market trends—predictive analytics can anticipate shifts in the market. This enables commercial teams to stay ahead of changes in prescribing behavior, proactively allocate resources, and refine their strategies rather than simply reacting to past events.15
- Content Optimization and Generation: Generative AI is rapidly becoming a powerful tool for marketing teams. It can analyze past successful campaigns and market trends to generate initial creative concepts for testing.21 While fully AI-generated promotional content remains inadvisable in a highly regulated industry, “augmented content creation”—where AI supports human creativity—is already delivering significant value by helping to scale content production and repurpose it for different channels and audiences.20
- Streamlining Compliance and Medical-Legal Review (MLR): One of the most significant operational bottlenecks in pharma marketing is the painstaking MLR process. AI is being deployed to streamline these reviews by automatically flagging potential compliance risks, comparing new content against established rules, and accelerating a process that has historically been a major source of frustration and delay.20
Section 2.3: Quantifying the Impact: The Proven ROI of Data-Driven Precision Marketing in Pharma
For executive leadership, the critical question is whether the significant investment required to build this data and analytics infrastructure delivers a tangible return. The evidence overwhelmingly indicates that it does, both in terms of direct financial ROI and long-term strategic value.
Data-driven precision marketing allows for a more efficient allocation of resources, shifting spend away from low-performing tactics toward those with a measurable impact. A clear example of this can be seen in the ROI of different physician engagement channels. One analysis found that the ROI for e-detailing was $2.48 for every dollar spent. This figure significantly outperformed the ROI for traditional in-person detailing ($1.72) and direct-to-consumer (DTC) advertising ($1.68).11 This type of direct comparison provides a clear, data-backed rationale for reallocating marketing budgets toward more precise and efficient digital channels.
The broader business impact is even more compelling. A report from McKinsey states that organizations that leverage data-driven strategies are 23 times more likely to acquire customers and six times more likely to retain them compared to their less data-savvy peers.23 In an industry where building and maintaining relationships with both HCPs and patients is paramount, this represents a profound competitive advantage.
However, a sophisticated understanding of ROI in the modern pharmaceutical context requires moving beyond a simple formula of (Revenue – Cost) ÷ Cost.11 While a short-term ROI of 2:1 or 3:1 on incremental revenue may be a solid benchmark, a truly effective strategy must also account for long-term value creation. This means supplementing financial metrics with measures of brand health, such as physician awareness, prescriber trust, and patient sentiment.11 The ultimate goal of a data-driven system is to achieve closed-loop marketing, where it is possible to connect specific marketing touchpoints directly to changes in HCP prescribing behavior. This is accomplished through National Provider Identifier (NPI)-level attribution, which tracks which HCPs saw a message, how they engaged with it, and whether their prescribing patterns subsequently changed.11 This level of granularity transforms marketing from a perceived cost center into a measurable driver of business outcomes.
The pragmatic and cautious adoption of AI in pharmaceutical marketing reveals a critical reality about this transformation. While the technology’s potential is vast, its successful implementation is less about having the most sophisticated algorithm and more about addressing fundamental organizational challenges. The primary hurdles are not technological but cultural and structural. Success hinges on ensuring high-quality, accessible data, which requires breaking down the internal silos that have historically fragmented information across commercial, medical, and R&D functions.16 It demands the establishment of robust data governance frameworks to navigate complex privacy regulations like HIPAA and GDPR.16 Ultimately, it requires fostering a corporate culture that embraces “safe experimentation” and invests in upskilling cross-functional teams to understand both AI’s capabilities and its compliance requirements.21 The technology is often ahead of the organization’s ability to absorb it, making strategic change management—not just technological investment—the true determinant of success in unlocking AI’s immense value.
Part III: The New Blueprints – Strategies for Market Leadership
Building upon the foundation of data and AI, the pharmaceutical industry is developing new commercial blueprints designed for the modern healthcare ecosystem. These are not merely updated tactics but fundamental shifts in how value is created, communicated, and compensated. This section details the three core strategic models that will define market leadership: the patient-centric imperative, the shift to value-based contracting, and the execution of hyper-personalization at scale. These blueprints are not independent strategies; they form a deeply interconnected and mutually reinforcing system.
Section 3.1: Blueprint 1: The Patient-Centric Imperative
Patient-centricity has evolved from a well-intentioned aspiration into a core business imperative. It is a comprehensive framework that reorients the entire pharmaceutical value chain around the needs, preferences, and experiences of the patient.3 This goes far beyond creating patient-friendly marketing materials. It involves systematically understanding and addressing patients’ non-medical challenges (e.g., food insecurity for a diabetic patient), designing support services and clinical trials that align with their values and goals, and fostering an environment of collaboration and shared decision-making between patients and their providers.3
The transition to this model is being driven by a confluence of powerful forces. As noted previously, patients are demanding more control over their healthcare, a trend that pharma companies must adapt to in order to remain relevant.3 Regulatory agencies like the FDA are increasingly mandating patient-focused drug development initiatives to ensure that new therapies address outcomes that truly matter to patients.3 Furthermore, persistent challenges in clinical trials, such as high dropout rates, and low medication adherence in the real world (often as low as 50% in developed countries) underscore the urgent need for approaches that actively engage and support patients throughout their journey.3
Case Study in Focus: Scaling Patient Support for Zepbound’s Blockbuster Launch
A powerful illustration of patient-centricity in action is the operational response to the launch of the weight-loss drug Zepbound. The product’s rapid market uptake led to a surge in patient inquiries across phone, email, and chat channels, overwhelming the company’s existing support provider.25 This created long wait times and dropped chats, jeopardizing the patient experience at a critical moment in the brand’s lifecycle. Recognizing that a positive support experience is integral to patient success and brand loyalty, the company partnered with Emerge Growth to pilot a new, fully managed, and scalable BPO solution.
