Biologic drugs have ushered in a new era of therapeutic possibilities, revolutionizing the treatment landscape for a myriad of chronic and life-threatening conditions, from autoimmune diseases and cancers to diabetes. These advanced therapies, derived from living organisms, offer unparalleled efficacy and specificity, targeting underlying disease mechanisms with remarkable precision . However, this groundbreaking innovation comes with an undeniably steep price tag. The exorbitant cost of originator biologics presents a formidable barrier to access for countless patients globally and places a substantial financial strain on healthcare systems.
In response to this escalating cost crisis, biosimilars emerged as a beacon of hope. Conceived as more affordable, highly similar versions of these complex biologic drugs, biosimilars promise to introduce much-needed market competition, thereby driving down prices and expanding patient access. The underlying assumption is that as biosimilars gain traction, the economic benefits will cascade throughout the healthcare ecosystem, ultimately alleviating the financial burden on individual patients.
Yet, a critical question persists: while biosimilars demonstrably generate billions in system-wide healthcare savings, do these substantial reductions in overall spending genuinely translate into lower out-of-pocket costs for the patients who rely on these life-saving therapies? This report delves into this complex paradox, dissecting the intricate interplay of scientific, regulatory, economic, and policy factors that shape the biosimilar market. It aims to provide business professionals with a nuanced understanding of this landscape, equipping them with the knowledge to leverage market dynamics and intellectual property insights for strategic advantage in the evolving pharmaceutical and biotechnology industries.
The Biologic Revolution: A Double-Edged Sword of Innovation and Expense
Biologic drugs represent a pinnacle of modern pharmaceutical science, offering targeted and often life-changing treatments for conditions previously deemed untreatable or poorly managed. Their advent has transformed patient outcomes, providing hope where little existed. However, the very nature of these sophisticated therapies inherently contributes to their high cost, creating a significant challenge for healthcare systems worldwide.
Understanding Biologic Drugs: Complexity, Efficacy, and Inherent High Costs
At their core, biologics are not synthesized through traditional chemical reactions like small-molecule drugs. Instead, they are complex medications derived from natural and living sources, such as human, animal, or microorganism cells . This category encompasses a heterogeneous group of molecules, including proteins, antibodies, and vaccines, each with unique characteristics and mechanisms of action . For instance, monoclonal antibodies (mAbs) are highly specific molecules produced by genetically modified organisms in vivo, designed to target particular cells or proteins in the body .
The scientific and manufacturing complexities of biologics are profound. Unlike small molecules with well-defined chemical structures, biologics possess intricate three-dimensional conformations and often undergo post-translational modifications, such as glycosylation patterns, which critically influence their biological activity, safety, and potential to provoke an immune response . Even minor variations in the living systems used for their production or in the manufacturing conditions can lead to batch-to-batch variability, complicating product characterization and raising concerns about consistency . Key scientific and technical challenges in their development include ensuring structural complexity and heterogeneity, establishing product similarity and comparability across different batches or changes, assessing and mitigating immunogenicity (the potential to evoke anti-drug antibodies), and overcoming delivery and bioavailability issues, which often necessitate parenteral administration.
Manufacturing biologics involves a series of highly sensitive and complex “unit operations,” ranging from cell culture and expression to purification and formulation . Scaling up production from laboratory to commercial levels is notoriously difficult, as processes that work efficiently at a small scale may behave unpredictably when scaled up. Rigorous quality control and reproducibility are paramount to ensure batch-to-batch consistency, requiring advanced and often resource-intensive analytical techniques .
This extensive research and development (R&D), coupled with the long development timelines—often spanning 7 to 8 years and costing hundreds of millions of dollars—and the intricate, highly controlled manufacturing processes, are the primary drivers of the high cost of originator biologics . While biologics account for a mere 2% of all prescriptions, they command a disproportionate 37% of net drug spending in the United States. The annual cost for some biologic therapies can range from a few thousand to well over $100,000, particularly for treatments targeting severe conditions like certain cancers. This fundamental economic reality underscores the urgent need for more affordable alternatives.
The Promise of Biosimilars: A Pathway to Affordability and Access?
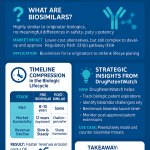
In this context, biosimilars emerged as a strategic response to the high cost of originator biologics. Biosimilars are not generic drugs in the traditional sense; they are highly similar versions of already approved reference biologics, with no clinically meaningful differences in terms of safety, purity, and potency . The distinction from generics is crucial: unlike chemically synthesized small-molecule generics that are identical copies of their reference products, biosimilars, being produced in living systems, cannot be exact replicas due to inherent natural variability . This fundamental difference shapes their regulatory pathway and market dynamics.
The overarching goal behind the development and introduction of biosimilars is clear: to provide more affordable treatment options as originator biologics lose patent protection . By stimulating market competition, biosimilars are intended to contribute to healthcare sustainability and expand patient access to vital therapies . The initial pricing strategy for biosimilars reflects this objective, with typical launch prices being 15% to 35% lower than their reference drugs . Some market analyses indicate even more substantial discounts, with the average sales price (ASP) for biosimilars often being around 50% less than the reference brand biologic’s price at the time of biosimilar launch .
The “highly similar, not identical” characteristic of biosimilars is a pivotal concept that underpins their regulatory pathway and, critically, public perception. This scientific nuance, while entirely acceptable from a clinical standpoint, creates unique challenges for market acceptance compared to the straightforward substitution of traditional generics. The rigorous regulatory pathway, based on a “totality of evidence” rather than full de novo clinical trials, aims to demonstrate this high similarity without compromising safety or efficacy . However, this distinction, though scientifically sound, can contribute to hesitancy among both healthcare providers and patients. This makes widespread adoption more challenging than for generics, despite the clear promise of cost savings, and highlights a complex interplay between scientific understanding, regulatory frameworks, and market dynamics.
Navigating the Regulatory Labyrinth: Paving the Way for Biosimilar Entry
The journey from scientific discovery to patient access for both originator biologics and their biosimilar counterparts is meticulously governed by stringent regulatory processes. These pathways, while designed to ensure safety, efficacy, and quality, also significantly influence market entry, competition, and ultimately, drug affordability.
Rigorous Pathways: FDA and EMA Approval Processes for Biologics and Biosimilars
Originator biologic drugs undergo an exhaustive approval process in the United States, culminating in a Biologics License Application (BLA) submitted to the Food and Drug Administration (FDA) . This submission requires comprehensive clinical data demonstrating the product’s safety, purity, and potency across all proposed indications . The BLA process involves extensive research, finalizing statistical analysis plans, conducting primary efficacy and comprehensive safety data analyses, and preparing integrated summaries of efficacy and safety. Similarly, the European Medicines Agency (EMA) evaluates applications for originator biologics based on a complete dossier of quality, pre-clinical, and clinical data .
Recognizing the immense cost and time associated with full BLAs, the Biologics Price Competition and Innovation Act (BPCIA) of 2009 established an abbreviated approval pathway for biosimilars in the U.S. . The intent was to reduce development time and cost without compromising the high standards of safety and effectiveness. The EMA, which pioneered biosimilar regulation in 2006, also employs a similar framework, establishing a solid foundation for biosimilar development globally.
The core of biosimilar approval, under both FDA and EMA, is the demonstration of “no clinically meaningful differences” from a reference product through a comprehensive “comparability exercise” . This approach, based on the “totality of evidence,” aims to avoid unnecessary repetition of costly and lengthy clinical trials that were already conducted for the reference product . The data typically required includes:
- Analytical Studies: These form the foundational component of biosimilar development, providing detailed data to support the structural and functional similarity of the proposed biosimilar to the reference product .
- Animal Studies: These may be required to provide toxicology or pharmacology information for the biosimilar, if deemed necessary by the regulatory agency .
- Clinical Pharmacology Studies: These studies demonstrate that the proposed biosimilar moves through the body in the same way (pharmacokinetics, PK) and produces the same effects (pharmacodynamics, PD) as the reference product. This often includes an immunogenicity assessment to evaluate a patient’s immune response .
