Executive Summary
The proliferation of generic drugs represents one of the most significant public health and economic achievements in modern healthcare, saving the U.S. system billions of dollars annually and dramatically expanding patient access to essential medicines. Despite this, a persistent and costly paradox remains: while patients and the public overwhelmingly acknowledge the financial benefits of generics, a substantial portion harbor deep-seated reservations about their personal use. This hesitancy is not rooted in a single misconception but in a complex web of psychological biases, sociological distrust, communication failures, and systemic barriers. Consequently, the full potential of generic drugs to enhance medication adherence, improve health equity, and ensure healthcare sustainability remains unrealized.
This report provides a comprehensive strategic framework for stakeholders across the healthcare ecosystem to move beyond reactive, fact-sheet-based education toward a proactive, multi-layered approach to building patient trust in generic medicines. It deconstructs the core drivers of patient skepticism, from the pervasive “cheaper is inferior” heuristic to a fundamental distrust in the pharmaceutical industry and the broader medical system. The analysis reveals that patient education is not merely about conveying information but is a clinical intervention in itself, capable of mitigating the nocebo effect and improving therapeutic outcomes.
The foundational strategy presented herein is built on three pillars. First, it establishes a clear, authoritative understanding of the rigorous science and global regulatory consensus that guarantee the bioequivalence and quality of generic drugs, providing the factual bedrock to counter misinformation. Second, it outlines an evidence-based communication framework for healthcare professionals—the most trusted messengers—transforming their role from simple information providers to active endorsers who can leverage the patient-provider relationship to build confidence. This includes tailoring communication to the unique needs of diverse patient populations, recognizing that generic drug education is a critical component of health equity.
Finally, this report argues for a paradigm shift, urging health systems and payers to adopt the strategic foresight of the pharmaceutical industry. By leveraging publicly available market intelligence, such as patent expiry data, stakeholders can launch proactive, timed educational campaigns that reframe the introduction of a generic from an unexpected “switch” to a planned, positive “upgrade” in a patient’s care. This strategic approach, complemented by an analysis of successful initiatives from leading U.S. health systems and international policy models, provides a detailed roadmap for a coordinated, system-wide effort. The ultimate goal is to align patient perception with scientific reality, ensuring that the immense value of generic drugs is fully embraced by the individuals they are designed to serve.
Section 1: The Paradox of Patient Perception: Cost, Value, and Hesitancy
The landscape of patient attitudes toward generic drugs is defined by a significant and persistent contradiction. On one hand, patients demonstrate a clear intellectual understanding and appreciation for the economic value that generics bring to the healthcare system. On the other, a considerable degree of personal hesitancy and brand preference remains, creating a critical gap between public acknowledgment and private behavior. This paradox is the central challenge that any successful educational strategy must address.
The Acknowledged Value
Data from national surveys consistently affirms that patients recognize the primary benefits of generic drugs, particularly their cost-effectiveness. An overwhelming 94% of commercially insured adults believe that generics are less expensive than their brand-name counterparts, and over 70% agree that they represent a “better value”.1 This perception is grounded in reality; generic medications can cost 20% to 90% less than the original brand products, offering substantial savings to both patients and the healthcare system.2 The systemic impact is profound: in the United States, generics account for approximately two-thirds of all prescriptions filled but constitute less than 13% of total drug expenditures.1
However, this broad agreement on value does not translate directly into personal preference. A pivotal study found that while 56% of Americans believe the country should utilize more generic drugs, only 37.6% personally prefer to take them.1 This disconnect highlights a “not in my medicine cabinet” phenomenon, where the abstract public good of cost savings is often outweighed by personal reservations when an individual’s own health is at stake.
The Influence of Branding and Generational Trust
Patient choice is not a purely rational calculation of cost and clinical benefit; it is heavily influenced by the powerful, non-clinical forces of branding and trust. Decades of marketing by pharmaceutical companies have cultivated a strong association between brand names and quality, an association that educational efforts must actively counteract. A significant majority (62%) of Americans report trusting brand-name medications more than generics, even if financial pressures lead them to choose the lower-cost option.3 In fact, 60% of patients state they would prefer the brand-name drug but opt for the generic due to its lower price, indicating that for many, the choice is a compromise rather than a confident selection.3
This brand preference is particularly pronounced among younger generations. Gen Z, the youngest cohort of adult patients, is the most likely to favor brand-name medications. Their reasoning is rooted in core marketing principles: greater trust in the brand (78%), familiarity with the name (69%), and a belief that a well-known brand signifies higher quality (59%).3 This preference extends to specific treatment areas, with Gen Z showing a stronger inclination for branded drugs when treating conditions they perceive as more serious or impactful, such as mental health (38% preference for brand) and pain relief (33%).3 This suggests that as the perceived risk of a condition increases, so does the reliance on the perceived safety of a familiar brand.
The influence of consumer product marketing on healthcare decisions is becoming increasingly explicit. A striking finding reveals that for one in ten Gen Z and Millennial patients, the preference for a brand-name drug is based on the packaging alone.3 This signals a profound shift in patient behavior, where the aesthetic and “user experience” of a medication—its packaging, and by extension, the color, shape, and size of the pill itself—are no longer minor details. They are integral components of the product that directly influence patient trust, perception of quality, and ultimately, the choice of therapy. Healthcare systems and generic manufacturers that fail to recognize and address this consumerization of medicine risk being unable to connect with and build trust among younger patient populations.
The Disconnect Between General Belief and Personal Action
The core paradox lies in the chasm between what patients believe is a logical, beneficial choice for society and what they are comfortable choosing for themselves. The decision-making process appears to be governed by a “Public Good vs. Personal Risk” fallacy. Patients frame the choice as an implicit trade-off: they understand that widespread generic use is a collective benefit that saves the healthcare system money, but they perceive the personal adoption of a generic as a potential risk. Is this cheaper, different-looking pill really as good for me? This psychological framing—pitting a diffuse societal gain against a concrete personal uncertainty—is a formidable barrier to uptake.
This is not a failure to understand cost; it is a perceived gamble with one’s own health, fueled by a lack of deep confidence in the equivalence of the generic product. The concept of “brand response,” a term describing the comprehensive physiological and psychological effect of a drug brand, demonstrates that this preference can have tangible effects, influencing both patient compliance and the perceived efficacy of a treatment.4 Therefore, educational strategies must pivot away from emphasizing systemic cost savings. While important, that message reinforces the “public good” side of the fallacy. To be successful, communication must directly address the “personal risk” perception, reassuring individual patients that the choice of a generic is not a sacrifice or a compromise, but an identical, equally effective, and smarter therapeutic choice for
their specific health needs.
Section 2: Deconstructing Mistrust: Sociological, Psychological, and Literacy Barriers
Patient skepticism toward generic drugs is not a simple matter of misinformation. It is a complex phenomenon rooted in deep-seated psychological biases, sociological distrust of institutions, and fundamental deficits in health literacy. To effectively educate patients, it is essential to first understand and deconstruct these underlying barriers, which often operate below the surface of conscious decision-making.
The “Cheaper is Inferior” Heuristic
In nearly every consumer market, price serves as a powerful signal of quality. This cognitive shortcut, or heuristic, is deeply ingrained and is automatically applied by many patients to their medications. The lower cost of generic drugs, their single greatest advantage, thus becomes a primary driver of mistrust.5 Qualitative studies have captured this sentiment vividly, with patients describing generics as analogous to “cheap brand” groceries or asserting they are “not as good as the real medicine”.6 This belief that a less expensive product must be of lower quality is a formidable barrier, particularly among patients from lower socioeconomic backgrounds who may have more experience with markets where price and quality are indeed tightly correlated.7 This heuristic provides a simple, albeit incorrect, explanation for the price difference, and it is a narrative that educational efforts must directly and convincingly dismantle.
Sociological Distrust in Systems
A patient’s trust in a specific pill is inextricably linked to their trust in the broader systems that develop, approve, regulate, and dispense it. This distrust operates on multiple levels and often compounds, creating a powerful undercurrent of skepticism.
First, there is a widespread public distrust of the pharmaceutical industry itself. The industry is frequently perceived as prioritizing profits over patient well-being, a perception fueled by high drug prices and media narratives surrounding marketing practices and conflicts of interest.9 This general suspicion is easily transferred to generic drugs, which can be misconstrued as just another cost-cutting measure designed to benefit corporate or insurer bottom lines at the patient’s expense.
