Section 1: The Inevitable Cliff and the Valley of Opportunity
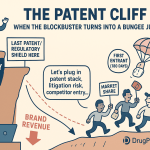
In the high-stakes world of pharmaceuticals, there is no force more predictable, more disruptive, and more transformative than the expiration of a drug patent. For decades, the industry has operated on a cycle of innovation, exclusivity, and reinvestment, a model powered by the temporary monopoly that patents provide. But this monopoly has a finite lifespan. When the clock runs out, the innovator company often finds itself staring over the edge of a “patent cliff”—a term that vividly captures the sudden and precipitous drop in revenue that follows the loss of exclusivity (LOE).1
The scale of this phenomenon is staggering. The period between 2025 and 2030 is projected to be one of the most significant patent cliffs in history, putting an estimated $200 billion to $300 billion in annual global revenue at risk.4 For an individual blockbuster drug, the consequences are stark. Upon the market entry of lower-cost generic alternatives, the original brand can expect to lose 80% to 90% of its market share, often within the first 12 to 24 months.4 It’s a moment of peril that can shake even the largest pharmaceutical giants to their core, forcing painful restructuring and a frantic search for new sources of growth.
Yet, this narrative of decline tells only half the story. The patent cliff is a dual-faced event. For every dollar of revenue lost by an innovator, there is a corresponding, and often greater, value created for the healthcare system and for patients. The entry of generic and biosimilar medicines unleashes powerful competitive forces that drive down prices, expand access, and generate immense savings. In 2022 alone, these lower-cost alternatives saved the U.S. healthcare system a breathtaking $408 billion, contributing to a cumulative savings of over $2.9 trillion in the preceding decade.12 Today, generics account for more than 90% of all prescriptions filled in the United States, yet they represent only about 17.5% of total prescription drug spending—a testament to their profound economic impact.12
This report is designed for the strategic decision-maker who understands that patent expiration is not a force of nature to be feared, but a complex market dynamic to be mastered. It is a guide for turning the industry’s most predictable disruption into a source of competitive advantage.
The very term “patent cliff” is, for the well-prepared organization, a misnomer. A cliff implies a sudden, unforeseen drop. But patent expiration dates are known years, often decades, in advance.16 They are not unexpected events but scheduled, recurring milestones in a product’s lifecycle. The “cliff” metaphor accurately describes the
financial outcome for companies that fail to plan, but it misrepresents the strategic reality. The true competitive differentiator lies not in avoiding the inevitable, but in mastering the art of the transition: for innovators, a controlled and managed descent that maximizes value until the very end; for generic and biosimilar manufacturers, a well-timed and powerful ascent into the valley of opportunity that opens up. A company that “falls” off the cliff has not been a victim of a sudden crisis; it has been a victim of a failure in its own long-range strategic foresight. This reframing—from crisis management to strategic navigation—is the essential first step toward thriving in a post-exclusivity world.
Over the following sections, we will deconstruct the intricate architecture of this landscape. We will explore the legal frameworks that govern exclusivity, the market dynamics that define competition, the offensive and defensive playbooks used by brand and generic players, and the powerful data-driven strategies that can illuminate the path forward. For in this high-stakes environment, the ticking clock of patent expiration is not just a countdown to loss; it is a metronome setting the rhythm of the entire market. The companies that learn to move in time with it will be the ones that lead the industry into its next chapter.
Section 2: The Architecture of Exclusivity: Understanding the Drug Patent Lifecycle
To master the impact of patent expiration, one must first understand the intricate legal and regulatory structures that define a drug’s period of market monopoly. This “architecture of exclusivity” is not a single, simple barrier but a complex, multi-layered defense system built from both patent law and regulatory provisions. For business strategists, deconstructing this architecture is the critical first step in identifying both vulnerabilities and opportunities.