- Additional Clinical Studies: While not always necessary, additional clinical studies may be conducted to address any remaining uncertainty about clinical similarity. However, the FDA and EMA have discretion to waive such studies for certain indications or populations if adequate scientific justification is provided, based on the comprehensive analytical and PK/PD data . The EMA, for instance, is actively proposing streamlined pathways that could reduce clinical data requirements, such as waiving comparative clinical efficacy studies, where strong analytical evidence exists .
The abbreviated pathway, while intended to speed market entry and lower costs, still demands significant investment and scientific rigor. This positions biosimilars in a unique regulatory space, distinct from both novel biologics and traditional generics. The development of a biosimilar typically costs between $100 million and $250 million and takes 7 to 8 years . This substantial barrier to entry, though less than for an originator biologic, is considerably higher than the $1 million to $4 million required for generic small-molecule drugs . This higher entry barrier ultimately limits the number of potential competitors in the biosimilar market compared to the generic market, which in turn influences the intensity and depth of price competition post-launch.
The Significance of Interchangeability: Streamlining Patient Access at the Pharmacy Level
Beyond demonstrating biosimilarity, a subset of biosimilars can achieve an “interchangeable” designation from the FDA. An interchangeable biosimilar meets additional, more stringent requirements, proving that switching between it and the reference product does not increase safety risks or decrease effectiveness, even with multiple switches .
This designation carries immense significance for streamlining patient access and enhancing market competition. Crucially, it allows pharmacists to substitute an interchangeable biosimilar for the reference product at the pharmacy level without requiring a new prescription or intervention from the prescribing physician, much like how generic drugs are routinely substituted for brand-name drugs . This automatic substitution capability is a powerful mechanism for driving uptake and competition, as it removes administrative hurdles and simplifies the prescribing and dispensing process. To achieve this, manufacturers typically conduct rigorous switching studies, where patients alternate between the reference product and the interchangeable biosimilar, to demonstrate comparable safety and efficacy .
However, the practical implementation of interchangeability is not uniform across the United States. While the FDA grants the designation, the actual ability of pharmacists to perform pharmacy-level substitution is subject to varying state pharmacy laws . Some states, for example, may require pharmacists to notify prescribers before dispensing a biosimilar or even mandate additional patient consent, adding administrative steps that can delay treatment and inadvertently discourage biosimilar use.
The concept of interchangeability represents a regulatory “holy grail” for biosimilars, as it allows them to truly mimic the efficiency of the generic market in driving down costs and increasing access. Yet, the slow pace of obtaining this status—only a few biosimilars have achieved it so far—and the persistent variability in state-level laws create a fragmented market that dilutes its full potential. The high cost and uncertain return on investment for manufacturers to pursue interchangeability, coupled with the patchwork of state laws, create a significant barrier to widespread adoption. This fragmentation and slow uptake mean that the market cannot fully leverage the “generic-like” substitution mechanism, thereby limiting the speed and depth of patient cost savings and overall market penetration. It highlights a policy-level disconnect between the intent of the BPCIA and the realities of real-world implementation.
The Economic Impact of Biosimilars: System-Wide Savings vs. Patient Realities
The introduction of biosimilars has undeniably created significant economic ripples throughout the healthcare system, leading to substantial savings for payers and a demonstrable reduction in drug prices. However, the critical question remains: how much of this economic benefit actually translates into lower out-of-pocket costs for the individual patient?
Driving Down List Prices: A Clear Win for Payers and Healthcare Systems
The overall economic impact of biosimilars on the U.S. healthcare system has been substantial. Biosimilars, alongside generics, generated a record $408 billion in savings for America’s patients, employers, and taxpayers in 2022, building on $373 billion in 2021 . Since their first entry in 2015, biosimilars alone have contributed $36 billion in savings, with projections indicating cumulative savings of $129 billion over five years by 2027 .
A key mechanism through which these savings are achieved is the competitive pressure biosimilars exert on the market. The introduction of biosimilars has consistently led to a reduction in the average sales price (ASP) of their corresponding brand biologics, with an average decline of 25% . Some studies have observed immediate and significant reductions in price per dose for originator biologics following biosimilar entry, such as a $438 reduction for trastuzumab, $112 for infliximab, and $110 for bevacizumab, with persistent further annual declines. Biosimilars themselves typically launch at a wholesale acquisition cost (WAC) that is 15% to 35% lower than their reference products . The ASP discounts for biosimilars can be even deeper, averaging around 50% less than the reference brand biologic price at the time of biosimilar launch .
This undeniable trend in price erosion for both biosimilars and their reference products represents a clear win for payers and healthcare systems, enabling them to manage budgets more effectively and potentially reallocate resources.
Case Studies in Price Erosion: Trastuzumab, Infliximab, and Adalimumab
Examining specific therapeutic areas reveals the varied impact of biosimilar competition:
- Trastuzumab (Herceptin): This oncology biologic is frequently cited as a prime example of biosimilars fulfilling their promise to reduce drug prices . When Kanjinti, the first trastuzumab biosimilar, entered the market, Herceptin’s average price dropped by approximately 21%. By the second quarter of 2022, the average sales prices for trastuzumab biosimilars ranged from 28% to 58% lower than Herceptin’s pre-competition ASP . The market demonstrated key hallmarks of competition: a choice among six products, rapid market share capture by new entrants, and steady price declines across all options. By Q3 2024, oncology biosimilars, including trastuzumab, held strong market shares, with trastuzumab biosimilars accounting for 86% of the market.
- Infliximab (Remicade): The infliximab biosimilar market share had increased to 48% by Q3 2024, with the average ASP for infliximab biosimilars decreasing by 7% by Q1 2025. However, early competition for infliximab was notably not linked to lower out-of-pocket costs for patients, despite the modest reductions in payer spending. This specific case highlights a critical divergence between system-level savings and direct patient benefit.
- Adalimumab (Humira): As the highest-expenditure medication worldwide in 2021, the entry of adalimumab biosimilars (e.g., Yusimry, launched at an 85% discount to branded Humira) was anticipated to drive significant cost savings for payers . Hypothetical models projected cumulative cost savings of millions for health plans depending on conversion rates from the reference product . Despite these deep discounts and the launch of multiple adalimumab biosimilars, they collectively achieved less than 2% of the market share versus brand biologics in 2023. This illustrates that price alone does not guarantee rapid or widespread uptake.
Broader Market Impact: Filgrastim, Pegfilgrastim, and Bevacizumab
The impact of biosimilars extends across various therapeutic areas, with mixed results in terms of market penetration and direct patient savings:
- Filgrastim & Pegfilgrastim: Biosimilars for filgrastim have achieved significant market share, reaching 77% by Q3 2020. For pegfilgrastim, studies in a commercially insured population showed that biosimilars led to 47-59% lower out-of-pocket costs for patients in the first cycle of treatment compared to the originator product . Interestingly, no significant difference in health plan costs was observed in these studies, as rebates and discounts were not considered in the analysis . This suggests that for some drugs, patient savings can be quite direct.
- Bevacizumab: The biosimilar bevacizumab market is projected for significant growth, driven by product innovation, aggressive pricing strategies, and strategic partnerships. In a real-world analysis, the use of bevacizumab-awwb in 2020 accounted for 34% of dispensed orders and resulted in savings of $166,894 for one institution, with potential for greater savings at higher adoption rates. The average sales price discounts for bevacizumab biosimilars averaged 49% in Q1 2025.
- Rituximab: Truxima, a rituximab biosimilar, launched in the U.S. at a 10% discount compared to the reference product’s list price. European studies indicate that the adoption of rituximab biosimilars could result in net budget savings ranging from €4.05 million to €303.86 million over five years, potentially extending treatment to thousands more patients.
While biosimilars undeniably reduce acquisition costs and system-wide spending (as reflected in ASP and WAC), their impact on market share and subsequent price erosion is highly variable across different molecules and therapeutic areas. This variability indicates that factors beyond just the availability of a biosimilar significantly influence its success and the depth of savings realized. The “clear win” for payers and healthcare systems in terms of price erosion is evident, but the realization of full potential savings through widespread adoption is not automatic and depends on overcoming non-price barriers, which will be explored further.