The solution involved the rapid deployment of a dedicated team of 15 Patient Care Representatives (PCRs) in under 30 days, trained to meet rigorous compliance and service standards. The success of the pilot was immediate and profound. Within six months, the team grew from 15 to over 100 PCRs, all managed by the BPO partner. This allowed the pharmaceutical company to seamlessly handle the immense volume of patient inquiries, improve satisfaction, and reduce the burden on its internal teams. The Zepbound case demonstrates that in the new commercial model, operational excellence in patient support is not a back-office function but a strategic pillar of a successful blockbuster launch.25
Case Study in Focus: Patient-Centric Sampling (PCS) in Clinical Trials
The patient-centric imperative is also reshaping the earliest stages of drug development. The traditional model of clinical trials, which often requires patients to travel to clinical sites for frequent venous blood draws, can be a significant burden, limiting recruitment and diversity.26 Patient-centric sampling (PCS) represents a paradigm shift, utilizing technological advancements in microsampling to allow for remote, at-home sample collection.26
A review of seven case studies implementing PCS highlights its clear advantages. By prioritizing patient convenience and engagement, PCS strategies have been shown to improve trial recruitment, increase participant diversity, minimize patient discomfort, and enhance overall operational efficiency.26 In one early-phase asthma trial, the use of PCS was instrumental in enhancing the study’s design. These examples show that embedding patient-centric principles deep within the R&D process not only improves the patient experience but also leads to better, more efficient science.26
Section 3.2: Blueprint 2: The Shift to Value-Based Contracting (VBCs)
Perhaps the most profound economic shift in the new playbook is the move away from the traditional fee-for-service model—where payment is made for every pill sold, regardless of its effectiveness—to value-based contracts (VBCs). Also known as risk-sharing or outcomes-based agreements, VBCs are innovative payment models that directly link a drug’s reimbursement level to its performance in a real-world patient population.1
This model creates a more rational and sustainable healthcare system by aligning the incentives of all major stakeholders.
- For Payers: VBCs offer a powerful tool to manage financial risk and ensure they are not paying for ineffective treatments. It reduces uncertainty regarding a new drug’s clinical value and financial impact by tying payment directly to proven performance.27
- For Manufacturers: In an increasingly crowded and competitive market, VBCs allow innovative companies to differentiate their products by demonstrating confidence in their real-world effectiveness. This can be a crucial strategy for securing market access and preferred formulary placement.27
- For Patients: VBCs can help provide earlier and broader access to new medicines, particularly for treatments with limited initial clinical data or those serving small patient populations. They provide an alternative to closed formularies, where a drug might otherwise be unavailable.27
A Deep Dive into VBC Models
While the specific terms of VBCs are often confidential, several common structures have emerged, each designed to address different clinical and financial scenarios:
- Outcomes-Based Rebates: This is one of the most common models. The manufacturer agrees to provide the payer with a rebate if the drug fails to meet pre-agreed clinical or cost-effectiveness metrics (e.g., a certain percentage of patients achieving a target biomarker level).1
- Indication-Specific Pricing: For drugs approved for multiple diseases or conditions, this model allows for different prices to be set for each FDA-approved indication, reflecting the drug’s varying levels of effectiveness and value in each context.1
- Shared Savings: In this model, the manufacturer and payer agree to share in the net cost savings if the use of the drug leads to a reduction in total healthcare costs. For example, if a new heart failure medication significantly reduces expensive hospital admissions, the manufacturer would receive a portion of those savings.1
- Cost/Utilization Cap: The manufacturer agrees to cover the costs of therapy that extend beyond a certain total cost or duration per patient. This model is particularly relevant for high-cost therapies for chronic conditions, providing the payer with budget predictability.1
Navigating the Hurdles
Despite their compelling logic, the broader implementation of VBCs in the U.S. has been slow due to significant operational, regulatory, and structural barriers.
- Administrative and Data Burden: VBCs are complex and resource-intensive to design and manage. They require robust data infrastructure to collect, integrate, and analyze outcomes data, often from multiple, disparate sources. This administrative burden can be substantial, and there are few economies of scale, as each contract is often unique.27
- Regulatory Barriers: The current regulatory environment presents significant hurdles. Policies like the Medicaid Best Price rule (which requires manufacturers to offer Medicaid the lowest price available to any commercial payer) and the federal Anti-Kickback Statute can create unintended consequences that make manufacturers and payers hesitant to enter into innovative risk-sharing arrangements.27
- Misaligned Incentives and Data Silos: A fundamental challenge is the structural separation of medical and pharmacy benefits in the U.S. healthcare system. A drug paid for under the pharmacy benefit may generate savings (e.g., avoided surgeries) that accrue to the medical benefit. If these benefits are managed by different entities, or even different departments within the same entity, it becomes incredibly difficult to track outcomes and attribute savings appropriately.28 Furthermore, powerful intermediaries like Pharmacy Benefit Managers (PBMs) may have less incentive to adopt complex VBCs when they can rely on more predictable revenue from traditional, volume-based rebate contracts.28
| VBC Model Type | Mechanism | Best Suited For… | Key Implementation Challenge |
| Outcomes-Based Rebate | Manufacturer provides a rebate if pre-agreed clinical or cost-effectiveness metrics are not met.1 | Drugs with clear, easily measurable, and short-term clinical endpoints (e.g., cholesterol levels, viral load).28 | Defining and agreeing upon feasible outcome measures; data collection and tracking burden.27 |