Second, for many, particularly those in disadvantaged and marginalized communities, this is compounded by a deeper mistrust of the medical system as a whole. Research in communities in the rural South, for instance, has uncovered beliefs that doctors’ prescribing habits are influenced by financial incentives from drug companies and a pervasive feeling that poorer patients are forced to “settle” for inferior generic care because they cannot afford the “real” medicine.6 This sense of being a “guinea pig” or receiving second-class treatment is a profound sociological barrier that cannot be overcome with simple facts about bioequivalence. Trust in the individual physician, however, can act as a powerful mediator. A long-term, trusting patient-physician relationship can serve as a bulwark against this systemic distrust, making the provider’s endorsement the single most critical factor in a patient’s acceptance of a generic drug.7
The Critical Role of Health Literacy
Health literacy—the capacity to obtain, process, and understand basic health information to make appropriate decisions—is a crucial variable that amplifies all other barriers.12 An estimated 90 million American adults have limited health literacy, which places them at a significantly higher risk for misunderstanding medication instructions and for adverse health outcomes.13 Patients with lower levels of health literacy are demonstrably more likely to believe that generic drugs are less safe and less effective.5 They find it difficult to grasp complex regulatory concepts like “bioequivalence,” leaving them more susceptible to the “cheaper is inferior” heuristic and other pervasive myths.14
This reality necessitates that all patient education efforts adopt a “universal precautions” approach, a principle which assumes that all patients, regardless of their apparent level of education, benefit from communication that is simple, clear, and direct.12 This includes the use of plain language, visual aids, and techniques like the teach-back method to ensure comprehension.15
The Impact of Physical Differences and Uncommunicated Switches
The tangible experience of receiving a generic drug can itself be a source of anxiety and mistrust. By law, generic drugs must not look identical to their brand-name counterparts due to trademark regulations.16 This means a patient may receive a pill of a different color, shape, or size, which can cause confusion and alarm, leading some to question if they have received the wrong medication and to stop taking it altogether.17
This anxiety is dramatically exacerbated when the switch from a brand-name to a generic drug is made without prior communication. Studies consistently show that a primary source of negative patient perception is the feeling of disempowerment and surprise that comes from not being asked or informed about the change beforehand.17 An unannounced switch can feel like a unilateral decision made by an impersonal system, confirming a patient’s pre-existing fears and suspicions.
This confluence of negative cues—a cheaper price, a different appearance, and a lack of communication—can trigger a tangible clinical barrier known as the nocebo effect. This is a phenomenon where the negative expectation of harm leads to the experience of real, perceived negative symptoms. A patient who is primed to believe a new, different-looking, cheaper pill will be inferior may attribute any subsequent adverse feeling to the generic drug, even if there is no pharmacological basis for it.8 This transforms a perception issue into a clinical one. Therefore, the communication strategy surrounding a generic substitution is not merely an educational exercise; it is a crucial clinical intervention designed to build positive expectations, foster trust, and prevent the nocebo effect from compromising therapeutic outcomes.
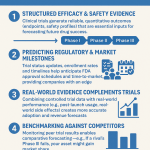
Section 3: The Foundation of Trust: Demystifying Bioequivalence and Regulatory Rigor
To effectively counter the deep-seated mistrust and misinformation surrounding generic drugs, all educational strategies must be built upon a foundation of clear, authoritative, and easily understandable facts. This requires demystifying the science of bioequivalence and illuminating the stringent regulatory processes that guarantee the quality, safety, and efficacy of every approved generic medicine. This section provides the factual bedrock for building patient confidence.
The Global Standard: Defining a Generic Drug
At its core, a generic drug is a copy of a brand-name drug that has been proven to be therapeutically equivalent. The definition is consistent across major international regulatory bodies. A generic medicine must contain the identical active pharmaceutical ingredient (API)—the chemical that makes the drug work—in the exact same strength and dosage form (e.g., tablet, capsule), and be administered via the same route (e.g., oral, injectable) as the original innovator product.2 The fundamental principle is that the generic drug is designed to be interchangeable with the brand-name drug, providing the same clinical benefit and safety profile.7
The Regulatory Gauntlet: The FDA and EMA Approval Processes
Generic drugs are not unregulated copies; they are subject to a rigorous and comprehensive review process by highly respected regulatory agencies like the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA).19 The narrative that this process is somehow less thorough than the one for brand-name drugs is a critical misconception that must be corrected.
In the United States, the landmark Drug Price Competition and Patent Term Restoration Act of 1984, commonly known as the Hatch-Waxman Act, established the Abbreviated New Drug Application (ANDA) pathway.25 The process is termed “abbreviated” not because it cuts corners on safety or quality, but because it avoids the unethical and unnecessary duplication of expensive clinical trials that have already proven the original drug’s active ingredient to be safe and effective.2 Instead of repeating these human trials, the ANDA process focuses on proving sameness. The generic manufacturer must demonstrate through extensive testing that their product meets the same high standards for quality, strength, purity, and stability as the brand-name drug. Furthermore, the FDA conducts rigorous inspections of manufacturing facilities to ensure they adhere to the same strict Good Manufacturing Practices (GMP) required of brand-name manufacturers.14
The European Union employs a similarly robust system, with multiple pathways for approval that all ensure the highest standards of quality, safety, and efficacy are met.23 The remarkable degree of global consensus on these standards is evidenced by the fact that there is a 95% concordance rate in the final approval decisions between the FDA and EMA for generic drug applications submitted to both agencies.28 This alignment underscores that the principles of generic drug evaluation are based on a shared, rigorous scientific foundation across the developed world.
Explaining Bioequivalence in Plain Language
The concept of bioequivalence is the scientific cornerstone of generic drug approval, yet it is also the most frequently misunderstood. Communicating it clearly is paramount.
The technical definition states that two drugs are bioequivalent when there is no significant difference in the rate and extent to which the active ingredient becomes available at the site of drug action when administered at the same dose.25 This is measured in human volunteers by analyzing blood samples over time to determine two key pharmacokinetic parameters: the maximum concentration of the drug in the blood (
Cmax) and the total exposure to the drug over time, known as the Area Under the Curve (AUC).25
A pervasive myth, often used to create doubt about generics, is that the FDA allows a generic’s potency to vary by as much as 45% from the brand-name drug. This is a fundamental misinterpretation of the statistics.30 The FDA’s bioequivalence standard requires that the 90% confidence interval for the ratio of the generic’s to the brand’s average AUC and
Cmax values must fall entirely within the limits of 80% to 125%.29 For this strict statistical requirement to be met, the actual measured difference in bioavailability between the generic and brand-name products is, on average, extremely small—approximately 3.5%.31 This level of variation is comparable to the difference observed between two different manufacturing batches of the
same brand-name drug.31
A simple, effective analogy can help patients grasp this concept: “Bioequivalence means the generic drug delivers the same amount of the active medicine to the part of your body where it’s needed, in the same amount of time as the brand-name drug. Think of it like two high-quality cars taking slightly different routes through a city but arriving at the exact same destination at the exact same time. The FDA’s strict tests are like a GPS verification that proves they perform identically.”
Addressing Differences: Inactive Ingredients and Appearance
It is crucial to proactively explain the legally mandated and clinically insignificant differences between generic and brand-name drugs.
- Inactive Ingredients: While the active ingredient must be identical, generic drugs may contain different inactive ingredients, also known as excipients. These are substances like fillers, binders, and coloring agents that help form the pill and ensure its stability.16 These excipients are also reviewed and approved by the FDA and rarely cause any clinically significant problems. In very rare instances, a patient may have a specific allergy to an inactive ingredient like a certain dye or lactose, which is why it is important for patients to discuss all allergies with their pharmacist and doctor.16
- Appearance: Trademark laws explicitly prohibit a generic drug from looking identical to its brand-name counterpart. This is the reason for differences in a pill’s shape, color, or size.16 It is essential to frame this for patients not as a sign of a different medicine, but as a legal requirement analogous to different brands of soda having different logos on their cans. These cosmetic differences have no impact on the drug’s therapeutic action.20
By reframing the regulatory process as a story of patient protection and by using clear, simple analogies to explain the science of bioequivalence, healthcare stakeholders can build a powerful, fact-based narrative that directly counters misinformation and serves as the unshakable foundation for patient trust.
Table 1: Comparative Overview of Generic Drug Regulatory Approval: FDA (U.S.) vs. EMA (E.U.)