The Patient’s Perspective: Unpacking Out-of-Pocket Costs
The journey of a drug’s price from manufacturer to patient is fraught with complexities, often obscuring the direct impact of market competition on an individual’s financial burden. For patients, out-of-pocket (OOP) costs are a tangible and often prohibitive barrier to accessing necessary biologic therapies.
The components of OOP costs for patients typically include deductibles, coinsurance, and copayments . A deductible is the amount a patient must pay out of pocket before their health insurance begins to cover services. Coinsurance, often applied to high-cost specialty drugs like biologics, requires the patient to pay a fixed percentage of the drug’s cost after the deductible has been met . Copayments are typically flat fees paid per prescription. For expensive specialty drugs, coinsurance can result in substantial patient responsibility.
A critical disconnect exists: despite the billions in system-wide savings generated by biosimilars, studies consistently show that these savings often do not systematically translate into lower out-of-pocket spending for individual patients . A cohort study examining 7 clinician-administered biologics found that annual OOP spending did not decrease after biosimilar competition began, and importantly, OOP costs were similar for biosimilars and their reference biologics. For infliximab, early biosimilar competition was not linked to lower patient costs.
This phenomenon arises because patients with deductibles and coinsurance are particularly vulnerable to high list prices. Their OOP spending is correlated with increases in the drug’s list price, but they do not directly benefit from the confidential rebates paid by manufacturers to insurers. This suggests that while biosimilar competition might lower overall premiums for all patients by reducing system-wide costs, it may not significantly reduce the direct OOP costs for the specific patients who are actually taking these medications.
The complex interplay of insurance benefit design (high deductibles, coinsurance) and Pharmacy Benefit Manager (PBM) practices (rebate walls, copay accumulators) creates a systemic barrier that insulates patients from the direct price reductions achieved by biosimilars. This reveals a fundamental flaw in the current healthcare financing model that undermines the very purpose of biosimilar competition for affordability. The current financial architecture effectively creates a “firewall” between system-level savings and patient-level affordability, leading to non-adherence and worse health outcomes . This is a critical systemic issue, not merely a market inefficiency.
The role of Pharmacy Benefit Managers (PBMs) and the “rebate wall” phenomenon further exacerbates this issue. PBMs act as intermediaries, negotiating rebates with drug manufacturers in exchange for placing specific biologics or biosimilars on their formularies—the curated lists of medications covered by a health insurance plan . This system can create a perverse incentive: PBMs may prioritize higher-priced brand biologics that offer larger rebates, rather than lower-cost biosimilars, because the rebates contribute to their revenue . “Rebate walls” are a particularly insidious tactic where manufacturers condition the availability of their rebates on the exclusion of a lower-cost product from the formulary or on the PBM delivering sufficiently high market share to the higher-priced product. This effectively hinders biosimilar uptake and prevents patients from benefiting from the inherent cost savings . The lack of transparency and misaligned incentives in this PBM rebate system distort the marketplace, preventing the true economic benefits of biosimilars from reaching patients.
Adding another layer of complexity are copay accumulator and maximizer programs. Drug manufacturers frequently offer patient assistance programs (PAPs) and copay assistance programs (e.g., copay cards or coupons) to help commercially insured patients offset their high OOP costs for specialty drugs . These programs can provide significant relief, sometimes reducing a patient’s payment to as little as $0. However, health plans and PBMs are increasingly implementing “copay accumulator” and “copay maximizer” programs . With copay accumulators, the value of the manufacturer’s copay assistance does not count toward the patient’s deductible or out-of-pocket maximum. Once the coupon’s value is exhausted, the patient suddenly faces the full burden of their deductible and subsequent coinsurance or copayments, often unexpectedly . Copay maximizers, on the other hand, aim to capture the full value of the manufacturer’s coupon by setting the patient’s cost-sharing to match the maximum coupon value, spread evenly throughout the year. While this might lead to low immediate OOP costs, the coupon still does not count toward the patient’s deductible or OOP maximum. These programs, though intended to curb overall spending and pressure manufacturers to lower prices, effectively negate the intended benefit of manufacturer assistance for patients, leaving them vulnerable to substantial, unforeseen financial burdens.
Faced with these high and often unpredictable costs, patients frequently resort to cost-cutting strategies that can carry serious health risks. They may delay filling prescriptions, stretch out their doses to make them last longer, or seek alternative, potentially less effective, over-the-counter medications . These actions can lead to non-adherence, disease progression, and ultimately, worse health outcomes, highlighting the profound human impact of the disconnect between system-level savings and individual patient affordability .
| Metric | System-Wide Impact (Payer/Healthcare System) | Patient Out-of-Pocket Cost Impact |
| Overall Savings from Biosimilars | $408 billion in 2022 (generics & biosimilars combined) | Often no systematic decrease observed |
| $36 billion since first biosimilar entry in 2015 | OOP costs often similar for biosimilars and reference biologics | |
| Average Sales Price (ASP) Reduction | Biosimilars: ~50% lower than reference brand biologic at launch | Patients with deductibles/coinsurance do not directly benefit from rebates influencing ASP |
| Originator Biologics: ~25% average reduction due to biosimilar competition | Patient OOP correlated with list prices, not net prices after rebates | |
| Specific Drug Examples | Trastuzumab: Reference price dropped ~21% upon biosimilar entry | Infliximab: Early biosimilar competition not linked to lower patient OOP costs |
| Bevacizumab: Institution saved $166,894 in 2020 with 34% biosimilar use | Pegfilgrastim: 47-59% lower OOP costs for patients in commercially insured population |
Table 1: The Disconnect: System Savings vs. Patient Out-of-Pocket Costs
This table visually highlights the core paradox of the biosimilar market. It succinctly presents quantitative evidence for system-level savings alongside the qualitative and quantitative evidence for the often-absent patient-level savings. By juxtaposing these figures, it immediately reinforces the “disconnect” for the reader, making the central argument more tangible and impactful. For business professionals, this comparison quickly illuminates the scale of system savings and the persistent challenge at the patient level, prompting them to consider strategies that bridge this critical gap.
Barriers to Widespread Biosimilar Adoption: A Complex Web of Challenges
Despite their clear potential to reduce healthcare costs and expand patient access, biosimilars face a formidable array of barriers that impede their widespread adoption. These challenges are not singular but rather form a complex, interconnected web spanning legal, economic, and behavioral domains.
Intellectual Property and Patent Thickets: The Legal Minefield Delaying Market Entry
Intellectual property (IP) rights, primarily patents and data exclusivity periods, are fundamental to the pharmaceutical industry. They serve as a crucial incentive for innovators to invest billions in the discovery and development of novel biologics, ensuring a return on their immense R&D investments . However, this very protection, while vital for innovation, simultaneously creates significant barriers for biosimilar entry, thereby delaying competition and directly influencing pricing and patient access.
A particularly challenging aspect is the “patent thicket.” Originator companies often amass vast portfolios of overlapping patents around a single blockbuster product . These patents can cover various aspects, including the core molecular structure, specific formulations, manufacturing processes, methods of use, and even ancillary technologies or delivery systems . This “thicket” is a deliberate and effective strategy designed to deter or delay biosimilar developers, making it exceedingly difficult for them to enter the market without infringing on existing patent rights . A prominent example is Humira (adalimumab), which, despite completing its initial exclusivity period in 2014, was protected by over 200 patents, many filed after this date, effectively delaying biosimilar launch until 2023.
The Biologics Price Competition and Innovation Act (BPCIA) in the U.S. introduced a “patent dance” procedure, intended to facilitate the early resolution of patent disputes. However, in practice, biosimilar manufacturers frequently encounter extensive and protracted patent litigation, which significantly increases their development costs and delays market entry . Unlike generic small-molecule drug manufacturers who can initiate patent litigation much earlier in their development process, biosimilar firms generally cannot initiate litigation under the BPCIA until after completing costly Phase 3 clinical trials . This timing disparity gives originator companies a strategic advantage, allowing them to extend their monopolies and delay biosimilar entry by approximately 1.8 years on average . This legal complexity adds substantial financial risk and time to biosimilar development, directly impacting their ability to deliver timely cost savings to patients.