| Indication-Specific Pricing | A single drug is priced differently for different FDA-approved indications based on varying effectiveness.1 | Oncology or immunology drugs with multiple approvals where value differs significantly by indication (e.g., higher price for first-line cancer vs. later lines).30 | Operational complexity for payers and providers to track and bill based on indication; potential for off-label use to complicate pricing.1 |
| Shared Savings | Manufacturer shares in the net cost savings if the drug leads to a reduction in total healthcare costs (e.g., fewer hospitalizations).1 | Drugs for chronic conditions like heart failure or COPD, where the primary value is avoiding costly acute events.31 | Difficulty in attributing cost savings solely to the drug versus other interventions; misalignment between pharmacy and medical benefits.28 |
| Cost/Utilization Cap | Manufacturer covers costs that go beyond a certain total cost or duration of therapy per patient.1 | High-cost curative therapies (e.g., gene therapies) or treatments for chronic conditions with unpredictable duration or cost.32 | Accurately forecasting utilization and setting appropriate caps; managing the financial risk for the manufacturer.1 |
Section 3.3: Blueprint 3: Hyper-Personalization at Scale
The third blueprint, hyper-personalization, is the tactical execution layer that brings the new commercial model to life. It leverages the data and AI engine described in Part II to move away from the inefficient paradigm of mass reach and toward a new era of precision engagement with both HCPs and patients.1
The Rise of Optichannel
For years, “omnichannel” has been a dominant buzzword in pharma marketing. However, in practice, its execution is often “messy” and falls short of its promise.17 Many omnichannel strategies devolve into simply being present on multiple channels, leading to fragmented customer journeys and diminishing returns.11 This requires breaking down the deep-seated organizational silos that separate brand, digital, medical, and sales teams to create a single, consistent view of the customer.17
The more sophisticated evolution of this concept is optichannel. This approach is not about using all channels, but about using data and analytics to select the optimal channel for a specific HCP, for a specific message, at a specific point in their workflow.11 This dynamic tailoring of communication delivers personalized, cost-effective engagement and drives smarter ROI by concentrating resources where they will have the greatest impact.11
Crafting Precision Engagement
True hyper-personalization goes far beyond adding a doctor’s name to an email subject line. It involves using AI to analyze rich, first-party data on HCPs’ clinical interests, prescribing behaviors, and channel preferences to deliver information that is genuinely useful and relevant.16 This means shifting the entire marketing mindset from a focus on message frequency (“how often can we reach them?”) to a focus on interaction quality (“how can we make this next interaction meaningful?”).16
For an HCP, this could mean receiving a concise summary of new clinical data relevant to their specific patient population just before they begin treatment planning. For a patient, it could mean receiving a supportive text message reminding them to take their medication, linked to an educational resource about managing side effects. Each interaction is data-driven, contextually aware, and designed to add value rather than simply promote a brand.
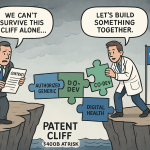
The successful implementation of these three blueprints reveals a critical strategic connection: they are not independent options but an interdependent, reinforcing system. Value-Based Contracts, for instance, are entirely dependent on the ability to prove real-world outcomes.1 This proof requires the collection and analysis of high-quality RWD and PGHD, which can only be gathered effectively through a Patient-Centric model that engages and supports patients throughout their treatment journey.1 Driving the necessary patient adherence and physician engagement to collect this data and achieve positive outcomes, in turn, requires Hyper-Personalized communication that is timely, relevant, and delivered through the optimal channel.11 In this new ecosystem, hyper-personalization enables patient-centricity, which generates the data and adherence needed to make value-based models viable. They are three legs of the same stool; attempting to implement one in isolation will inevitably lead to instability and failure.
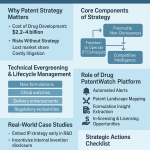
Part IV: The Cornerstone of Value – Mastering Intellectual Property Strategy
While data, AI, and new commercial models are transforming how pharmaceutical companies operate, the fundamental source of value in the industry remains unchanged: the period of market exclusivity granted by a patent. Intellectual property (IP) is not a peripheral legal function; it is the central economic engine that makes the entire high-risk, high-cost model of drug development possible.18 This section elevates the discussion by reframing patent strategy from a defensive necessity into a core commercial weapon, detailing the sophisticated tactics used to maximize exclusivity and analyzing the central role of patent intelligence and litigation in shaping market dynamics.
Section 4.1: The Patent as a Commercial Weapon, Not Just a Legal Shield
It is impossible to overstate the foundational role of patents in the pharmaceutical ecosystem. The average cost to develop a new drug now exceeds $2 billion, a process that can take over a decade from initial discovery to regulatory approval.8 The patent provides the inventor with a temporary monopoly, a period of market exclusivity during which the company can price the drug to recoup this massive investment and fund future R&D.5 Without this protection, the economic model collapses.33
Consequently, a comprehensive drug patent strategy is not merely a defensive legal shield but a central pillar of offensive corporate strategy.18 It must be woven into the fabric of the business from the earliest stages of development, influencing which drug candidates are pursued, how clinical trials are designed, and how global commercialization is planned.18 The patent portfolio is the company’s most valuable commercial asset, and its strategic management is a primary driver of long-term market dominance.