This table provides a high-level comparison of the regulatory frameworks for generic drugs in the United States and the European Union, highlighting the strong alignment on core scientific and quality standards. This demonstrates a global consensus on the requirements for ensuring generic medicines are safe, effective, and interchangeable with their brand-name counterparts.
| Feature | FDA (U.S.) | EMA (E.U.) |
| Governing Legislation | Drug Price Competition and Patent Term Restoration Act of 1984 (Hatch-Waxman Act) 25 | EU Directives and Regulations (e.g., Directive 2001/83/EC) 23 |
| Primary Application | Abbreviated New Drug Application (ANDA) 26 | Marketing Authorisation Application (MAA) for a generic medicine 23 |
| Key Requirement | Demonstration of pharmaceutical equivalence and bioequivalence to a Reference Listed Drug (RLD) 25 | Demonstration that the medicine is a ‘generic’ of a ‘reference medicine’ already authorised in the EU 23 |
| Bioequivalence Standard | The 90% confidence interval of the ratio of geometric means for AUC and Cmax must be within 80.00% to 125.00% 29 | The 90% confidence interval for the ratio of the test and reference products for AUC and Cmax should be within the acceptance interval of 80.00% to 125.00% 7 |
| Manufacturing Standard | Adherence to Current Good Manufacturing Practices (cGMP); facilities are subject to FDA inspection 14 | Adherence to Good Manufacturing Practice (GMP); facilities are subject to inspection by national competent authorities 20 |
| Labeling | Labeling must be the same as the brand-name drug’s labeling, with certain permissible differences 25 | The Summary of Product Characteristics (SmPC) is based on that of the reference medicine, with differences allowed for aspects covered by patent law 23 |
| Post-Market Surveillance | FDA monitors adverse event reports and product quality issues for all drugs on the market 24 | National competent authorities and the EMA monitor the safety of all medicines on the market (pharmacovigilance) 20 |
Section 4: The Front Lines of Education: A Communication Framework for Healthcare Professionals
While systemic policies and public campaigns play a vital role, the most critical interactions in patient education occur in clinics and pharmacies. Healthcare professionals—physicians, pharmacists, and nurses—are consistently ranked as the most trusted sources of health information. Their ability to communicate effectively and build confidence is the linchpin of any successful strategy to increase the acceptance and proper use of generic drugs.
The Primacy of the Provider
The influence of a healthcare professional in a patient’s decision-making process cannot be overstated. Research consistently shows that patient comfort and acceptance of a generic medication increase significantly when a physician or pharmacist takes the time to discuss the substitution with them.5 In many cases, a patient’s trust in their provider is strong enough to override their personal skepticism or mistrust of the broader pharmaceutical and healthcare systems.7 This dynamic means that provider communication is not merely an adjunct to an educational strategy; it is the single most important educational intervention. A provider’s confidence, clarity, and endorsement can transform a moment of uncertainty into an affirmation of quality care.
However, this influence can be a double-edged sword. Any perceived hesitation or lack of knowledge on the part of the provider can amplify a patient’s existing fears. Studies have shown that certain provider groups, such as specialists or older physicians, may be less likely to prescribe or recommend generics.1 If a provider uses equivocal language, such as, “You can
try the generic and see how it goes,” a patient will rightly interpret this as a lack of confidence, confirming their suspicion that the generic is an inferior option. Therefore, a comprehensive educational strategy must begin with robust provider education, ensuring that clinicians themselves are well-informed, confident, and consistent messengers.
Core Principles of Patient-Centered Communication
Effective education is built on the foundation of a strong, trusting provider-patient relationship. This requires adopting patient-centered communication techniques that prioritize the patient’s perspective and concerns.
- Listen First, Talk Second: The conversation should always begin with an open-ended inquiry to assess the patient’s existing knowledge, beliefs, and fears. Simple questions like, “What have you heard about generic medicines?” or “When the pharmacist offers you the generic version of this, what are your main concerns?” create a space for the patient to voice their perspective.38 This diagnostic step is crucial; it allows the provider to tailor their explanation to the patient’s specific worries rather than delivering a generic script.
- Empathize and Validate Concerns: It is vital to acknowledge and validate the patient’s feelings, even if they are based on misinformation. Dismissing a concern as unfounded can make a patient feel unheard and defensive. Simple, empathetic statements like, “I can certainly understand why a change in your medication would make you feel anxious,” or “That’s a very common question, and it’s smart to be cautious,” build rapport and demonstrate that the provider is a partner, not an adversary.38
- Frame as a Shared Decision: The goal is to engage the patient in a process of shared decision-making. This involves clearly explaining the options (brand vs. generic), providing a concise rationale for the recommendation (e.g., identical active ingredient, rigorous FDA testing, significant cost savings), and explicitly asking for the patient’s input and agreement.39 This collaborative approach respects patient autonomy and transforms the patient from a passive recipient of a decision into an active participant in their own care.
The Pharmacist’s Crucial Role at the Point of Dispensing
Pharmacists are uniquely positioned on the front lines of generic substitution. As the most accessible healthcare professionals, they often manage the final, tangible step of the process and have a critical opportunity to either build or erode patient trust. Proactive counseling is key. Rather than waiting for a patient to express confusion about a different-looking pill, the pharmacist should initiate the conversation, explaining beforehand that the medication may look different but that it is the same medicine prescribed by their doctor.17 This simple act of pre-emption can prevent significant anxiety and non-adherence. Pharmacists should be prepared to address common questions about active versus inactive ingredients, the FDA approval process, and the reasons for the cost difference, reinforcing the messages from the prescribing physician.14
Ensuring Understanding with the “Teach-Back” Method
A cornerstone of effective patient education is closing the communication loop to ensure genuine understanding. The teach-back method is a simple but powerful tool for achieving this. After providing an explanation, the provider asks the patient to explain the information back in their own words. This is framed not as a test of the patient’s knowledge, but as a check on the provider’s ability to communicate clearly. For example, a clinician might say, “To make sure I did a good job explaining this, could you tell me what you’ll tell your husband about this new medication when you get home?”.39 The patient’s response immediately reveals any gaps in understanding, allowing the provider to clarify the information in real-time.
Ultimately, the most effective communication relies less on the simple transmission of information and more on the power of a trusted endorsement. Patients are inundated with conflicting health information from various sources. They place the most weight on the recommendation of their personal physician or pharmacist.7 Therefore, a provider who acts as a librarian, simply pointing to the facts, is less effective than one who acts as a trusted advisor. A clear, confident, personal endorsement—”I recommend this generic for you. It contains the exact same medicine, it has been proven to work just as well, and I prescribe it for my own family”—leverages the pre-existing trust in the relationship to provide powerful reassurance that no fact sheet can match.
Table 2: Evidence-Based Communication Strategies for Discussing Generic Drugs
This table provides a practical, actionable toolkit for healthcare professionals, translating core communication principles into specific techniques and example phrasing that can be used in clinical practice to build patient trust in generic medicines.
| Strategy/Technique | Description & Rationale | Example Phrasing for Physicians/Pharmacists | Supporting Evidence |
| Active Listening & Open-Ended Inquiry | Begins the conversation by assessing the patient’s existing knowledge, beliefs, and fears. This patient-centered approach allows for tailored education that directly addresses their specific concerns. | “What have you heard about generic medicines before?” “Tell me about your experiences with brand-name versus generic drugs.” “What questions or concerns do you have about me prescribing the generic version for you?” | 38 |
| Empathetic Validation | Acknowledges the patient’s feelings as legitimate, which builds rapport and reduces defensiveness. It shows the patient they are being heard and respected, making them more receptive to new information. | “I understand why you might be concerned about a change. It’s completely normal to have questions when your pill looks different.” “That’s a very common concern. Let’s talk through exactly what it means.” | 38 |
| The Endorsement | Leverages the trust inherent in the provider-patient relationship. A strong, personal recommendation is more persuasive than an impersonal recitation of facts, as it transfers the provider’s confidence to the patient. | “This generic version has the exact same active ingredient and has been rigorously tested by the FDA to work the same way. I am confident this is the right choice for you.” “I prescribe this generic version to my patients all the time, and even for my own family. It’s the same medicine.” | 5 |
| Plain Language Explanation (Bioequivalence) | Translates complex scientific and regulatory concepts into simple, relatable terms. Avoids jargon like “bioequivalent” or “ANDA” that can confuse patients and increase anxiety. | “The FDA requires the generic to deliver the same amount of the active medicine to your body in the same amount of time as the brand. It works in the exact same way.” “The reason it’s cheaper is that the generic company didn’t have to spend billions on the initial research, which was already done by the brand company. The savings are passed on to you.” | 42 |
| Proactive Management of Differences | Addresses the potential for confusion from changes in pill appearance before it happens. This pre-empts patient anxiety and reduces the risk of non-adherence due to medication uncertainty. | (Pharmacist) “When you open this bottle, you’ll notice the pill is a different color and shape than you’re used to. This is normal and required by law. It is the same medicine your doctor prescribed.” | 14 |
| Teach-Back Method | A proven technique to confirm patient understanding. It is a test of how well the provider explained the information, not a quiz for the patient. It allows for immediate correction of any misunderstandings. | “To make sure I’ve done a good job explaining everything, can you tell me in your own words how this generic medicine is the same as the brand-name one?” “What will you tell your spouse about the change we made to your medication today?” | 39 |
Section 5: Tailoring the Message: Strategies for Diverse Patient Populations
A “one-size-fits-all” approach to patient education is destined to fail. Patients are not a monolithic group; their perspectives, concerns, and learning styles are shaped by age, health status, cultural background, and life experiences. An effective educational framework must be agile and adaptable, tailoring its message and methods to meet the specific needs of diverse patient populations.