Navigating this complex patent landscape requires sophisticated tools and expertise. DrugPatentWatch offers critical insights by providing comprehensive data on patent lifecycles, litigation trends, and market exclusivity periods . By analyzing patent family size, forward citations (indicating patent influence), and claim breadth (the scope of protection), companies can identify undervalued assets, anticipate generic and biosimilar competition, and mitigate risks. This intelligence is vital for strategic R&D investment decisions and for developing effective market entry plans for biosimilars . The current legal and IP environment, while intended to balance innovation and competition, has inadvertently become a potent tool for originators to extend monopolies and delay biosimilar entry, directly impacting patient access and affordability for longer than necessary.
Healthcare System Dynamics: Formulary Decisions, Reimbursement Models, and Provider Incentives
Beyond the legal complexities, the intricate financial and operational dynamics of the healthcare system itself pose significant barriers to biosimilar adoption. Pharmacy Benefit Managers (PBMs) play a pivotal role in determining drug access and pricing through their formulary decisions. Many PBMs either exclude biosimilars from their formularies, place them on higher tiers that result in greater out-of-pocket costs for patients, or list them at parity with higher-cost reference products without providing the necessary incentives for patients to switch . This directly impacts patient access and the realization of potential cost savings at the point of care .
Reimbursement models further complicate the picture. Inadequate reimbursement for biosimilars, particularly under the complex cost-sharing structures of Medicare Part D, can lead to a perverse situation where physicians may actually lose money when administering these treatments. This financial disincentive can make healthcare providers reluctant to prescribe biosimilars, even if they are clinically appropriate and offer lower list prices.
The current system often creates misaligned incentives, favoring higher-list-price biologics due to the larger rebates they generate for PBMs and payers. This has been described as a “formulary construction crisis,” where payer-driven incentives prevent the inclusion of potentially lower-cost medicines, including biosimilars. Policies that tie provider reimbursement to the acquisition price of biologics can also inadvertently disincentivize the use of lower-cost options, as providers may rely on margins from higher-priced drugs for revenue.
The Inflation Reduction Act (IRA) of 2022, while aiming to lower drug costs through government price negotiations, introduces another layer of complexity. While well-intentioned, the IRA’s provisions may have unintended consequences, potentially deterring manufacturers from launching biosimilars, especially for high-sales biologics . This “chilling effect” could lead to substantial lost annual savings—potentially billions of dollars—if biosimilar entry is delayed or curtailed due to pricing uncertainty .
The current healthcare system’s financial architecture, particularly PBM practices and reimbursement models, creates a “pull” towards higher-cost originator biologics, effectively neutralizing the price advantage of biosimilars at multiple levels. This systemic inertia is a more potent barrier than initial price differences alone. The complex interplay of PBM rebates, formulary design, and provider reimbursement creates a system where financial incentives are misaligned, favoring the entrenched, higher-priced originator products. This creates a “rebate wall” and a lack of “gainsharing” at the provider level, meaning that even when biosimilars are approved and available at lower prices, the economic ecosystem of healthcare often prevents those savings from being realized or passed on to patients, leading to lower uptake and persistent high costs. The IRA, while well-intentioned, could exacerbate this by further disincentivizing biosimilar development.
Bridging the Knowledge Gap: Addressing Physician and Patient Hesitancy
Beyond economic and regulatory hurdles, a significant psychological and informational barrier exists that directly impacts biosimilar adoption. Many healthcare professionals (HCPs), including physicians and pharmacists, initially express hesitancy to adopt biosimilars. This stems from concerns about perceived structural differences from reference products, potential impacts on safety and efficacy, and uncertainty surrounding interchangeability. Studies have revealed that a notable percentage of physicians (2-25%) may not accurately define biosimilars, and a significant majority (65-67%) harbor concerns about prescribing them. HCPs also face practical administrative burdens, such as navigating prior authorizations or step therapy requirements, which can further deter biosimilar prescribing.
Patients, too, often exhibit a lack of strong knowledge about biosimilars; one study indicated that only 21% of patients reported having a strong understanding. They may be reluctant to switch from a stable, familiar biologic, often fearing a compromise in efficacy or safety. The common comparison of biosimilars to “generics” can be confusing for both patients and providers, as biosimilars are not identical copies, leading to questions about their true nature and safety. Misinformation surrounding biosimilars can also play a role in fostering distrust.
To overcome this, comprehensive education is vital for both healthcare providers and patients . Educational initiatives should cover general information about biosimilars, their rigorous approval processes, comparable safety and efficacy data relative to reference products, and the precise meaning of interchangeability . Pharmacists are uniquely positioned to serve as key educators, providing crucial information and addressing concerns at the point of care for both prescribers and patients . For patients, framing biosimilars positively and emphasizing benefits such as providing additional treatment options during drug shortages (a benefit patients themselves identified as important) can significantly improve acceptance .
The lack of comprehensive, consistent education fosters misconceptions and distrust, which directly translates into lower adoption rates, regardless of price or regulatory approval. Investing in education is therefore a strategic imperative. It is not merely about informing, but about building confidence and overcoming psychological barriers that prevent patients from benefiting from lower-cost options. This also empowers patients to advocate for themselves, fostering informed decision-making.
| Barrier Category | Specific Examples and Data Points | Impact on Adoption & Patient Costs |
| Intellectual Property & Legal | – Patent Thickets: Originator companies amass 100s of patents (e.g., Humira with 200+), many filed after initial exclusivity, to delay competition . | Delays biosimilar market entry (avg. 1.8 years) , prolonging high prices for patients. Increases development costs for biosimilars. |
| – “Patent Dance” & Litigation: Biosimilar firms can only initiate litigation after costly Phase 3 trials . | Adds significant financial risk and time to biosimilar development, limiting new entrants. | |
| Healthcare System Dynamics | – PBM Formulary Practices: Exclusion, higher tiers, or parity pricing without incentives for biosimilars . | Prevents lower biosimilar prices from translating into patient savings; patients face higher OOP or no access to cheaper options . |
| – “Rebate Walls”: Originators condition rebates on PBMs excluding lower-cost biosimilars or ensuring high market share for brand. | Actively hinders biosimilar uptake and competition, maintaining high drug costs. | |
| – Reimbursement Models: Inadequate Medicare Part D reimbursement can make biosimilars financially unviable for providers . | Disincentivizes providers from prescribing biosimilars, limiting patient access . | |
| – Copay Accumulator/Maximizer Programs: Manufacturer patient assistance doesn’t count towards patient deductible/OOP max . | Negates manufacturer assistance, leaving patients with unexpected, substantial financial burdens. | |
| – Inflation Reduction Act (IRA): Government price negotiations may “chill” biosimilar development . | Could lead to lost future savings and delayed competition, impacting long-term affordability . | |
| Provider & Patient Hesitancy | – Physician Knowledge Gaps: 2-25% don’t know biosimilar definition; 65-67% have concerns about prescribing. | Leads to reluctance to prescribe biosimilars, maintaining reliance on higher-cost originators . |
| – Patient Knowledge Gaps: Only 21% report strong biosimilar knowledge; reluctance to switch from stable biologics . | Limits patient acceptance and willingness to switch, even for cost savings. | |
| – Administrative Hurdles: Prior authorizations, step therapy, varying state substitution laws. | Adds complexity and delays, discouraging biosimilar use. |
Table 2: Multifaceted Barriers to Biosimilar Adoption
This table provides a structured overview of the complex and interconnected barriers to biosimilar adoption. By categorizing these challenges into legal/IP, healthcare system, and provider/patient factors, it helps deconstruct a complex problem into manageable components. The table’s comprehensiveness ensures that all major barriers identified in the available information are presented, demonstrating a holistic understanding. For business professionals, this serves as a valuable tool to identify specific areas where targeted interventions—such as legal strategies, PBM engagement, or educational campaigns—are needed to improve biosimilar uptake and, critically, patient access and affordability.
Unlocking the Full Potential: Strategies for Enhancing Patient Affordability
Realizing the full promise of biosimilars—not just for system-wide savings but for tangible reductions in patient out-of-pocket costs—requires a concerted, multi-pronged approach. This involves strategic policy interventions, robust educational initiatives, and a commitment to fostering true market competition.