Section 4.2: The Art of the Patent Thicket: Extending Exclusivity and Deterring Competition
The most sophisticated and controversial application of offensive patent strategy is the creation of a “patent thicket.” This involves shielding a single drug with a dense, multi-layered, and overlapping portfolio of patents that extends far beyond the initial “composition of matter” patent covering the active molecule.9 This web of
secondary patents is meticulously constructed to protect every conceivable aspect of the drug, including:
- New Formulations: Such as extended-release versions that offer more convenient dosing.35
- Methods of Use: Protecting the use of the drug to treat new diseases or specific patient subpopulations, a practice that forms the legal basis for drug repurposing.18
- Manufacturing Processes: Covering novel and non-obvious methods of producing the drug.35
- Other Variations: Including patents on specific crystalline structures (polymorphs), delivery devices, or combinations with other drugs.9
The strategic objective of the patent thicket is not necessarily to win every potential court battle over every single patent. Instead, it is to create such a formidable and complex legal barrier that the prospect of litigation becomes prohibitively daunting and expensive for generic and biosimilar competitors. This legal fortress can effectively deter challenges or force competitors into settlement agreements that are highly favorable to the brand manufacturer, delaying the onset of competition for years.9
Definitive Case Study: How AbbVie’s Humira Strategy Rewrote the Rules of Monopoly Extension
The most definitive and well-documented example of a patent thicket strategy is AbbVie’s defense of its blockbuster anti-inflammatory drug, Humira. An analysis of this strategy reveals its scale, its jurisdictional specificity, its profound financial impact, and the intense legal and ethical debates it has ignited.
- The Scale of the Thicket: AbbVie constructed an unprecedented fortress around Humira, filing 247 patent applications in the United States alone. This strategy was explicitly aimed at delaying biosimilar competition for a total of 39 years from the first patent filing.34 Critically, a staggering
89% of these patent applications were filed after Humira was already approved and on the market, with nearly half filed more than a decade after its launch.36 - The U.S. vs. Europe Discrepancy: The Humira case powerfully illustrates that the patent thicket is largely an American phenomenon, enabled by the specific rules of the U.S. patent system. A comparative analysis found that while Humira’s U.S. portfolio consisted of roughly 73 core granted patents, approximately 80% of them were non-patentably distinct (duplicative) from one another, a practice permitted through the use of “terminal disclaimers”.37 In stark contrast, Humira’s European patent portfolio was dramatically smaller, comprising only
eight non-duplicative patents.37 This discrepancy in patenting strategy directly led to biosimilars entering the European market in 2018, nearly five years before their U.S. launch in 2023.36 - The Financial Impact: The success of AbbVie’s strategy in delaying U.S. competition was immensely profitable. Before the entry of biosimilars, the Humira franchise was generating revenue of $47.5 million per day.34 The extended monopoly in the U.S. is estimated to have added billions in excess costs to the American healthcare system.36
- The Legal and Ethical Debate: AbbVie’s strategy, while ultimately successful in court, has been at the center of a fierce debate. The company faced antitrust lawsuits alleging that its patent thicket constituted illegal monopolization, though the courts ultimately ruled that its actions were protected petitioning activities.38 This has fueled a broader societal discussion about “evergreening”—the fine line between protecting legitimate, incremental innovation that benefits patients (e.g., a safer formulation) and deploying patents on trivial modifications purely to block competition and exploit the legal system.39 While proponents argue it is a necessary incentive for continued research, critics contend it is an abuse of the patent system that prioritizes profits over public health.40
| Metric | United States | European Union |
| Total Patent Applications Filed | 247 36 | 76 36 |
| Core Granted Patents (Product/Formulation) | ~73 37 | 8 37 |
| Number of Distinct Inventions | 14 37 | 8 37 |
| Percentage of Duplicative Patents | ~80% 37 | 0% 37 |
| Year of First Biosimilar Entry | 2023 34 | 2018 36 |
| Estimated Additional Cost to Healthcare System | >$14.4 Billion 36 | N/A |
Section 4.3: Navigating the Battlefield: Understanding the Inevitable Role of Patent Litigation
Drug patent litigation is not an anomaly or a breakdown of the system; it is a core, intended feature of the legislative framework established by the Drug Price Competition and Patent Term Restoration Act of 1984, commonly known as the Hatch-Waxman Act.9 This landmark legislation created a “grand bargain” designed to balance the competing goals of incentivizing innovation and ensuring affordable access to medicines. The litigation it spawns is the adversarial process through which this balance is tested and the validity and scope of pharmaceutical patents are challenged.9
The framework creates powerful and opposing incentives for innovator and generic companies, placing them on a near-inevitable collision course.
- The Generic’s Gambit: The Hatch-Waxman Act provides a powerful prize for generic companies willing to challenge an innovator’s patents: a 180-day period of marketing exclusivity is awarded to the first generic applicant to file an Abbreviated New Drug Application (ANDA) containing a “Paragraph IV certification” (a legal assertion that the innovator’s patent is invalid, unenforceable, or will not be infringed by the generic product).9 This exclusivity period is immensely lucrative, as the first-to-file generic can capture substantial market share at a price well above what will prevail once multiple competitors enter. This dynamic effectively deputizes generic companies to act as private “sheriffs,” incentivized to scrutinize and challenge potentially weak or invalid patents that block competition.9
- The Innovator’s Imperative: For the innovator company, the financial stakes are astronomical. A disproportionate amount of a drug’s lifetime revenue is often generated in the final years of its patent-protected life.9 The entry of a generic competitor is an existential threat to this revenue stream. This reality drives innovators to adopt aggressive litigation strategies and deploy their patent thickets as a defensive fortress to delay generic entry for as long as possible. Due to the rigid legal timelines triggered by a Paragraph IV notice, innovator companies must operate in a state of almost perpetual litigation readiness.9
Section 4.4: Patent Intelligence: Transforming Patent Data into a Predictive, Actionable Asset
In this high-stakes environment, the proactive use of patent data as a strategic asset is a critical differentiator. Sophisticated companies no longer view patent information as the exclusive domain of their legal departments; they harness it as a source of predictive competitive intelligence to inform commercial strategy.