Age-Based Cohorts
Different generations interact with the healthcare system and process information in distinct ways.
- Elderly Patients: This cohort often takes multiple medications and may have established routines over many years. They can be more resistant to change and particularly sensitive to alterations in a pill’s physical appearance, which can lead to confusion and medication errors.17 Communication strategies should be characterized by patience, allowing extra time for explanation and questions. Educational materials should be provided in large, clear print. Proactively addressing the visual differences—”Your new pill for blood pressure will be a small blue one instead of the larger white one, but it is the same medicine”—is critical to prevent non-adherence. Furthermore, involving family members or caregivers in these conversations is essential, as they are often key partners in medication management.15
- Younger Adults (Millennials & Gen Z): While generally more open to the cost-saving benefits of generics, these digitally native generations are also more heavily influenced by branding and consumer aesthetics.3 They may harbor skepticism about quality, viewing generics through the same lens as off-brand consumer goods.3 Educational outreach should leverage the channels they trust, such as mobile apps, patient portals, and credible online resources.42 The message should emphasize the “smart choice”—highlighting not just the cost savings but the efficiency and scientific rigor of the generic approval process. It is also important to directly address their brand-driven quality concerns by explaining the concept of bioequivalence in clear, modern terms.
Patients with Chronic vs. Acute Conditions
The nature of a patient’s illness significantly influences their risk tolerance and receptivity to generic medications.
- Chronic Conditions: Patients managing serious, lifelong conditions such as epilepsy, cardiovascular disease, or mental health disorders often experience heightened anxiety about the stability and efficacy of their treatment. Studies show that patients are far more reluctant to accept a generic for a serious illness than for a minor, temporary one.6 For this group, education must be exceptionally reassuring. The conversation should focus on the consistency of supply, the long-term cost savings that enhance sustainability of care and improve adherence, and the fact that regulatory standards for bioequivalence are just as strict for all medications, including those with a “narrow therapeutic index” where small differences in dose could have significant clinical effects.33
- Acute Conditions: Patients being treated for short-term issues like infections or acute pain tend to be more open to generics.1 This presents a strategic opportunity for providers to create a positive first experience with a generic medication. A provider can intentionally frame this experience as an educational moment: “We’re going to use the generic version of this antibiotic. You’ll see that it works just as well to clear up your infection and it saves you money. This is the same principle of quality and value we apply to all the medications we prescribe.” This curated positive experience can build a foundation of trust that can be referenced later if a more sensitive switch for a chronic condition becomes necessary.
Cultural and Linguistic Diversity: A Health Equity Imperative
Perhaps the most critical and often overlooked dimension of tailored education is addressing cultural and linguistic diversity. Failure to do so not only renders education ineffective but also exacerbates existing health disparities.
Language discordance between a patient and provider is a primary barrier to medication safety and adherence.45 It is essential to use professional medical interpreters for patients with limited English proficiency, rather than relying on family members (especially children), who may not understand medical nuances or may filter information.42 All educational materials, from brochures to prescription labels, must be translated accurately into the primary languages of the patient population being served. These materials should use plain language, be culturally sensitive, and incorporate visual aids like pictograms to bridge literacy gaps.42
Beyond language, cultural beliefs about health, illness, and medicine can profoundly impact a patient’s perception of generic drugs. For some communities, particularly those with a history of marginalization or unethical treatment by the medical establishment, there exists a deep-seated and justified mistrust of the system.6 Within this context, the recommendation of a cheaper medication can be interpreted not as a cost-saving measure, but as evidence of receiving second-class, inferior care.
This dynamic reframes generic drug education as a fundamental issue of health equity. The data is clear: negative perceptions and mistrust of generics are disproportionately higher among non-white, low-income, and low-education populations.5 These are the very communities who stand to benefit the most from the affordability of generics but are least likely to trust them. This creates a vicious cycle where a key tool for improving access and affordability is rejected due to systemic and historical factors. Therefore, generic drug education cannot be a standalone effort. It must be integrated into broader health equity initiatives that focus on building foundational trust with marginalized communities, using culturally competent messengers, and ensuring that all patients feel respected and valued within the healthcare system. The FDA itself has recognized this link, framing increased access to affordable generic drugs as a direct pathway to promoting health equity.50
Section 6: System-Level Interventions: The Role of Policy, Payers, and International Models
While individual patient-provider interactions are the final and most personal step in education, their effectiveness is profoundly shaped by the larger systems in which they occur. Government policies, payer strategies, and international precedents create the “choice architecture” that guides the decisions of both patients and clinicians. Understanding these systemic levers is crucial for developing a comprehensive strategy that magnifies the impact of frontline educational efforts.
Government Policy and Regulation
Government actions at both the federal and state levels establish the legal and regulatory framework for the generic drug market.
- The U.S. Federal Framework: The Hatch-Waxman Act of 1984 was the foundational legislation that created the modern generic drug industry in the U.S. by establishing the ANDA pathway and streamlining market entry.26 However, the system it created is a delicate balance. It includes provisions, such as patent term extensions for brand-name drugs and automatic 30-month stays on generic approval when litigation is filed, that can be strategically employed by innovator companies to delay competition.51 These complexities can lead to patient confusion and mistrust when expected generics do not appear on the market.
- State-Level Generic Substitution Laws: The authority for a pharmacist to substitute a generic for a prescribed brand-name drug is governed by state law, leading to a patchwork of regulations across the country. These laws are generally categorized as either “permissive,” allowing the pharmacist to substitute, or “mandatory,” requiring substitution unless the prescriber explicitly writes “Dispense as Written” or a similar directive.16 Some states have carved out exceptions for specific drug classes, such as anti-epileptics, requiring patient and practitioner consent for substitution, reflecting the heightened anxiety surrounding generics for certain chronic conditions.44
- Public Awareness Campaigns: Government bodies like the FDA conduct public awareness campaigns to educate consumers and dispel common myths about generic drugs.14 While valuable, the impact of these campaigns is often limited by funding and the ability to achieve sustained reach compared to the marketing efforts of the pharmaceutical industry.
The Powerful Role of Payers
Insurance providers and pharmacy benefit managers (PBMs) are arguably the most powerful drivers of generic drug utilization in the U.S. They design and implement the financial incentives that directly influence patient and provider behavior.
- Formulary Design: The primary tool used by payers is the formulary, or drug list, which is often structured into tiers. By placing generic drugs in the lowest-cost tier (Tier 1) with minimal or no co-payment, and brand-name drugs in higher-cost tiers, payers create a strong financial incentive for patients to choose the generic option.1
- Payer-Led Initiatives: In recent years, payers have become more proactive in addressing issues of generic drug price and supply. A notable example is the collaboration of numerous Blue Cross Blue Shield companies to co-found CivicaScript, a public benefit company aimed at developing and manufacturing affordable generic medications for common conditions, thereby directly intervening in the market to ensure competition and lower costs.54 Similarly, the Centers for Medicare & Medicaid Services (CMS) has explored models like a “$2 Drug List” to test whether standardizing and simplifying co-pays for essential generics can improve adherence and outcomes for Medicare beneficiaries.55
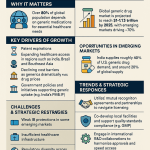
International Models: A Comparative Perspective
Examining the policies of other developed nations reveals a variety of successful strategies for promoting generic drug use and provides valuable lessons.
- United Kingdom: The National Health Service (NHS) emphasizes “generic prescribing,” a policy that encourages physicians to write prescriptions using the drug’s non-proprietary (generic) name rather than a brand name. This shifts the focus from substitution at the pharmacy to the initial prescribing decision and has resulted in one of the highest generic utilization rates in the world, at over 80%.56
- Canada: The Canadian system is decentralized, with each province and territory setting its own drug prices and interchangeability rules. Generic prices are often set as a fixed percentage of the brand-name price.58 While brand-name drugs are generally less expensive than in the U.S., some studies suggest that Canadian
generic prices can be higher due to less price competition in certain market segments.59 - Australia: Australia leverages the immense purchasing power of its national Pharmaceutical Benefits Scheme (PBS). The PBS acts as a single, powerful negotiator, driving down prices for both brand-name and generic drugs to levels significantly below those in the U.S..62 The system also mandates “active ingredient prescribing,” which requires doctors to include the generic name on prescriptions to encourage patients and pharmacists to choose the most cost-effective option.64
These different national approaches demonstrate that the decision to use a generic drug is not made in a vacuum. It is heavily influenced by the “choice architecture” created by policy and payer rules. In the U.S., the architecture is largely defined by financial incentives, requiring education to help patients navigate a complex choice. In the U.K., the architecture is shaped by the prescriber’s initial decision, requiring education that reinforces trust in that decision. In systems with mandatory substitution, education must focus on explaining the policy’s rationale and reassuring patients about the quality of the mandated switch.