Policy Interventions: Realigning Incentives for Direct Patient Benefit
Effective policy interventions are not merely about setting prices; they are about fundamentally reshaping the incentive structures within the healthcare system to ensure that system-wide savings are meaningfully passed on to patients. This necessitates a shift from a rebate-driven model to one that directly rewards the adoption of lower-cost alternatives.
A primary area for reform lies with Pharmacy Benefit Managers (PBMs). Policymakers should focus on increasing transparency in PBM practices and eliminating “rebate walls” that currently favor high-list-price drugs offering larger rebates . This includes encouraging PBMs to place biosimilars on favorable formulary tiers and implementing incentives for patients to switch to these more affordable options. Such reforms would help dismantle the financial “firewall” that prevents biosimilar savings from reaching patients.
Adjustments to Medicare Part D and the Inflation Reduction Act (IRA) are also critical. While the IRA introduced a welcome $2,000 yearly limit on Medicare Part D out-of-pocket costs, further targeted reforms are needed to prevent its government price negotiations from inadvertently chilling biosimilar development . For instance, automatically granting a two-year delay in price setting when a biosimilar is set to launch could mitigate this “chilling effect” and protect the biosimilar pipeline.
Reforming reimbursement models, particularly within Medicare Part B, is another vital step. Shifting away from the traditional “buy-and-bill” system towards market-based reforms, such as competitive bidding or blended reimbursement rates (e.g., a 106% “blended” average sales price for both originator and biosimilar), can spur head-to-head price competition and directly incentivize the use of lower-cost options. This approach would ensure that providers are financially encouraged, rather than penalized, for prescribing biosimilars.
Finally, promoting interchangeability is paramount. Policies that simplify biosimilar substitution at the pharmacy level, through clear and consistent interchangeability laws across all states, are crucial for streamlining patient access and maximizing uptake . Such measures would allow the market to function more efficiently, delivering the full economic benefits of biosimilars directly to patients. These policy changes are critical for creating an environment where the economic benefits of biosimilars are fully realized by patients, moving beyond theoretical savings to tangible affordability.
Fostering Education and Awareness: Empowering Patients and Providers for Informed Choices
Beyond economic and regulatory changes, addressing the knowledge gap and building trust among stakeholders is fundamental to increasing biosimilar adoption. Education is not a standalone solution but a crucial enabler that unlocks the potential of economic and regulatory reforms. Without trust and understanding, even the most affordable and accessible biosimilar may face resistance, highlighting the human element in market adoption.
Comprehensive, targeted education initiatives are vital to address existing knowledge gaps and build confidence among healthcare providers (physicians, pharmacists) and patients . The content of these educational programs should be clear, concise, and evidence-based, covering essential information about biosimilars, their rigorous approval processes, and their comparable safety and efficacy to reference products . Explaining the concept of interchangeability and its implications for patient choice and convenience is also crucial .
Pharmacists, in particular, are uniquely positioned to serve as frontline educators. They can provide critical information to both prescribers and patients, addressing concerns and clarifying misconceptions at the point of care . Equipping pharmacists with readily accessible, simplified resources on biosimilar information, including state-specific substitution laws, can significantly facilitate their role.
For patients, the framing of biosimilars is important. Rather than focusing solely on cost, emphasizing benefits such as providing additional treatment options, especially during drug shortages—a benefit patients themselves identified as important—can foster greater acceptance . Positive communication about the safety and efficacy of biosimilars, supported by real-world evidence, can help overcome psychological barriers and reluctance to switch from familiar originator biologics. Investing in education is a strategic imperative because it is not just about informing, but about building confidence and overcoming psychological barriers that prevent patients from benefiting from lower-cost options. This also empowers patients to advocate for themselves, fostering informed decision-making.
Promoting True Competition: Beyond Initial Price Reductions to Sustainable Access
True competition in the biosimilar market extends beyond simply having multiple products available. It requires a dynamic interplay of legal reforms, manufacturing innovation, robust data generation, and strategic market intelligence to ensure sustainable supply and continuous price pressure that ultimately benefits patients.
Addressing patent barriers is a critical first step. Reforms to the patent litigation framework, such as allowing biosimilar manufacturers to initiate patent litigation earlier—for instance, at the start of Phase 3 clinical trials—could significantly reduce market entry delays, potentially by nearly two years . This would enable biosimilar firms to resolve patent issues well before the brand biologic’s primary patent expiration date, accelerating the availability of more affordable options.
Biosimilar manufacturers must continue to innovate in their manufacturing processes to achieve greater cost-effectiveness and ensure supply reliability . Technological improvements, such as the development of single-use or disposable technologies, can reduce capital costs and enhance efficiency. Forming strategic partnerships with other biosimilar developers, research institutions, or even originator companies can also expedite market entry and reduce litigation costs by sharing resources and expertise.
Generating robust real-world evidence (RWE) is essential for building confidence among all stakeholders. RWE on the long-term safety, efficacy, and cost-effectiveness of biosimilars can provide valuable insights that complement clinical trial data, further validating their use and informing decision-making at both clinical and policy levels . RWE can also play a crucial role in supporting biosimilar interchangeability designations in the U.S. .
Manufacturer-sponsored patient assistance programs (PAPs) remain a vital safety net for commercially insured patients, helping them manage the often-prohibitive out-of-pocket costs associated with specialty drugs . However, these programs must be protected from the adverse impact of copay accumulator and maximizer programs, which undermine their effectiveness in providing direct patient relief.
Finally, leveraging competitive intelligence (CI) tools and strategies is crucial for companies operating in this dynamic landscape . Tools like DrugPatentWatch provide critical data on patent lifecycles, litigation trends, and market exclusivity periods, enabling companies to anticipate competitor moves, identify market opportunities, and refine their R&D and market access strategies . CI helps companies stay ahead of regulatory changes, optimize pricing strategies, and ensure a sustainable market presence . By systematically incorporating patent analytics into their decision frameworks, pharmaceutical investors can gain strategic advantages, including early identification of undervalued assets, risk mitigation through probabilistic modeling of litigation and regulatory outcomes, and alpha generation by anticipating market shifts from patent cliffs and genericization waves.
The ultimate success of biosimilars in reducing patient out-of-pocket costs hinges on a paradigm shift from a fragmented, adversarial market to a collaborative ecosystem where all stakeholders are incentivized to prioritize patient access and affordability. This requires sustained political will and industry commitment. A truly competitive market is not just about more biosimilars, but effective biosimilars that can overcome systemic barriers. This leads to sustained price reductions and, critically, improved patient access and affordability over the long term.
The Future Landscape: A Vision for Accessible Biologic Therapies
The biosimilar market is at a pivotal juncture, poised for significant growth while simultaneously grappling with persistent challenges that will shape its ability to deliver on the promise of accessible biologic therapies.
Emerging Trends and Market Projections: Continued Growth and Challenges
Projections for the global biosimilar market are robust, with valuations expected to reach $72.29 billion by 2035 (at a compound annual growth rate, CAGR, of 7.5%) or even $175.79 billion by 2034 (at a CAGR of 17.6%) . This impressive growth trajectory is primarily driven by the impending patent expirations of numerous blockbuster biologics and the ever-increasing global demand for more affordable alternatives to expensive originator therapies .
Biosimilars are also expanding their therapeutic footprint beyond the initial focus on oncology and autoimmune diseases. They are now targeting areas such as ophthalmology, endocrinology, and rare diseases, broadening the scope of conditions for which more affordable options are available. Oncology biosimilars, in particular, have demonstrated strong market shares, with trastuzumab biosimilars holding 86% and bevacizumab biosimilars holding 90% of their respective markets by Q3 2024.
Despite these positive trends and growth projections, significant challenges persist. Manufacturing complexities and the high costs associated with biosimilar development remain formidable barriers to entry, particularly for smaller firms. Intense market competition, coupled with pricing pressure among existing players, can also restrain market growth and sustainability. Furthermore, the potential “chilling effect” of government price negotiations under the Inflation Reduction Act (IRA) on future biosimilar development remains a considerable concern, as it could deter manufacturers from investing in new biosimilar programs, especially for high-sales biologics . In 2023, despite offering price discounts greater than 80%, biosimilar versions of the best-selling biologic Humira collectively achieved less than two percent of the market versus brand biologics. This highlights that while the market will expand, its full potential for patient affordability is not guaranteed and requires ongoing, concerted effort.