The foundational tool for this is Patent Landscape Analysis. This involves systematically searching and analyzing existing patents, applications, and scientific literature to create a comprehensive map of the IP terrain in a specific therapeutic area.18 This analysis serves several critical strategic functions:
- Identifying “White Space”: It reveals areas with limited patent coverage, highlighting opportunities for innovation where a company can establish a strong, defensible patent position with a lower risk of infringement.18
- Assessing Competitor Activity: It provides invaluable intelligence on which companies are active in a space, what technologies they are pursuing, and where their R&D efforts are focused, informing decisions on which drug candidates to prioritize.44
- Avoiding Infringement: It identifies existing patents that could block a company’s own development, allowing them to “design around” the patents or seek a license early in the process, before significant resources are committed.18
To execute this analysis effectively, companies increasingly rely on specialized competitive intelligence platforms. Services like DrugPatentWatch provide comprehensive databases and deep analytics on global drug patents, clinical trials, patent expiration dates, and ongoing litigation.1 This intelligence transforms IP from a reactive legal concern into a proactive marketing weapon. For example, knowing that a competitor’s key formulation patent is weak and likely to be challenged can inform a company’s long-term messaging, allowing them to position their own product’s unique features as a more durable advantage.46
Finally, a sophisticated IP strategy involves quantifying the Return on Investment (ROI) of the patent portfolio itself. This requires a comprehensive assessment that goes beyond simply tracking legal and maintenance costs. It involves estimating the revenue directly generated or protected by each patent, the cost savings from market exclusivity, the defensive value in deterring competitors, and the potential for revenue generation through strategic licensing opportunities.49 This data-driven approach allows companies to make informed decisions about which patents to maintain, which to license, and which to abandon, ensuring that resources are focused on the IP assets that create the most commercial value.
The aggressive patenting strategies exemplified by the Humira case, while designed to prolong the life of the traditional high-price, volume-based model, have created a powerful paradoxical effect. By extending monopolies and maintaining extraordinarily high prices for years beyond what many deem reasonable, these tactics have placed an unsustainable financial burden on the healthcare system.36 This immense cost pressure has, in turn, become a primary catalyst for payers and policymakers to seek alternatives. It has accelerated the very shift towards value-based models that challenge the paradigm these strategies were meant to protect.12 The industry’s most potent tool for preserving the past has, ironically, become a major force in hastening the arrival of the future.
Part V: The Roadmap to Transformation – Implementation and Future Outlook
The transition to a new commercial playbook is not merely a matter of adopting new technologies or strategies; it requires a profound transformation of organizational culture, capabilities, and ethical governance. This final section provides a forward-looking roadmap for implementation, addressing the critical ethical challenges of a data-driven world, the necessary organizational restructuring, and the key trends that will shape the pharmaceutical landscape through 2030.
Section 5.1: The Ethical Compass: Navigating the Moral Minefield of Data Privacy, Algorithmic Bias, and Patient Consent
As pharmaceutical companies harness the power of big data and AI, they also inherit a significant ethical responsibility. Building a successful and sustainable commercial model for the future requires not only technological sophistication but also a demonstrable commitment to ethical principles. Failure to navigate this moral minefield can result in a catastrophic loss of trust from patients, providers, and regulators, undermining the very foundation of the new playbook. The key ethical challenges fall into three interconnected domains 52:
- Respecting Autonomy and Consent: The use of large, aggregated datasets challenges traditional models of informed consent. Big Data research often relies on “broad consent,” where individuals agree to the use of their data for a wide range of future, unspecified research.52 This can leave patients unaware of how their information is being used, particularly when AI uncovers unexpected correlations. Furthermore, the use of de-identified data raises concerns about the potential for re-identification, especially with genetic information, meaning data thought to be anonymous may not be.52 Organizations must move toward more transparent and dynamic consent models that give patients greater control and understanding.
- Achieving Equity and Avoiding Bias: AI algorithms are only as unbiased as the data they are trained on. If an algorithm is trained on datasets that underrepresent certain racial, ethnic, or socioeconomic groups, its conclusions can perpetuate and even amplify existing healthcare disparities.52 A predictive model for disease risk, for example, might perform poorly for underrepresented populations, leading to inequitable care. This creates a moral and business imperative for companies to actively audit their datasets for bias and ensure their models are trained on representative populations.
- Protecting Privacy and Building Trust: In an age of big data, health information can take on “surveillance implications”.52 The potential for data to be used in ways that individuals did not anticipate—from marketing to employment decisions—erodes trust. To counteract this, companies must implement robust data governance frameworks, prioritize working with de-identified data wherever possible, and maintain transparency with all stakeholders about how data is being used and protected.21 The so-called “black box” problem of AI, where even developers cannot fully explain an algorithm’s decision-making process, necessitates a commitment to human review and clear lines of accountability for AI-assisted outputs.21
| Ethical Principle | Key Question for Your Organization | Mitigation Strategy |
| Autonomy & Consent | Is our consent process clear, specific, and dynamic, or does it rely on overly broad, one-time agreements? 52 | Implement layered, easy-to-understand consent notices. Explore dynamic consent platforms that allow individuals to manage their preferences over time. Prioritize patient education on data use.54 |
| Equity & Bias | Have we audited our datasets for demographic, socioeconomic, and geographic bias? How do we test our algorithms for disparate impacts on underrepresented populations? 52 | Invest in sourcing diverse and representative datasets. Establish cross-functional ethics committees to review algorithms before deployment. Implement continuous monitoring to detect and correct for algorithmic drift and bias.53 |
| Privacy & Security | What are our protocols for data de-identification, and how do we assess and mitigate the risk of re-identification? 52 | Work with de-identified data wherever possible. Implement robust data governance and security frameworks. Select technology vendors with healthcare-specific privacy expertise and certifications.21 |
| Transparency & Accountability | Can we explain the logic behind our key AI-driven decisions? Who is accountable if an algorithm produces a harmful or erroneous output? 21 | Document AI decision logic where possible. Implement mandatory human review processes for high-stakes AI outputs. Create clear accountability frameworks that assign responsibility for AI-assisted content and decisions.21 |
Section 5.2: Building the Organization of the Future: Breaking Down Silos and Cultivating New Capabilities
Executing the new playbook requires a fundamental redesign of the commercial organization itself. The legacy structure, characterized by rigid silos between functional areas, is incompatible with the demands of a data-driven, patient-centric world.