The 20-Year Patent Term: A Theoretical Lifespan
The foundation of a drug’s exclusivity is its patent. Governed by international agreements like the Agreement on Trade-Related Aspects of Intellectual Property Rights (TRIPS), the standard statutory term for a drug patent in most major jurisdictions, including the United States, Europe, and Japan, is 20 years from the date the patent application was filed.10
However, this 20-year figure is profoundly misleading when it comes to a drug’s commercial life. The patent clock starts ticking the moment the application is filed, a step that pharmaceutical companies take very early in the development process to secure their intellectual property on a promising molecule. What follows is a long and arduous journey of preclinical research, extensive and costly multi-phase clinical trials, and a rigorous regulatory review by agencies like the U.S. Food and Drug Administration (FDA). This entire process can easily consume 10 to 15 years of the 20-year patent term before the drug ever reaches the market and generates its first dollar of revenue.16
Consequently, the “effective patent life”—the actual period during which a drug is sold on the market under patent protection, free from generic competition—is often much shorter, typically averaging between 7 and 14 years.9 This truncated window for recouping massive R&D investments, which can range from hundreds of millions to billions of dollars, creates immense economic pressure and underpins many of the strategic behaviors we see as a patent’s expiration date approaches.
The Hierarchy of Patents: Not All IP is Created Equal
The patent protection surrounding a single drug is rarely monolithic. Innovator companies strategically build a portfolio of patents covering different aspects of their product. The most valuable and sought-after of these is the composition of matter patent. This patent covers the active pharmaceutical ingredient (API) itself—the core chemical entity responsible for the drug’s therapeutic effect. It is the strongest form of protection because it prevents any competitor from making, using, or selling the same drug substance, regardless of how it is formulated or what it is used for.
Beyond this core protection, companies often file secondary patents, such as:
- Method of Use Patents: These patents cover a specific, novel way of using a drug to treat a particular disease or condition. For example, a drug initially approved for hypertension might later be found effective for heart failure, and this new use can be patented.
- Formulation Patents: These cover the specific recipe of the final drug product, including inactive ingredients (excipients), delivery mechanisms (e.g., extended-release technology), or dosage forms (e.g., a tablet vs. a capsule).
- Process Patents: These protect a specific, novel method of manufacturing the drug.
These different patents often have different filing and expiration dates, creating a complex and overlapping web of protection often referred to as a “patent thicket”.18
A Layer Cake of Protection: Regulatory Exclusivities
Layered on top of the patent system is a separate framework of regulatory exclusivities granted by the FDA. These are statutory periods of market protection that are independent of a drug’s patent status. They were designed to provide additional incentives for innovation in specific circumstances. Key regulatory exclusivities in the U.S. include:
- New Chemical Entity (NCE) Exclusivity: A five-year period of market exclusivity granted to the first company to gain approval for a drug containing a new active ingredient that has never before been approved by the FDA. During this period, the FDA cannot accept an Abbreviated New Drug Application (ANDA) from a generic competitor for the first four years (or five if the generic does not include a patent challenge).19
- Orphan Drug Exclusivity (ODE): To incentivize the development of drugs for rare diseases (affecting fewer than 200,000 people in the U.S.), the FDA grants a seven-year period of market exclusivity for a drug approved with an orphan designation. During this time, the FDA cannot approve another application for the same drug for the same orphan indication.19
- Biologics Exclusivity: Under the Biologics Price Competition and Innovation Act (BPCIA), innovator biologics receive a 12-year period of exclusivity from the date of first licensure. The FDA cannot approve a biosimilar application until this period has passed.
- Pediatric Exclusivity: If a company conducts pediatric studies of its drug in response to a written request from the FDA, it can receive an additional six months of market exclusivity. This valuable extension is tacked onto any existing patent and regulatory exclusivities the drug may have.19
Restoring Lost Time: Patent Term Extensions
Recognizing that the lengthy regulatory review process erodes a significant portion of a patent’s life, legal frameworks were established to compensate innovators. In the United States, the Patent Term Extension (PTE) program, established by the Hatch-Waxman Act, allows for the restoration of some of the patent time lost during clinical trials and FDA review. A company can extend one patent on a product for a period of time, with the total extension capped at five years and the resulting patent term not to exceed 14 years from the drug’s approval date.17 Europe has a similar mechanism known as a
Supplementary Protection Certificate (SPC).10
This intricate system reveals a crucial reality of the pharmaceutical business. The intellectual property landscape is not a single wall represented by one patent. Instead, it is a complex fortress with overlapping fields of fire, constructed from multiple patents covering different aspects of a product and further reinforced by various regulatory exclusivities. A generic or biosimilar competitor cannot simply mark a single date on the calendar. They must conduct a sophisticated analysis of a matrix of legal and regulatory expiration dates, each with its own rules and duration. This complexity is not an accident; it is, in itself, a powerful defensive strategy for innovators. The layering of protections creates a “defense-in-depth” system, where even if one patent falls, others may still stand. For a would-be competitor, the challenge is not to breach a single wall, but to find the path of least resistance through the entire defensive system, a task that makes deep competitive and legal intelligence an absolute prerequisite for success.