The future of biosimilars is a complex interplay of strong growth drivers (patent cliffs, demand) and persistent headwinds (regulatory uncertainty, PBM practices, intellectual property challenges). This suggests that while the market will expand, its full potential for patient affordability is not guaranteed and requires ongoing, concerted effort. The rate and depth of patient benefit will depend on how effectively these systemic barriers are addressed through policy, industry innovation, and education.
Collaborative Pathways for Sustainable Affordability and Patient Access
Maximizing the benefits of biosimilars—ensuring they deliver not only system-wide savings but also tangible reductions in patient out-of-pocket costs—requires a fundamental shift towards multi-stakeholder cooperation. This collaborative approach must involve regulators, developers, payers, providers, and patients working in concert .
Policymakers face the delicate task of balancing aggressive cost containment measures with strategies that actively promote biosimilar competition and development . This means crafting policies that foster a vibrant biosimilar market without inadvertently stifling innovation or discouraging new entrants. A patient-centric approach should guide all policy decisions, positioning biosimilars as a crucial solution to expand access, improve patient outcomes, and ensure supply continuity .
Industry leadership is equally vital. Pharmaceutical and biotechnology companies must continue to invest in R&D, enhance manufacturing efficiencies, and develop robust market access strategies to ensure a sustainable biosimilar pipeline . This includes exploring innovative pricing models and patient support programs that directly benefit individuals.
As John Murphy III, President and CEO of the Association for Accessible Medicines, aptly states, “The better option is the proven success of reducing drug prices through generic and biosimilar competition”. This sentiment underscores the collective responsibility to create an environment where biosimilars can thrive and truly deliver on their promise. The vision of accessible biologic therapies is achievable, but it is a shared responsibility. It is not just about biosimilars existing, but about creating an ecosystem where they can flourish and provide meaningful benefits for every patient who needs them.
Key Takeaways
The advent of biosimilars has introduced a dynamic force into the pharmaceutical landscape, undeniably reshaping the economics of high-cost biologic therapies. The analysis reveals several critical points for business professionals navigating this evolving market:
- System-Wide Savings are Real and Substantial: Biosimilar competition demonstrably reduces overall healthcare system spending and the average sales prices of both biosimilars and their reference products. This has led to billions in savings for payers, employers, and taxpayers, demonstrating the significant economic value biosimilars bring to the healthcare system.
- Patient Out-of-Pocket Costs Remain a Persistent Challenge: Despite these significant system-level savings, the evidence indicates that these benefits often do not consistently translate into lower out-of-pocket costs for individual patients. This is largely due to complex insurance designs (high deductibles, coinsurance on list prices), opaque PBM practices (rebate walls, formulary tiering that favors high-rebate products), and the detrimental impact of copay accumulator and maximizer programs that negate manufacturer patient assistance.
- Multifaceted Barriers Impede Widespread Adoption: The full potential of biosimilars is hindered by a complex web of challenges. These include protracted patent litigation and “patent thickets” that delay market entry, misaligned financial incentives within the healthcare system that favor originator biologics, and critical knowledge gaps and hesitancy among both healthcare providers and patients regarding biosimilar safety and efficacy.
- Unlocking Patient Affordability Requires Comprehensive Intervention: To ensure that biosimilar competition truly benefits patients directly, a multi-faceted approach is essential:
- Policy Reforms: Implementing greater transparency in PBM practices, adjusting IRA provisions to protect biosimilar development, and reforming reimbursement models to incentivize the use of lower-cost biosimilars.
- Education and Awareness: Launching comprehensive, targeted educational programs for providers and patients to build trust, address misconceptions, and foster informed decision-making.
- Market Optimization: Streamlining patent challenges, fostering continuous manufacturing innovation, generating robust real-world evidence to build confidence, and strategically leveraging competitive intelligence tools (such as those offered by DrugPatentWatch) to navigate market dynamics and ensure a sustainable and truly competitive biosimilar market.
- Collaboration is Key to the Future: The vision of accessible biologic therapies hinges on sustained collaboration among all stakeholders—regulators, developers, payers, providers, and patients. By aligning incentives and fostering a patient-centric approach, the healthcare ecosystem can ensure that the economic benefits of biosimilars are fully realized by the patients who need them most, driving both health equity and economic sustainability.
“Transitioning patients in British Columbia, Alberta, and New Brunswick has saved more than $100M since the process started in 2019. This has been done with no adverse health effects for those receiving these agents. These governments have reinvested the money in improving health care particularly for those with arthritis. This has been a big win for both health care and for arthritis patients.”
Frequently Asked Questions (FAQs)
Q1: How are biosimilars different from generic drugs, and why does this matter for patient costs?
A: Generic drugs are identical chemical copies of small-molecule drugs, making their development and regulatory approval relatively straightforward. This typically leads to rapid and deep price erosion upon market entry. Biosimilars, however, are large, complex biological products derived from living systems. While they are “highly similar” to their reference biologics and have no clinically meaningful differences in safety, purity, and potency, they are not identical copies due to the inherent variability of biological production. This complexity necessitates a more rigorous, albeit abbreviated, regulatory approval pathway and significantly higher development costs than generics. This distinction impacts the speed of market entry, the intensity of price competition, and can contribute to physician and patient hesitancy, all of which can influence how quickly and significantly patient out-of-pocket costs decrease.
Q2: Why do healthcare system savings from biosimilars not always reach the patient?
A: The primary reason for this disconnect lies in the intricate interplay of insurance benefit designs and Pharmacy Benefit Manager (PBM) practices. Many patients face high deductibles and coinsurance, meaning their out-of-pocket costs are often calculated as a percentage of the drug’s list price, not the lower net price after confidential rebates. PBMs frequently prioritize rebates negotiated with originator biologic manufacturers, which can lead to biosimilars being placed on less favorable formulary tiers or even excluded, despite their lower list prices. Additionally, “copay accumulator” and “maximizer” programs prevent manufacturer-provided patient assistance from counting towards a patient’s deductible or out-of-pocket maximum, leaving patients exposed to the full cost once the assistance is exhausted. These systemic factors create a barrier that prevents the full economic benefits of biosimilars from directly reaching patients.
Q3: What role do “patent thickets” play in delaying biosimilar market entry and impacting costs?
A: “Patent thickets” refer to the dense, overlapping portfolios of patents (covering the molecule, formulation, manufacturing processes, and even administration devices) that originator companies create around their blockbuster biologics. This strategy aims to extend market exclusivity beyond the primary patent expiration. For biosimilar manufacturers, navigating these thickets involves costly and protracted patent litigation, which often cannot be initiated until after extensive and expensive Phase 3 clinical trials are completed. This legal minefield significantly delays biosimilar market entry, potentially by years, thereby prolonging the period of high-cost originator monopoly and limiting the timely introduction of more affordable options for patients.
Q4: How can policy changes and education help lower patient out-of-pocket costs for biologics?
A: Policy interventions are crucial for realigning financial incentives within the healthcare system. This includes reforming PBM practices to increase transparency and prevent “rebate walls” that favor high-rebate products, adjusting government price negotiation policies (such as those under the IRA) to avoid chilling biosimilar development, and implementing reimbursement models that directly incentivize the use of lower-cost biosimilars. Complementing these policy changes, comprehensive and targeted education for healthcare providers and patients is essential. By addressing misconceptions about biosimilar safety and efficacy, and by clearly communicating their benefits and the concept of interchangeability, education can build trust and encourage greater adoption, ultimately translating system-wide savings into tangible patient affordability.
Q5: What is the significance of “interchangeability” for biosimilars, and why is it not more widespread?