The creation of a seamless, personalized customer journey is impossible when brand, digital, medical, and sales teams operate from separate datasets and with conflicting objectives. The execution of a true optichannel strategy is often described as “messy” precisely because it requires breaking down these internal walls.17 Achieving this requires strong executive leadership to champion a unified vision and the implementation of integrated technology platforms that create a single source of truth for all customer data.
This transformation also ignites a strategic debate over the ideal operating model: should companies build these new data and digital capabilities in-house, or should they continue to rely on external agencies? There is a robust discussion in the industry around this topic, with a clear trend emerging toward hybrid models.17 While in-house teams can offer deeper brand knowledge, tighter alignment with corporate goals, and greater cost control, building these capabilities requires significant investment in talent and technology. External agencies, conversely, offer broader industry expertise, creative innovation, and the ability to scale resources quickly. The hybrid approach seeks the best of both worlds, combining a strong internal strategic core with a network of specialized external partners.17
Finally, the sheer complexity of the new landscape is fostering a greater need for collaboration and knowledge sharing within the industry. A recent Fierce Pharma report noted that marketers are increasingly “craving more candid conversations with their peers”.17 As everyone navigates similar pressures—from launching in a competitive category to mastering new engagement models—the insights gained from peer-to-peer exchange are becoming as valuable as formal trend reports. This highlights the growing importance of industry forums and collaborations for collectively solving shared challenges.17
Section 5.3: Outlook 2030: Key Trends on the Future of Pharma Commercialization
Synthesizing forward-looking analyses from industry leaders like Deloitte and McKinsey provides a clear vision of the forces that will shape pharmaceutical commercialization through the end of the decade. The trends identified in the current environment are not fleeting; they are foundational shifts that will continue to accelerate.
- Pervasive Digital Transformation and AI Integration: The industry’s investment in digital and AI will move from experimentation to full-scale operationalization. Nearly 60% of life sciences executives plan to increase their investments in generative AI across the entire value chain, from R&D to commercial operations.10 AI implementation is expected to generate significant value, with potential cost savings of up to 12% of total revenue for some medtech companies and value generation of up to 11% of revenue for biopharma over the next five years.10
- Intensifying Pricing and Competitive Pressures: Pricing and market access will remain the single most significant issue facing the industry.10 The ongoing patent cliff, coupled with increased competition from generics, biosimilars, and novel therapies in crowded classes like oncology and immunology, will keep margins under pressure. This environment will further fuel the imperative for companies to demonstrate clear clinical and economic value.
- The Ascendant Health Consumer: The empowerment of patients will continue to reshape the market. Consumers will demand more personalization, frictionless support services, and enhanced digital technologies.10 This trend is likely to drive further experimentation with direct-to-consumer (D2C) models, as pioneered by companies like Lilly and Pfizer, potentially moving these programs from the fringes to the mainstream.10
- Navigating Business Volatility: The need for operational resilience will remain a top priority. Geopolitical instability, climate-related disruptions, and the inherent fragility of complex global supply chains will force companies to continue fortifying their manufacturing and distribution networks. This is a particularly acute concern for the medtech sector, where 48% of executives cited supply chain risks as a significant threat to their 2025 strategy.10
- A Renewed Focus on Broad Innovation: While investment in high-science areas like oncology and rare diseases will continue, the blockbuster success of GLP-1 agonists in treating obesity and related conditions is revitalizing interest in general medicines for common conditions.2 This signals a potential rebalancing of R&D portfolios, creating new competitive dynamics in both specialty and primary care markets.
Conclusion: Competing on a New Axis of Value
The pharmaceutical industry is navigating a period of profound and irreversible change. The legacy commercial model, built for a bygone era of mass markets and lengthy monopolies, is no longer fit for purpose. The convergence of the patent cliff, empowered stakeholders, and a data-rich technological landscape has created a new playbook for market leadership.
The diagnosis is clear: the old foundations are crumbling under the weight of unprecedented financial pressure and a seismic shift in stakeholder expectations. The path forward is powered by a new fuel—the vast ecosystem of real-world and patient-generated data—and a new engine—the transformative power of artificial intelligence and predictive analytics. This foundation enables the construction of new commercial blueprints built on patient-centricity, value-based economics, and hyper-personalized engagement.
However, the analysis reveals that the most successful pharmaceutical company of 2030 will compete not just on the scientific merit of its molecules, but on a new axis of value defined by the sophistication of its data intelligence, the seamlessness of its customer experience, and the trustworthiness of its brand. The old product-centric world, where the best molecule always won, is giving way to a new ecosystem where mastering the flow of information and building trusted relationships is paramount. This requires a deep commitment to ethical governance, as privacy, equity, and transparency are no longer compliance issues but central pillars of commercial strategy. In the coming decade, the most durable competitive advantage—the “brand moat” of the future—will be built not of patents alone, but on a foundation of trust. The companies that master this new playbook will not just survive the current disruption; they will define the next era of market leadership and, in doing so, create a more effective, efficient, and equitable future for healthcare.