This international comparison also provides a powerful tool for de-linking the price-quality heuristic in patients’ minds. The fact that U.S. prices for brand-name drugs are the highest in the world while its prices for unbranded generics are among the lowest is a critical, counterintuitive point.65 This demonstrates that price is not an inherent marker of a drug’s quality but is rather an outcome of a country’s specific market regulations, negotiating power, and competitive landscape. An educational message built around this fact can be highly effective: “The price difference you see is about our country’s market rules, not about the quality of the medicine in the bottle, which is the same.”
Table 3: International Comparison of Generic Drug Policies and Market Outcomes
This table provides a comparative summary of the policy levers, market share, and pricing environments for generic drugs in four major developed countries, illustrating how different systemic approaches can lead to varied but often successful outcomes in promoting generic utilization.
| Country | Key Policy Lever | Generic Market Share (% of Volume) | Relative Price Environment | Supporting Evidence |
| United States | Payer-driven substitution via tiered formularies; strong price competition among generic manufacturers. | ~89% | Brand prices are the highest internationally; generic prices are highly competitive and often lower than in other developed nations. | 2 |
| United Kingdom | “Generic Prescribing” at the physician level is standard practice within the National Health Service (NHS). | ~83% | Generic prices are among the lowest in Europe due to strong competition and NHS purchasing power. | 56 |
| Canada | Decentralized provincial price setting (often as a % of brand price); provincial interchangeability lists. | ~75% | Brand prices are lower than in the U.S. but higher than in many other countries. Generic prices can be higher than in the U.S. due to pricing formulas. | 58 |
| Australia | Centralized price negotiation via the Pharmaceutical Benefits Scheme (PBS); mandatory active ingredient prescribing. | High (specific % not in sources) | Both brand and generic prices are significantly lower than in the U.S. due to the government’s strong negotiating power as a single purchaser. | 63 |
Section 7: Strategic Intelligence in Patient Education: Leveraging Market Data for Proactive Campaigns
The prevailing model of patient education on generic drugs is largely reactive. It typically occurs at the point of prescribing or, more often, at the pharmacy counter when a patient is surprised by a change in their medication’s appearance. This report proposes a paradigm shift: for patient education to be truly successful, key stakeholders like health systems and payers must move from a reactive posture to a proactive, strategic function. This can be achieved by adopting the same tools of market intelligence and forward-planning used by the pharmaceutical industry itself.
The “Patent Cliff” as a Predictable Educational Opportunity
The expiration of a patent on a blockbuster, brand-name drug—an event known as the “patent cliff”—is a predictable and highly consequential moment in the pharmaceutical market.67 It is not a surprise. The dates of patent and regulatory exclusivity expiry are public knowledge, often years in advance. Upon expiry, the market dynamics shift dramatically. Generic manufacturers, who have prepared their applications in advance, can enter the market, often leading to a rapid and steep decline in the brand-name drug’s market share, which can fall by as much as 90% within months.67
Branded pharmaceutical companies do not wait for this to happen. They engage in years of strategic planning to mitigate the impact of patent expiry. This includes aggressive lifecycle management, such as developing new formulations or seeking new indications (“evergreening”), and launching sophisticated marketing and loyalty campaigns aimed at retaining both prescribers and patients well before the first generic competitor arrives.67
A New Strategy: Proactive, Timed Educational Campaigns
Health systems, insurance payers, and patient advocacy groups should adopt this same strategic, forward-looking mindset. By systematically monitoring public data on patent expiries for high-volume, high-cost drugs, these organizations can transform a moment of potential patient confusion into a planned and positive educational opportunity.
Publicly available resources, such as the FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations (commonly known as the “Orange Book”) and specialized business intelligence platforms like DrugPatentWatch, provide all the necessary data on patent numbers, expiration dates, and regulatory exclusivities.71 This information allows for the creation of a “Patient Education Calendar,” enabling a structured, multi-stage communication campaign:
- 18-24 Months Pre-Expiry: The strategic planning phase begins. The health system or payer identifies the upcoming patent expiry of a major drug. They analyze their own data to determine the specific patient and provider populations that will be affected. A cross-functional team can be assembled to begin developing the core messages and educational materials (e.g., letters, portal messages, brochures, short videos).
- 6-12 Months Pre-Expiry: The provider education phase is initiated. The organization begins communicating with its network of physicians and pharmacists about the upcoming change. This ensures that providers are well-informed, aligned on the message, and prepared to be confident endorsers of the generic when it becomes available. This phase can also include broader, unbranded disease-state awareness campaigns that subtly prepare the ground.
- 0-6 Months Pre-Expiry: The targeted patient communication phase is launched. The organization sends personalized communications directly to affected patients. This messaging should be framed as positive news, informing them that a lower-cost, identical generic version of their medication will soon be available. Crucially, this communication should proactively address the most common concerns, stating clearly, for example, that “the new pill will look different, but it contains the exact same active medicine and works in the exact same way.”
This proactive approach fundamentally reframes the patient experience. The introduction of a generic is no longer a jarring “switch” that happens to a patient, but a planned “upgrade” to their therapy that is happening for them. The current model, with its language of “switching,” inherently implies moving from a known, trusted entity to an unknown and potentially lesser one, creating uncertainty and anxiety.17 A proactive campaign controls the narrative from the outset. The message becomes: “For the past several years, you have been taking Brand X to manage your condition. We are pleased to let you know that its patent is expiring, which allows us to provide you with the
exact same medicine at a much lower cost. This is a positive development that makes your treatment more affordable and sustainable for the long term.” This simple shift in framing transforms the emotional tone of the event from one of potential loss to one of tangible gain, pre-empting the mistrust that an unexpected change at the pharmacy counter inevitably breeds.
Furthermore, in an increasingly competitive healthcare market, this level of proactive, patient-centered communication can become a powerful differentiator. A health system or insurance plan that demonstrates this competence and transparency is providing a measurably superior patient experience. It communicates to patients that their well-being—both clinical and financial—is being actively managed. This builds trust not only in the generic drug but in the healthcare organization itself, turning a logistical challenge into a valuable brand-building asset that can foster long-term patient loyalty.
Section 8: Blueprints for Success: Case Studies from Leading U.S. Health Systems and Insurers
The strategic principles for educating patients about generic drugs are not merely theoretical. They are being actively implemented, with varying degrees of proactivity and success, by major healthcare organizations across the United States. An analysis of the publicly available policies and patient-facing materials of these leading integrated delivery networks (IDNs) and national insurers provides a valuable blueprint of current best practices and reveals opportunities for further innovation.
Integrated Delivery Networks (IDNs)
IDNs, which combine insurance and care delivery, are uniquely positioned to align incentives and communication around generic drug use.
- Kaiser Permanente: As a closed-system IDN, Kaiser Permanente utilizes a single, unified drug formulary to drive prescribing patterns. Their patient education materials are direct and reassuring. They emphasize that generic drugs use the same active ingredients, are rigorously approved by the FDA, and that approximately 50% of all generics are actually manufactured by brand-name companies—a powerful and often surprising fact for patients.74 Kaiser explicitly connects the use of generics to member benefits, stating that the strategy has resulted in significant savings “in the form of lower rates and prescription prices”.75 Their policy is clear: when a generic version of a medication is available, it is typically the only version included on their formulary, making it the default and standard of care.76
- Ascension: This large, non-profit health system has taken a highly proactive, market-shaping approach. Ascension was a founding member of the collaboration that created Civica Rx, a not-for-profit generic drug company established to directly combat chronic shortages and price gouging of essential medications.77 By framing this initiative as part of its core mission to serve the poor and vulnerable, Ascension builds trust and demonstrates a commitment that goes beyond simple cost-cutting. Their formularies reinforce this by clearly endorsing the use of FDA-approved, bioequivalent generics and often designating a brand-name drug as non-formulary once a generic equivalent becomes available.78
Major National Insurers (Payers)
National payers leverage their scale and data analytics to implement sophisticated programs aimed at encouraging generic utilization.