A: Interchangeability is a regulatory designation granted by the FDA that allows a pharmacist to substitute an interchangeable biosimilar for its reference product without the need for a new prescription, similar to how generic drugs are routinely substituted. This designation is highly significant because it can streamline patient access and dramatically increase biosimilar uptake, thereby intensifying price competition in the market. However, achieving interchangeability requires manufacturers to conduct additional, costly switching studies to demonstrate that alternating between the biosimilar and reference product does not diminish safety or effectiveness. Furthermore, the actual ability to substitute at the pharmacy level varies by state law. The substantial investment required for manufacturers and the fragmented regulatory landscape across states have limited the number of biosimilars that have achieved this status, hindering the full realization of its potential benefits for patient affordability.
References |
Works cited
- What are the common challenges in biologic drug development? – Patsnap Synapse, accessed July 17, 2025, https://synapse.patsnap.com/article/what-are-the-common-challenges-in-biologic-drug-development
- Manufacturing of Biologics – ResearchGate, accessed July 17, 2025, https://www.researchgate.net/publication/322212686_Manufacturing_of_Biologics
- Biosimilars: Regulatory Trends and Manufacturing Considerations – Sigma-Aldrich, accessed July 17, 2025, https://www.sigmaaldrich.com/deepweb/assets/sigmaaldrich/product/documents/990/152/biosimilars-white-paper-en-feb-2017-low-mk.pdf
- An Overview of Biosimilars—Development, Quality, Regulatory Issues, and Management in Healthcare – ResearchGate, accessed July 17, 2025, https://www.researchgate.net/publication/378041576_An_Overview_of_Biosimilars-Development_Quality_Regulatory_Issues_and_Management_in_Healthcare
- The Biologics License Application (BLA) Process Explained – The FDA Group, accessed July 17, 2025, https://www.thefdagroup.com/blog/2014/07/test-the-biologics-license-application-bla-process/
- The Real Cost of Biologic Drugs, accessed July 17, 2025, https://biologicmeds.org/biologic-basics/the-real-cost-of-biologic-drugs/
- The Economics of Biosimilars – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4031732/
- Biosimilars Market Growth, Drivers, and Opportunities – MarketsandMarkets, accessed July 17, 2025, https://www.marketsandmarkets.com/Market-Reports/biosimilars-40.html
- Review and Approval – FDA, accessed July 17, 2025, https://www.fda.gov/drugs/biosimilars/review-and-approval
- Biosimilar Product Regulatory Review and Approval | FDA, accessed July 17, 2025, https://www.fda.gov/files/drugs/published/Biosimilar-Product-Regulatory-Review-and-Approval.pdf
- Biosimilar Regulatory Review and Approval – FDA, accessed July 17, 2025, https://www.fda.gov/media/151061/download
- www.goodrx.com, accessed July 17, 2025, https://www.goodrx.com/drugs/biologics/what-are-biologics-and-biosimilars#:~:text=Biologics%20are%20complex%20medications%20that%20come%20from%20natural%20and%20living,Semglee%2C%20Amjevita%2C%20and%20Inflectra.
- Biosimilar medicines: Overview – EMA – European Union, accessed July 17, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/biosimilar-medicines-overview
- Transforming healthcare with biosimilars: lower costs, greater access, smarter solutions, accessed July 17, 2025, https://www.wolterskluwer.com/en/expert-insights/transforming-healthcare-biosimilars-lower-costs-smarter-solutions
- Op-Ed: Expand Patient Choice to Lower Medication Costs – Articularis – Healthcare Group, accessed July 17, 2025, https://articularishealthcare.com/news/op-ed-expand-patient-choice-to-lower-medication-costs/
- Patient Out-of-Pocket Costs for Biologic Drugs After Biosimilar Competition – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10980968/
- Biosimilar Adoption: Why Low Uptake is Still a Challenge – SmithRx, accessed July 17, 2025, https://www.smithrx.com/blog/biosimilar-adoption-why-low-uptake-is-still-a-challenge
- Report: 2023 U.S. Generic and Biosimilar Medicines Savings Report, accessed July 17, 2025, https://accessiblemeds.org/resources/reports/2023-savings-report-2/
- The U.S. Generic & Biosimilar Medicines Savings Report, accessed July 17, 2025, https://accessiblemeds.org/wp-content/uploads/2025/01/AAM-2024-Generic-Biosimilar-Medicines-Savings-Report.pdf
- Biosimilars Drive Cost Savings and Achieve 53% Market Share Across Treatment Areas, accessed July 17, 2025, https://www.centerforbiosimilars.com/view/biosimilars-drive-cost-savings-and-achieve-53-market-share-across-treatment-areas
- Biosimilar medicines: marketing authorisation – EMA – European Union, accessed July 17, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/marketing-authorisation/biosimilar-medicines-marketing-authorisation
- The European Medicines Agency Proposes Streamlined Pathway for the Approval of Biosimilar Medicinal Products in the EU | BioSlice Blog, accessed July 17, 2025, https://www.biosliceblog.com/2025/06/the-european-medicines-agency-proposes-streamlined-pathway-for-the-approval-of-biosimilar-medicinal-products-in-the-eu/
- Biological guidelines | European Medicines Agency (EMA), accessed July 17, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/research-and-development/scientific-guidelines/biological-guidelines
- Biosimilars (US and EU) Strategic Pharmaceutical CI Insights – DataM Intelligence, accessed July 17, 2025, https://www.datamintelligence.com/strategic-insights/biosimilars-us-and-eu
- Medicare Price Negotiations Will Slow Biosimilar Momentum, Widening Market Gap, accessed July 17, 2025, https://www.centerforbiosimilars.com/view/medicare-price-negotiations-will-slow-biosimilar-momentum-widening-market-gap
- Biosimilars in Focus: Advancing Implementation in Health Care Systems, accessed July 17, 2025, https://www.ajmc.com/view/biosimilars-in-focus-advancing-implementation-in-health-care-systems
- Report: 2022 U.S. Generic and Biosimilar Medicines Savings Report, accessed July 17, 2025, https://accessiblemeds.org/resources/reports/2022-savings-report/
- Reduction of biologic pricing following biosimilar introduction: Analysis across 57 countries and regions, 2012–19 – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11156405/
- Biosimilar drug market competition results in significantly reduced costs – HSC News, accessed July 17, 2025, https://hscnews.usc.edu/biosimilar-drug-market-competition-results-in-significantly-reduced-costs
- Study: Biosimilars ‘Fulfilling Their Promise’ of Lowering Biologic Prices – BioSpace, accessed July 17, 2025, https://www.biospace.com/study-biosimilars-fulfilling-their-promise-of-lowering-biologic-prices
- Increased Competition Is Lowering Trastuzumab Prices – Center for Biosimilars, accessed July 17, 2025, https://www.centerforbiosimilars.com/view/increased-competition-is-lowering-trastuzumab-prices
- Infliximab Biosimilar Competition did not Improve Affordability for Patients – HCPLive, accessed July 17, 2025, https://www.hcplive.com/view/infliximab-biosimilar-competition-did-not-improve-affordability-for-patients
- Budget impact analysis of including biosimilar adalimumab on formulary: A United States payer perspective – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11522441/
- Budget impact analysis of including biosimilar adalimumab on formulary: A United States payer perspective | Journal of Managed Care & Specialty Pharmacy, accessed July 17, 2025, https://www.jmcp.org/doi/10.18553/jmcp.2024.24036
- Originator Biologics and Biosimilars: Payment Policy Solutions to Increase Price Competition While Maintaining Market Sustainabi, accessed July 17, 2025, https://healthpolicy.duke.edu/sites/default/files/2021-11/Realizing%20the%20Benefits%20of%20Biosimilars%20Part%20B.pdf
- Patient out-of-pocket and payer costs for pegfilgrastim originator vs biosimilars as primary prophylaxis of febrile neutropenia in the first cycle among a commercially insured population – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10372998/