Works cited
- The New Pharma Playbook: From Data Overload to Market Domination – DrugPatentWatch, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/new-business-models-for-pharmaceutical-marketing-transforming-data-into-market-domination/
- 2025 May Be a Year of Innovation, Growth for Life Sciences and Health Care – Deloitte, accessed October 3, 2025, https://www.deloitte.com/us/en/Industries/life-sciences-health-care/blogs/health-care/may-be-a-year-of-innovation-growth-for-life-sciences-and-health-care.html
- How Patient Centricity is Reshaping Pharma Marketing Landscape …, accessed October 3, 2025, https://newristics.com/how-patient-centricity-is-reshaping-pharma-marketing-landscape.php
- Top Strategies for Pharma Profitability after Drug Patents Expire …, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/top-strategies-for-pharma-profitability-after-drug-patents-expire/
- Patent protection strategies – PMC, accessed October 3, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3146086/
- Patent Cliff in Pharma: Navigating Disruption and Creating Opportunity – Global Pricing, accessed October 3, 2025, https://globalpricing.com/patent-cliff-in-pharma-navigating-disruption-and-creating-opportunity/
- Navigating the Patent Cliff: Precision Print Campaigns for Pharma’s Evolving Landscape – RxJam, accessed October 3, 2025, https://rxjam.com/blog/navigating-the-patent-cliff-precision-print-campaigns-for-pharmas-evolving-landscape/
- Patent Defense Isn’t a Legal Problem. It’s a Strategy Problem. Patent Defense Tactics That Every Pharma Company Needs – Drug Patent Watch, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/patent-defense-isnt-a-legal-problem-its-a-strategy-problem-patent-defense-tactics-that-every-pharma-company-needs/
- What to Expect from Drug Patent Litigation – DrugPatentWatch …, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/what-to-expect-from-drug-patent-litigation/
- 2025 life sciences outlook | Deloitte Insights, accessed October 3, 2025, https://www.deloitte.com/us/en/insights/industry/health-care/life-sciences-and-health-care-industry-outlooks/2025-life-sciences-executive-outlook.html
- Pharma Marketing ROI 2025: Analytics That Matter – Valuebound, accessed October 3, 2025, https://www.valuebound.com/resources/blog/Pharma-marketing-ROI
- Understanding Value-Based Care Models – Oracle, accessed October 3, 2025, https://www.oracle.com/health/value-based-care-models/
- Sustained Growth Amidst Reshaping: Deloitte 2025 Life Sciences Outlook, accessed October 3, 2025, https://www.deloitte.com/cn/en/Industries/life-sciences-health-care/research/2025-life-sciences-executive-outlook.html
- Deloitte Life Sciences and Health Care 2025 Outlook: Capturing Market Share Will Likely Hinge on Understanding the Consumer and Embracing Industry Convergence – PR Newswire, accessed October 3, 2025, https://www.prnewswire.com/news-releases/deloitte-life-sciences-and-health-care-2025-outlook-capturing-market-share-will-likely-hinge-on-understanding-the-consumer-and-embracing-industry-convergence-302290817.html
- The Role of Digital Marketing in Revolutionizing the Pharma Industry: Strategies and Success Stories – MarketBeam, accessed October 3, 2025, https://marketbeam.io/the-role-of-digital-marketing-in-revolutionizing-the-pharma-industry-strategies-and-success-stories/
- AI in healthcare marketing: What’s making an impact in 2025, accessed October 3, 2025, https://blog.doceree.com/ai-in-healthcare-marketing-and-its-impact-in-2025
- Pharma Marketing in 2025: A Conversation with Fierce Pharma …, accessed October 3, 2025, https://www.fiercepharma.com/sponsored/pharma-marketing-2025-conversation-fierce-pharma
- The Pharmaceutical Patent Playbook: Forging Competitive …, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/developing-a-comprehensive-drug-patent-strategy/
- A vision for Medical Affairs in 2025 – McKinsey, accessed October 3, 2025, https://www.mckinsey.com/~/media/mckinsey/industries/life%20sciences/our%20insights/a%20vision%20for%20medical%20affairs%20in%202025/a-vision-for-medical-affairs-in-2025.pdf
- Generative AI’s Impact on Pharmaceutical Marketing | Ideas Exchange – Klick Health, accessed October 3, 2025, https://idx.klick.com/articles/generative-ais-impact-on-pharmaceutical-marketing
- How AI Is Transforming Pharma Marketing in 2025 – L7 Creative, accessed October 3, 2025, https://www.l7creative.com/ai-marketing/ai-transforms-pharma-marketing-2025/
- The Crucial Role of Real-Time Data Use in Pharma Marketing – IQVIA, accessed October 3, 2025, https://www.iqvia.com/blogs/2024/11/the-crucial-role-of-real-time-data-use-in-pharma-marketing
- Data-Driven Marketing for Healthcare: How You Can Improve Campaign ROI | Alpha Sophia, accessed October 3, 2025, https://www.alphasophia.com/blog-post/data-driven-marketing-for-healthcare-how-you-can-improve-campaign-roi
- ZS publishes book on reinventing patient centricity and using patient-led business models, accessed October 3, 2025, https://www.zs.com/insights/book-reinventing-patient-centricity-patient-led-business-models
- Case Study: Transforming Patient Support Through Managed BPO, accessed October 3, 2025, https://www.emergetalent.com/post/case-study-transforming-patient-support-through-managed-bpo
- Case Studies on the Use of Patient-centric Sampling for Clinical …, accessed October 3, 2025, https://pubmed.ncbi.nlm.nih.gov/40830292/
- Value-Based Contracts | National Pharmaceutical Council, accessed October 3, 2025, https://www.npcnow.org/topics/alternative-payment-models/value-based-contracts