- Anthem (Elevance Health): Anthem employs a strategy of consolidated and targeted member communication. Instead of sending multiple, disparate letters, they use tools like the “Medication Review” and “MyHealth Note” to deliver personalized messages that highlight opportunities to switch to generic or therapeutic equivalents, often including member-specific cost savings data.79 This data-driven approach makes the financial benefit of switching tangible and personal for the member. Their policy is also unambiguous: if a member chooses a medication that is not on the drug list, they are responsible for the full cost.79
- Cigna: Cigna’s educational materials for members are direct, using clear, benefit-oriented language: generics “work in the same way…but cost up to 85% less”.80 They supplement formulary design with programs like the “Patient Assurance Program,” which caps out-of-pocket costs for certain eligible medications, directly removing the financial burden for patients. Cigna also provides members with direct access to licensed pharmacists who can answer questions, explain how medications work, and suggest ways to save money, providing a valuable human touchpoint for education and support.80
- Aetna (a CVS Health company): Aetna’s member resources, such as online FAQs, provide clear, concise definitions of generic drugs, stating that they are identical to brand-name drugs in dosage, safety, strength, and quality.82 Recognizing that formulary changes can be disruptive, Aetna has implemented a formal “transition process.” This policy provides a temporary, one-month supply of a medication that is no longer on the formulary, giving the member and their doctor time to either switch to a covered alternative or request a formal exception.83 This structured process helps manage change and reduce patient anxiety. Their pharmacy drug guides explicitly state that “Generics should be considered the first line of prescribing”.84
- UnitedHealth Group (Optum Rx): UHG has taken an aggressive approach to eliminating cost as a barrier to adherence. Their prescription drug lists feature extensive zero-cost sharing ($0 co-pay) for a wide range of generic drugs used to treat common chronic conditions like hypertension and hypercholesterolemia.85 This strategy moves beyond simply making generics the
cheaper option to making them the free option, a powerful incentive for both patients and prescribers. They have also launched initiatives to increase transparency in pharmacy payment models and reduce administrative hurdles like prior authorizations, aiming to simplify the entire prescription process.86
An analysis of these industry leaders reveals a clear spectrum of proactivity. Some organizations have well-defined but essentially reactive policies, like Aetna’s “transition process,” which manages a change after it has occurred. Others, like Anthem, are more proactive, using data analytics to push personalized cost-saving opportunities to members. The most advanced organizations, such as Ascension and the BCBS companies involved with CivicaScript, have moved to a market-shaping stance, vertically integrating to create their own generic supply chains to guarantee affordability and access.54 This creates a clear maturity model against which any health system or payer can benchmark its own generic drug strategy, identifying opportunities to evolve from a reactive to a fully proactive or even market-shaping position.
However, a common gap persists. While these organizations excel at communicating the “what” (this generic is on our formulary and it is cheaper) and the “how” (use our mail-order pharmacy to fill it), they often neglect to fully address the patient’s fundamental “why” (why should I trust this medicine?). Their communication is primarily oriented around financial and logistical benefits. This leaves a crucial trust-building and educational gap that frontline providers are expected to fill. Payers have a significant opportunity to enhance their member communications by integrating the trust-centered messages outlined in this report. Instead of simply publishing a drug list, they could partner with trusted provider groups to co-brand educational materials or create and distribute simple, compelling videos that explain bioequivalence. Aligning their powerful financial incentives with a more holistic, trust-based educational approach would not only improve adherence but also enhance member satisfaction and loyalty.
Table 4: Generic Drug Initiatives and Formulary Strategies of Major U.S. Payers and Health Systems
This table provides a comparative summary of the strategies employed by leading U.S. healthcare organizations to promote the use of generic drugs, highlighting their primary initiatives and communication tools.
| Payer/Health System | Primary Strategy/Initiative | Key Patient Communication Tool | Approach to Non-Formulary Brands | Supporting Evidence |
| Kaiser Permanente | Integrated Formulary as Standard of Care | Direct member education on safety and value of generics. | When a generic is available, it is typically the only version covered on the formulary. | 74 |
| Anthem (Elevance Health) | Proactive, Data-Driven Member Messaging | “Medication Review” and “MyHealth Note” with personalized cost-savings data. | Member is responsible for the full cost if a non-formulary drug is chosen. | 79 |
| Cigna | Member Support and Cost-Capping | “Patient Assurance Program” to cap co-pays; direct access to pharmacists for counseling. | Tiered formulary with higher costs for non-preferred brands; exception process available. | 80 |
| Aetna (CVS Health) | Structured Formulary Management | “Transition Process” for members on newly non-formulary drugs; clear drug guides. | Formal transition process provides a temporary supply; exception process available. | 82 |
| UnitedHealth Group (Optum Rx) | Eliminating Cost Barriers | $0 Cost-Share lists for many generics treating chronic conditions. | Tiered formulary with significant cost differences; advocates for generic use. | 85 |
| Ascension | Non-Profit Manufacturing / Supply Chain Intervention | Public messaging frames initiative as mission-driven to serve the vulnerable. | Formulary endorses generics as first-line; brands may become non-formulary when generic exists. | 77 |
Conclusion: A Multi-Stakeholder Roadmap for Building Trust and Driving Value
The challenge of educating patients about generic drugs is not a simple communications task but a complex, system-wide imperative. Overcoming decades of brand marketing, deep-seated psychological biases, and sociological mistrust requires a coordinated and sustained effort from every stakeholder in the healthcare ecosystem. Success hinges on shifting from a reactive, information-based model to a proactive, trust-centered strategic framework. The following roadmap outlines targeted, actionable recommendations for key stakeholders to build patient confidence, improve health outcomes, and realize the full value of generic medicines.
For Healthcare Providers (Physicians & Pharmacists)
As the most trusted figures in a patient’s healthcare journey, providers are the essential front line for building confidence.
- Embrace the Role of Active Endorser: Move beyond passively providing information. Leverage the trust of the patient-provider relationship with a clear, confident, personal endorsement of the generic drug’s safety, quality, and efficacy.
- Adopt a “Listen First” Approach: Begin every conversation by assessing the patient’s existing beliefs, fears, and questions about generic drugs. Tailor the educational message to address their specific concerns.
- Systematically Use the Teach-Back Method: After explaining the rationale for a generic, ask the patient to explain it back in their own words. This simple step is the most effective way to ensure true comprehension and identify any lingering misunderstandings.
- Proactively Manage Change: For pharmacists, initiate counseling before a patient notices a change in their pill’s appearance. For physicians, inform patients during the prescribing process that they should expect to receive a generic version.
For Health System Administrators
Health system leaders have the power to create an environment where trust in generics is the default standard of care.
- Shift from Reactive to Proactive Education: Implement a strategic intelligence function to monitor drug patent expiry data. Launch timed, proactive communication campaigns that frame the arrival of a new generic as a planned, positive “upgrade” to a patient’s therapy.
- Invest in Provider Training: Develop and mandate training for all clinical staff not just on the science of bioequivalence, but on the evidence-based communication strategies and endorsement techniques required to build patient trust.
- Integrate Health Equity into Medication Education: Recognize that mistrust is highest in marginalized communities. Partner with community leaders and invest in culturally and linguistically appropriate services, including professional medical interpreters and translated materials, as a core component of care.
- Standardize the Message: Work to ensure that patients receive a consistent, reassuring message about generic drugs from every touchpoint within the system—from their primary care physician and specialist to the pharmacist and patient portal.
For Insurance Payers
Payers wield immense influence through benefit design and member communication, which can be optimized to build trust alongside driving value.
- Evolve Member Communication Beyond Cost and Logistics: Enhance formulary announcements and member communications to include clear, simple, and compelling content about the rigorous FDA approval process and the science of bioequivalence.
- Partner with Providers for a Unified Message: Co-develop educational materials with trusted provider groups and medical societies. A message co-branded by an insurer and a respected clinical organization is more powerful than one from the insurer alone.
- Innovate Benefit Design to Eliminate Barriers: Explore and expand innovative models that remove friction and anxiety, such as the $0 co-pay lists for essential generics pioneered by UnitedHealth Group, which completely eliminates cost as a factor in the decision.
For Policymakers and Regulators
Government bodies set the rules of the market and can foster an environment that promotes transparency, competition, and public confidence.
- Fund and Sustain Robust Public Education Campaigns: Support broad, long-term public awareness initiatives, like those from the FDA, to consistently disseminate accurate information and debunk common myths about generic drugs.
- Continue to Streamline and Support the Generic Approval Process: Ensure the FDA has the resources needed to conduct timely and rigorous reviews of generic drug applications, which promotes competition and lowers prices.
- Address Anti-Competitive Market Tactics: Examine and, where appropriate, enact policies to limit strategies—such as certain patent litigation tactics or “pay-for-delay” agreements—that are used to unnecessarily delay the entry of affordable generics into the market and sow patient confusion.