- Patient out-of-pocket and payer costs for pegfilgrastim originator vs biosimilars as primary prophylaxis of febrile neutropenia in the first cycle among a commercially insured population | Journal of Managed Care & Specialty Pharmacy, accessed July 17, 2025, https://www.jmcp.org/doi/10.18553/jmcp.2022.28.7.795
- Biosimilar Bevacizumab Market Size, Growth, Trends 2034 | MRFR, accessed July 17, 2025, https://www.marketresearchfuture.com/reports/biosimilar-bevacizumab-market-21960
- Real-World Tolerability and Financial Impact of Biosimilar Bevacizumab-awwb Compared With Bevacizumab in Patients With Cancer, accessed July 17, 2025, https://jhoponline.com/issue-archive/2024-issues/april-2024-vol-14-no-2/real-world-tolerability-and-financial-impact-of-biosimilar-bevacizumab-awwb-compared-with-bevacizumab-in-patients-with-cancer
- Biosimilars Boom: Rituximab Biosimilars Market Poised for 12% CAGR Surge from 2024 to 2031 – BioSpace, accessed July 17, 2025, https://www.biospace.com/biosimilars-boom-rituximab-biosimilars-market-poised-for-12-percent-cagr-surge-from-2024-to-2031
- Budget Impact Analysis of the Introduction of Rituximab and Trastuzumab Intravenous Biosimilars to EU-5 Markets – PMC – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7803676/
- Copay Adjustment Programs: What Are They and What Do They Mean for Consumers?, accessed July 17, 2025, https://www.kff.org/health-costs/issue-brief/copay-adjustment-programs-what-are-they-and-what-do-they-mean-for-consumers/
- Copay Accumulator Programs: What They Are And How They Might Impact Your Out-Of-Pocket Costs – Spondylitis Association of America, accessed July 17, 2025, https://spondylitis.org/spondylitis-plus/copay-accumulator-programs-what-they-are-and-how-they-might-impact-your-out-of-pocket-costs/
- Study: More Biosimilar Competition Is Not Lowering Patient OOP Costs, accessed July 17, 2025, https://www.centerforbiosimilars.com/view/study-more-biosimilar-competition-is-not-lowering-patient-oop-costs
- Correlation Between Changes in Brand-Name Drug Prices and Patient Out-of-Pocket Costs, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8097497/
- Drug Costs and Their Impact on Care | Arnold Ventures, accessed July 17, 2025, https://www.arnoldventures.org/stories/drug-costs-and-their-impact-on-care
- Drug Costs and Their Impact on Care: Insights from Medicare Patients and Providers – Commonwealth Fund, accessed July 17, 2025, https://www.commonwealthfund.org/publications/issue-briefs/2025/feb/drug-costs-impact-care-insights-medicare-patients-providers
- Expert: Overcoming Barriers to Wider Biosimilar Adoption – Pharmacy Times, accessed July 17, 2025, https://www.pharmacytimes.com/view/expert-overcoming-barriers-to-wider-biosimilar-adoption
- Medicare’s recent actions to promote access to lower cost drugs – Brookings Institution, accessed July 17, 2025, https://www.brookings.edu/articles/medicares-recent-actions-to-promote-access-to-lower-cost-drugs/
- Unlocking the Future of Biosimilars – Politico, accessed July 17, 2025, https://www.politico.com/sponsored/2025/05/unlocking-the-future-of-biosimilars/
- Biocon Biologics Patient Assistance Program (U.S.): Enabling Affordable Access to Vital Medicines, accessed July 17, 2025, https://www.bioconbiologicsus.com/pap
- What role do IP rights play in biologics and biosimilars? – Patsnap Synapse, accessed July 17, 2025, https://synapse.patsnap.com/article/what-role-do-ip-rights-play-in-biologics-and-biosimilars
- Leveraging Drug Patent Data for Strategic Investment Decisions: A Comprehensive Analysis, accessed July 17, 2025, https://www.drugpatentwatch.com/blog/leveraging-drug-patent-data-for-strategic-investment-decisions-a-comprehensive-analysis/
- Failure to Launch: Biosimilar Sales Continue to Fall Flat in the United States – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7255927/
- Navigating the Patent Thicket: Balancing Innovation, Biosimilar Access in the Biologics Market, accessed July 17, 2025, https://www.centerforbiosimilars.com/view/navigating-the-patent-thicket-balancing-innovation-biosimilar-access-in-the-biologics-market
- Cracking the Biosimilar Code: A Deep Dive into Effective IP Strategies – DrugPatentWatch, accessed July 17, 2025, https://www.drugpatentwatch.com/blog/cracking-the-biosimilar-code-a-deep-dive-into-effective-ip-strategies/
- Navigating Patent Thickets in the Age of Biosimilars – WIT Legal, accessed July 17, 2025, https://www.witlegal.com/insights/blog/big-pharmas-balancing-act-navigating-patent-thickets-in-the-age-of-biosimilars/
- Accelerating biosimilar market access: the case for allowing earlier standing | Journal of Law and the Biosciences | Oxford Academic, accessed July 17, 2025, https://academic.oup.com/jlb/article/12/1/lsae030/7942247
- Analyzing biosimilar market dynamics in different patient populations – DrugPatentWatch, accessed July 17, 2025, https://www.drugpatentwatch.com/blog/analyzing-biosimilar-market-dynamics-in-different-patient-populations/
- How to Evaluate the Patent Landscape Before Developing a Biosimilar – Patsnap Synapse, accessed July 17, 2025, https://synapse.patsnap.com/article/how-to-evaluate-the-patent-landscape-before-developing-a-biosimilar
- Addressing Patent Challenges in Biologics and Biosimilars – PatentPC, accessed July 17, 2025, https://patentpc.com/blog/addressing-patent-challenges-biologics-and-biosimilars
- Biosimilar Cost Savings in the United States: Initial Experience and Future Potential – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6075809/
- Medicare Drug Price Negotiation has Chilling Effect on Generic and Biosimilar Medicines Development and Availability, accessed July 17, 2025, https://accessiblemeds.org/resources/press-releases/medicare-drug-price-negotiation-has-chilling-effect-on-generic-and-biosimilar-medicines-development-and-availability/
- How HCP attitudes are shaping biosimilar market growth – ZS, accessed July 17, 2025, https://www.zs.com/insights/biosimilars-physician-attitudes-humira-uptake
- Attitude, Education Among Non-Economic Barriers Hinder Adoption of Biosimilars, accessed July 17, 2025, https://www.pharmacytimes.com/view/attitude-education-among-non-economic-barriers-hinder-adoption-of-biosimilars
- Physicians’ and patients’ perception of biosimilars and factors affecting biosimilar prescribing in selected Asian countries: a survey study – PubMed, accessed July 17, 2025, https://pubmed.ncbi.nlm.nih.gov/39234698/
- Fostering the Adoption of Biosimilars Into Clinical Practice – U.S. Pharmacist, accessed July 17, 2025, https://www.uspharmacist.com/article/fostering-the-adoption-of-biosimilars-into-clinical-practice
- Advocacy – Biosimilars Forum, accessed July 17, 2025, https://biosimilarsforum.org/advocacy/
- (PDF) Understanding the factors influencing the adoption of biosimilars; an innovation theory perspective – ResearchGate, accessed July 17, 2025, https://www.researchgate.net/publication/393001211_Understanding_the_factors_influencing_the_adoption_of_biosimilars_an_innovation_theory_perspective
- Barriers and Enablers Affecting the Uptake of Biosimilar Medicines Viewed Through the Lens of Actor Network Theory: A Systematic Review, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11247062/
- What role for real-world evidence in market access of biosimilars? – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11891046/
- What is Competitive Intelligence in the pharmaceutical industry? – Lifescience Dynamics, accessed July 17, 2025, https://www.lifesciencedynamics.com/press/articles/what-is-competitive-intelligence-in-the-pharma-industry/
- Biosimilars Market Growth Driven by Patent Expirations and Rising Demand – Towards Healthcare, accessed July 17, 2025, https://www.towardshealthcare.com/insights/biosimilars-market
- The Future of Biosimilars: Maximizing Benefits Across Immune-Mediated Inflammatory Diseases – PMC – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7007415/
- Samsung Bioepis’ European Whitepaper Proposes Solutions to Bridge Policy Gaps that Hinder Healthy Market Competition and Timely Access to Biosimilar Medicines – FirstWord Pharma, accessed July 17, 2025, https://firstwordpharma.com/story/5980929
- What the experts are saying about biosimilars | Health and Social Services, accessed July 17, 2025, https://www.hss.gov.nt.ca/en/services/biosimilar-initiative/what-experts-are-saying-about-biosimilars