- Value-Based Contracting and Pharmacy Benefit: Challenges and Sources of Incremental Improvement – L.E.K. Consulting, accessed October 3, 2025, https://www.lek.com/sites/default/files/PDFs/vbc-pharmacy-benefit_web.pdf
- How Value-Based Payment Can Improve Drug Spending, Utilization, and Equity, accessed October 3, 2025, https://www.commonwealthfund.org/blog/2023/how-value-based-payment-can-improve-drug-spending-utilization-and-equity
- Evolution of Patient-Centricity in the Multi-Indication Pharmaceutical Era – IQVIA, accessed October 3, 2025, https://www.iqvia.com/blogs/2025/03/evolution-of-patient-centricity-in-the-multi-indication-pharmaceutical-era
- Pay-for-Performance and Value-Based Care – StatPearls – NCBI Bookshelf, accessed October 3, 2025, https://www.ncbi.nlm.nih.gov/books/NBK607995/
- Value-Based Contracting for Pharmaceuticals: Getting Ready for Prime Time? | AJMC, accessed October 3, 2025, https://www.ajmc.com/view/value-based-contracting-for-pharmaceuticals-getting-ready-for-prime-time
- The Alchemist’s Playbook: Transforming Drug Patent Data into Financial Gold with Advanced IP Valuation and Financing Models – DrugPatentWatch, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/the-alchemists-playbook-transforming-drug-patent-data-into-financial-gold-with-advanced-ip-valuation-and-financing-models/
- The Dark Reality of Drug Patent Thickets: Innovation or Exploitation …, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/the-dark-reality-of-drug-patent-thickets-innovation-or-exploitation/
- Patent Litigation in the Pharmaceutical Industry: Key Considerations – PatentPC, accessed October 3, 2025, https://patentpc.com/blog/patent-litigation-in-the-pharmaceutical-industry-key-considerations
- Humira – I-MAK, accessed October 3, 2025, https://www.i-mak.org/wp-content/uploads/2020/10/i-mak.humira.report.3.final-REVISED-2020-10-06.pdf
- Biological patent thickets and delayed access to biosimilars, an …, accessed October 3, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9439849/
- AbbVie’s Enforcement of its ‘Patent Thicket’ For Humira Under the BPCIA Does Not Provide Cognizable Basis for an Antitrust Violation | Mintz, accessed October 3, 2025, https://www.mintz.com/insights-center/viewpoints/2231/2020-06-18-abbvies-enforcement-its-patent-thicket-humira-under
- Ethical Issues of Drug Patents: A Crucial Topic for A Level GP Paper – Supernova, accessed October 3, 2025, https://gpsupernova.sg/role-of-patents-in-pharmaceutical-biomedical-innovation
- Patent Evergreening In The Pharmaceutical Industry: Legal …, accessed October 3, 2025, https://ijlsss.com/patent-evergreening-in-the-pharmaceutical-industry-legal-loophole-or-strategic-innovation/
- Drug patents: the evergreening problem – PMC, accessed October 3, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3680578/
- Drug patents: the high price of watchdog litigation – PMC, accessed October 3, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3680579/
- Pharmaceutical Patent Challenges: Company Strategies and Litigation Outcomes, accessed October 3, 2025, https://www.journals.uchicago.edu/doi/abs/10.1162/AJHE_a_00066
- IP Landscape Analysis is a Strategic Necessity for Modern Businesses – UnitedLex, accessed October 3, 2025, https://unitedlex.com/insights/ip-landscape-analysis-is-a-strategic-necessity-for-modern-businesses/
- Strategic Patenting in the Pharmaceutical Landscape – Parabolic Drugs, accessed October 3, 2025, https://parabolicdrugs.com/strategic-patenting-in-the-pharmaceutical-landscape/
- Marketing Your Patented Drug Effectively: Strategies for Maximizing …, accessed October 3, 2025, https://www.drugpatentwatch.com/blog/marketing-your-patented-drug-effectively-strategies-for-maximizing-patent-protection-and-exclusivity/
- Customer Success Stories – Biotechblog, accessed October 3, 2025, https://www.biotechblog.com/category/customer-success-stories/
- Drug Patent Watch: Generic Drug Pricing Requires Market Awareness, Data Analysis, and Stakeholder Collaboration – GeneOnline News, accessed October 3, 2025, https://www.geneonline.com/drug-patent-watch-generic-drug-pricing-requires-market-awareness-data-analysis-and-stakeholder-collaboration/
- How to Determine Patent ROI to Guide Budget Decisions | PatentPC, accessed October 3, 2025, https://patentpc.com/blog/how-to-determine-patent-roi-to-guide-budget-decisions
- Evaluating Patent ROI: Which Patents to Keep, Sell, or Let Go | PatentPC, accessed October 3, 2025, https://patentpc.com/blog/evaluating-patent-roi-which-patents-to-keep-sell-or-let-go
- A Framework to Extract ROI from Your Patent Portfolio – Patentskart, accessed October 3, 2025, https://patentskart.com/a-framework-to-extract-roi-from-your-patent-portfolio/
- Ethical Challenges Posed by Big Data – PMC, accessed October 3, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7819582/
- Ethics and Big Data in Drug Development – Newsroom – Alphanumeric Systems, accessed October 3, 2025, https://blog.alphanumeric.com/newsroom/ethics-and-big-data-in-drug-development
- Ethical Challenges in Pharmaceutical Marketing: A Multidimensional Analysis of Healthcare Industry Practices – ResearchGate, accessed October 3, 2025, https://www.researchgate.net/publication/389678483_Ethical_Challenges_in_Pharmaceutical_Marketing_A_Multidimensional_Analysis_of_Healthcare_Industry_Practices
- 2025 life sciences outlook | Deloitte Australia, accessed October 3, 2025, https://www.deloitte.com/au/en/Industries/life-sciences-health-care/analysis/global-life-sciences-sector-outlook.html