- Promote Cross-National Learning: Study and adapt successful policy levers from international models, such as the U.K.’s emphasis on generic prescribing and Australia’s use of active ingredient prescribing, to enhance domestic policy.
For Patient Advocacy Organizations
These organizations are crucial, independent voices that can bridge the gap between the healthcare system and the communities it serves.
- Serve as a Key Partner in Content Development: Collaborate with health systems, payers, and government agencies to create and vet educational materials, ensuring they are patient-centered, unbiased, and easy to understand.
- Advocate for Policies that Build System-Wide Trust: Champion initiatives that increase transparency in drug pricing, strengthen regulatory oversight, and promote health equity. A more trusted healthcare system is a prerequisite for more trusted medicines.
- Empower Patients with Knowledge: Develop and disseminate resources that teach patients how to ask good questions, how to read a prescription label, and how to be active, informed participants in decisions about their medications.
By working in concert, these stakeholders can dismantle the barriers of mistrust and misunderstanding, ensuring that all patients can confidently access the safe, effective, and affordable generic medicines they need to lead healthier lives.
Works cited
- Patients’ Perceptions Of Generic Medications: Although most Americans appreciate the cost-saving value of generics, few are eager to use generics themselves – PMC – National Institutes of Health (NIH) |, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2748784/
- Knowledge and perceptions of patients towards generic and local medications: The lebanese version – Pharmacia, accessed August 1, 2025, https://pharmacia.pensoft.net/article/98699/
- Do lower prices make generic medications the top choice for … – Tebra, accessed August 1, 2025, https://www.tebra.com/theintake/healthcare-reports/patient-treatment/generic-vs-name-brand
- Drug Brand Response and Its Impact on Compliance and Efficacy in Depression Patients, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5222824/
- Patient Perceptions of Generic Drugs: Dispelling Misconceptions – U.S. Pharmacist, accessed August 1, 2025, https://www.uspharmacist.com/article/patient-perceptions-of-generic-drugs-dispelling-misconceptions
- Preventing Chronic Disease | Perceptions of and Barriers to Use of …, accessed August 1, 2025, https://www.cdc.gov/pcd/issues/2012/12_0010.htm
- What do people really think of generic medicines? A systematic review and critical appraisal of literature on stakeholder perceptions of generic drugs – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4520280/
- What Do Users of Generic Medicines Think of Them? A Systematic Review of Consumers’ and Patients’ Perceptions of, and Experiences with, Generic Medicines – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/301793186_What_Do_Users_of_Generic_Medicines_Think_of_Them_A_Systematic_Review_of_Consumers’_and_Patients’_Perceptions_of_and_Experiences_with_Generic_Medicines
- Patient adherence – the key to restoring trust in pharma – pharmaphorum, accessed August 1, 2025, https://pharmaphorum.com/views-and-analysis/patient-adherence-the-key-to-restoring-trust-in-pharma
- Patient distrust in pharmaceutical companies: an explanation for women under-representation in respiratory clinical trials?, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7424561/
- Patients’ Trust in Their Physicians: Effects of Choice, Continuity, and Payment Method – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC1500897/
- Health Literacy and Medication Use | Pharmacotherapy: A Pathophysiologic Approach, 10e, accessed August 1, 2025, https://accesspharmacy.mhmedical.com/content.aspx?bookid=1861§ionid=146212356
- USP Health Literacy, accessed August 1, 2025, https://www.usp.org/healthcare-quality-safety/health-literacy
- Dispelling Generic Drug Myths and Misconceptions – U.S. Pharmacist, accessed August 1, 2025, https://www.uspharmacist.com/article/dispelling-generic-drug-myths-and-misconceptions
- Five strategies for providing effective patient education – Wolters Kluwer, accessed August 1, 2025, https://www.wolterskluwer.com/en/expert-insights/5-strategies-for-providing-effective-patient-education
- The Pros and Cons of Using Generic Drugs – UMass Memorial Health, accessed August 1, 2025, https://www.ummhealth.org/simply-well/the-pros-and-cons-of-using-generic-drugs
- Utilizing Generic Drug Awareness to Improve Patient Outcomes with Dr. Sarah Ibrahim | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/news-events-human-drugs/utilizing-generic-drug-awareness-improve-patient-outcomes-dr-sarah-ibrahim
- Improving Medication Adherence and Patient Experience by Researching Patient Perceptions of Generic Drugs | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/cder-conversations/improving-medication-adherence-and-patient-experience-researching-patient-perceptions-generic-drugs
- Generic Drugs, Overview & Basics – FDA, accessed August 1, 2025, https://www.fda.gov/drugs/generic-drugs/overview-basics
- About generics – Medicines UK, accessed August 1, 2025, https://www.medicinesuk.com/about-generics.php
- Generic Drugs: Your Questions Answered | CDA-AMC, accessed August 1, 2025, https://www.cda-amc.ca/generic-drugs-your-questions-answered
- Access to Generic Drugs in Canada, accessed August 1, 2025, https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/fact-sheets/access-to-generic-drugs.html
- Generic and hybrid medicines | European Medicines Agency (EMA) – European Union, accessed August 1, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/generic-hybrid-medicines
- Generic prescription medicines: Fact sheet | Therapeutic Goods Administration (TGA), accessed August 1, 2025, https://www.tga.gov.au/news/news/generic-prescription-medicines-fact-sheet
- A primer on generic drugs and bioequivalence – FDA, accessed August 1, 2025, https://www.fda.gov/files/about%20fda/published/Generic-Drugs-and-Bioequivalence—Presentation.pdf
- Generic Substitution Laws and Combination Products, accessed August 1, 2025, https://www.fdli.org/wp-content/uploads/2023/10/Pasha-Generic-Substitution-Laws-and-Combination-Products-FDLJ-78-2.pdf
- Generic medicines – homepage | Medicines for Europe, accessed August 1, 2025, https://www.medicinesforeurope.com/generic-medicines/
- Comparing FDA and EMA Decisions for Market Authorization of Generic Drug Applications covering 2017–2020, accessed August 1, 2025, https://www.fda.gov/media/156611/download
- Understanding Bioequivalence in Generic Drug Approval – Vici Health Sciences, accessed August 1, 2025, https://vicihealthsciences.com/what-is-bioequivalence/
- Similarities and Differences Between Brand Name and Generic Drugs | CDA-AMC, accessed August 1, 2025, https://www.cda-amc.ca/similarities-and-differences-between-brand-name-and-generic-drugs
- A review of the differences and similarities between generic drugs and their originator counterparts, including economic benefits associated with usage of generic medicines, using Ireland as a case study – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3579676/
- Tips for Talking With Your Pharmacist – Patient Advocate Foundation, accessed August 1, 2025, https://www.patientadvocate.org/wp-content/uploads/Tips-for-Talking-With-Your-Pharmacist-1.pdf
- Bioequivalence and Interchangeability of Generic Drugs – Merck Manuals, accessed August 1, 2025, https://www.merckmanuals.com/home/drugs/brand-name-and-generic-drugs/bioequivalence-and-interchangeability-of-generic-drugs
- What are generic medicines? | healthdirect, accessed August 1, 2025, https://www.healthdirect.gov.au/what-are-generic-medicines
- A Comparative Overview of Generic Drug Regulation in US, Europe, Australia and India, accessed August 1, 2025, https://www.ijdra.com/index.php/journal/article/download/747/396
- Generic medicine | European Medicines Agency (EMA) – European Union, accessed August 1, 2025, https://www.ema.europa.eu/en/glossary-terms/generic-medicine
- Influencers of Generic Drug Utilization: A Systematic Review – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5910277/
- Communication Strategies in Pharmacy – ACCP, accessed August 1, 2025, https://www.accp.com/docs/meetings/UT18/handouts/Communication_Strategies_in_Pharmacy_Supplemental_Chapter_PH.pdf
- Medications and doctor–patient communication – RACGP, accessed August 1, 2025, https://www1.racgp.org.au/ajgp/2021/october/medications-and-communication
- Go: Tips for Talking with Your Pharmacist to Learn How to Use Medicines Safely | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/tips-seniors/stop-learn-go-tips-talking-your-pharmacist-learn-how-use-medicines-safely
- epublications.marquette.edu, accessed August 1, 2025, https://epublications.marquette.edu/cgi/viewcontent.cgi?filename=0&article=1619&context=nursing_fac&type=additional#:~:text=The%20framework%2C%20rooted%20in%20the,%2C%20and%20teach%2Dback%20method.
- Educating Patients about Generic Drugs: Strategies for Success …, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/educating-patients-about-generic-drugs-strategies-for-success/
- Your Medicine: Be Smart. Be Safe. (with wallet card) | Agency for …, accessed August 1, 2025, https://www.ahrq.gov/es/health-literacy/patient-education/ask-your-doctor/your-meds.html
- Generic-Substitution Laws – U.S. Pharmacist, accessed August 1, 2025, https://www.uspharmacist.com/article/generic-substitution-laws
- Understanding Medication Adherence in Patients with Limited …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8765509/
- The impact of language barriers on patient care: a pharmacy perspective. | PSNet, accessed August 1, 2025, https://psnet.ahrq.gov/issue/impact-language-barriers-patient-care-pharmacy-perspective
- Multilingual Med Guides: Better Adherence – Harmoni, accessed August 1, 2025, https://www.harmonitranslate.com/blog/multilingual-medication-guides.html
- Full article: Development of a Patient-Centered Bilingual Prescription Drug Label, accessed August 1, 2025, https://www.tandfonline.com/doi/full/10.1080/10810730.2013.825664
- Factors influencing trust in doctors: a community segmentation strategy for quality improvement in healthcare | BMJ Open, accessed August 1, 2025, https://bmjopen.bmj.com/content/3/12/e004115
- Generic Drugs Can Help Promote Health Equity – FDA, accessed August 1, 2025, https://www.fda.gov/media/173765/download
- Generic Drugs | AMCP.org, accessed August 1, 2025, https://www.amcp.org/legislative-regulatory-position/generic-drugs
- – INCREASING GENERIC DRUG UTILIZATION: SAVING MONEY FOR PATIENTS – GovInfo, accessed August 1, 2025, https://www.govinfo.gov/content/pkg/CHRG-109hhrg21639/html/CHRG-109hhrg21639.htm
- A Comparative Case for Shifting US Generic Drug Policies to Increase Availability and Lower, accessed August 1, 2025, https://scholarlycommons.law.northwestern.edu/cgi/viewcontent.cgi?article=1903&context=njilb
- BCBS Patients Save Big with CivicaScript Generic Medications | Blue Cross Blue Shield, accessed August 1, 2025, https://www.bcbs.com/news-and-insights/article/blue-cross-blue-shield-save-patients-generic-drug
- Medicare Two Dollar Drug List Model – CMS, accessed August 1, 2025, https://www.cms.gov/priorities/innovation/innovation-models/medicare-two-dollar-drug-list-model
- Behaviour change interventions to promote prescribing of generic drugs: a rapid evidence synthesis and systematic review | BMJ Open, accessed August 1, 2025, https://bmjopen.bmj.com/content/4/5/e004623
- Comparing Generic Drug Markets in Europe and the United States: Prices, Volumes, and Spending | Milbank Quarterly, accessed August 1, 2025, https://www.milbank.org/quarterly/articles/comparing-generic-drug-markets-europe-united-states-prices-volumes-spending/
- REPORT – International Pricing and Canada’s Generic Prescription Medicines, accessed August 1, 2025, https://canadiangenerics.ca/wp-content/uploads/2023/12/CGPA_International-Pricing-and-Canadas-Generic-Prescription-Medicines-2023.pdf
- Prescription Drug Prices in Canada and the United States—Part 1 A Comparative Survey – Fraser Institute, accessed August 1, 2025, https://www.fraserinstitute.org/sites/default/files/PrescriptionDrugComparativeSurvey.pdf
- Generic Drug Sector Study – Competition Bureau Canada, accessed August 1, 2025, https://competition-bureau.canada.ca/en/generic-drug-sector-study
- Differences in generic drug prices between the US and Canada – PubMed, accessed August 1, 2025, https://pubmed.ncbi.nlm.nih.gov/18774867/
- An Overview on Comparative Study of Generic Drug Approval Process in USA, India and Australia – IJPPR, accessed August 1, 2025, https://ijppr.humanjournals.com/wp-content/uploads/2025/01/1.Parth-Raval1-Khyati-Patel2-Khushi-Patel2-Arpi-Patel2-Mrs-Mona-Gupta3-Ms.-Sandhya-Bodhe-.pdf
- Medicine price comparison between Australia and the United States, accessed August 1, 2025, https://australiainstitute.org.au/wp-content/uploads/2025/04/P1817-Medicine-price-comparison-between-Australia-and-US-web.pdf
- About prescriptions | Australian Government Department of Health, Disability and Ageing, accessed August 1, 2025, https://www.health.gov.au/topics/medicines/about-prescriptions
- Comparing Prescription Drugs in the US and Other Countries: Prices and Availability | HHS ASPE, accessed August 1, 2025, https://aspe.hhs.gov/sites/default/files/documents/d5541b529a379d1f908ed2f9c00a9255/aspe-cover-idr-pricing-availability.pdf
- Comparing Prescription Drugs in the U.S. and Other Countries: Prices and Availability, accessed August 1, 2025, https://aspe.hhs.gov/reports/comparing-prescription-drugs
- Navigating the Patent Cliff: Precision Print Campaigns for Pharma’s Evolving Landscape – RxJam, accessed August 1, 2025, https://rxjam.com/blog/navigating-the-patent-cliff-precision-print-campaigns-for-pharmas-evolving-landscape/
- Drug Patent Expirations and the “Patent Cliff” – U.S. Pharmacist, accessed August 1, 2025, https://www.uspharmacist.com/article/drug-patent-expirations-and-the-patent-cliff
- 5 Steps to Take When Your Drug Patent is About to Expire, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/5-steps-to-take-when-your-drug-patent-is-about-to-expire/
- Patent cliff and strategic switch: exploring strategic design possibilities in the pharmaceutical industry – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4899342/
- Thanks to DrugPatentWatch, we have optimized our workflow and saved on research costs, accessed August 1, 2025, https://www.drugpatentwatch.com/
- Patents and Exclusivity | FDA, accessed August 1, 2025, https://www.fda.gov/media/92548/download
- DrugPatentWatch | Software Reviews & Alternatives – Crozdesk, accessed August 1, 2025, https://crozdesk.com/software/drugpatentwatch
- Generic vs. Brand Name Drugs – Kaiser Permanente, accessed August 1, 2025, https://healthy.kaiserpermanente.org/learn/generic-vs-brand-name-drugs
- Common Pharmacy Questions | Kaiser Permanente, accessed August 1, 2025, https://healthy.kaiserpermanente.org/washington/get-care/additional-services/faq
- Generic drugs – Kaiser Permanente, accessed August 1, 2025, https://healthy.kaiserpermanente.org/northern-california/health-wellness/drug-formulary/generics
- Ascension joins other leading U.S. health systems to develop not-for-profit generic drug company, accessed August 1, 2025, https://about.ascension.org/news/2017/01/ascension-joins-other-leading-us-health-systems-to-develop-not-for-profit-generic-drug-company
- ASCENSION HEALTH, accessed August 1, 2025, https://mp.medimpact.com/brandcontentprovider/ASC/MP/current_formulary.pdf
- Pharmacy | Individual & Commercial Plans | Anthem, accessed August 1, 2025, https://www.anthem.com/provider/individual-commercial/pharmacy
- Your pharmacy benefits. – Cigna Healthcare, accessed August 1, 2025, https://www.cigna.com/static/www-cigna-com/docs/ifp/m-24-rx-all-967436-rx-benefits-overview-flyer-wag-advantage-markets.pdf
- Your pharmacy benefits. – Cigna Healthcare, accessed August 1, 2025, https://www.cigna.com/static/www-cigna-com/docs/ifp/m-25-rx-all-981602-rx-benefits-overview-flyer-cigna-90-now.pdf
- Pharmacy Coverage FAQs – Aetna, accessed August 1, 2025, https://www.aetna.com/faqs-health-insurance/pharmacy-faqs.html
- Prescription Drug Information & Resources | Aetna Medicare, accessed August 1, 2025, https://www.aetna.com/medicare/prescription-drugs/drug-information-resources.html
- 2025-Drug-guide-Aetna-Standard-Plan.pdf, accessed August 1, 2025, https://www.aetna.com/content/dam/aetna/pdfs/aetnacom/individuals-families-health-insurance/document-library/pharmacy/2025-Drug-guide-Aetna-Standard-Plan.pdf
- Prescription Drug Lists | Member resources | UnitedHealthcare, accessed August 1, 2025, https://www.uhc.com/member-resources/pharmacy-benefits/prescription-drug-lists
- Optum RX Transparency – UnitedHealth Group, accessed August 1, 2025, https://www.unitedhealthgroup.com/ns/orx-transparency.html
- Prescription Medications Covered by Your Health Plan | Cigna Healthcare, accessed August 1, 2025, https://www.cigna.com/individuals-families/member-guide/prescription-drug-lists/