Section 3: The Hatch-Waxman Act: The Law That Forged the Modern Generic Market
No single piece of legislation has had a more profound and lasting impact on the U.S. pharmaceutical market than the Drug Price Competition and Patent Term Restoration Act of 1984, universally known as the Hatch-Waxman Act.14 Before its passage, the generic drug industry was nascent and hamstrung. Generic applicants faced the insurmountable hurdle of having to conduct their own expensive and ethically questionable clinical trials to prove the safety and efficacy of drugs that had already been proven safe and effective by the innovator company. As a result, in 1984, generics accounted for a mere 19% of prescriptions.
The Hatch-Waxman Act was a masterful piece of legislative engineering that created a “grand bargain” to balance the competing interests of innovator and generic drug manufacturers.14 It simultaneously preserved incentives for high-risk R&D while creating a streamlined pathway for low-cost generics to enter the market. In doing so, it didn’t just create a market; it created a sophisticated strategic game with clearly defined rules, players, moves, and prizes—a game that continues to define competition today.
The Grand Bargain: A Two-Sided Agreement
The genius of Hatch-Waxman lies in its balanced approach. It gave something significant to both sides of the industry aisle:
- For Innovators: The Act created the system of Patent Term Restoration (PTE), allowing brand-name companies to recoup some of the patent life lost during the lengthy FDA approval process, as discussed in the previous section. This preserved the financial incentive to undertake the risky endeavor of new drug development.
- For Generics: The Act created the Abbreviated New Drug Application (ANDA) pathway, the cornerstone of the modern generic industry.14 This pathway streamlined the approval process by allowing a generic manufacturer to rely on the FDA’s previous finding of safety and effectiveness for the innovator’s drug (known as the Reference Listed Drug, or RLD). Instead of repeating clinical trials, the generic firm only needed to demonstrate that its product was bioequivalent—meaning it delivered the same amount of the active ingredient into the bloodstream over the same period of time.17 This dramatically lowered the cost and time required to bring a generic to market.
The Rulebook: Key Mechanisms of the Hatch-Waxman Game
To manage this new competitive dynamic, the Act established several key mechanisms that function as the rules of the game:
1. The “Orange Book”: The Official Game Board
The Act elevated the FDA’s publication, “Approved Drug Products with Therapeutic Equivalence Evaluations,” commonly known as the Orange Book, into the central repository for patent and exclusivity information. It mandated that innovator companies list all relevant patents protecting their drugs in the Orange Book. This transformed it from a simple clinical reference into an essential competitive intelligence tool, the official “game board” where all players could see the patent barriers associated with any given drug.
2. The Paragraph IV Certification: The Aggressive Move
When filing an ANDA, a generic company must make a certification for each patent listed in the Orange Book for the brand-name drug. While there are several types of certifications, the most strategically important is the Paragraph IV (P-IV) certification. By filing a P-IV certification, the generic applicant asserts that the brand’s patent is either invalid, unenforceable, or will not be infringed by the generic product. This is not a passive waiting game; it is an aggressive move that directly challenges the innovator’s intellectual property and initiates a potential legal confrontation.
3. The 30-Month Stay: The Timer
A P-IV certification is a declaration of war. The generic applicant must notify the brand company of its filing. If the brand company files a patent infringement lawsuit against the generic applicant within 45 days, it triggers an automatic 30-month stay on the FDA’s ability to grant final approval to the ANDA.26 This 30-month period acts as a “timer,” providing a window for the courts to resolve the patent dispute before the generic drug can enter the market.
4. The 180-Day Exclusivity: The “Brass Ring” Prize
To incentivize generic companies to undertake the costly and risky endeavor of patent litigation, Hatch-Waxman created a powerful prize: 180 days of market exclusivity.22 The first generic applicant to submit a “substantially complete” ANDA with a P-IV certification becomes eligible for this reward. If successful, this “first-to-file” generic is granted a 180-day period during which the FDA cannot approve any subsequent ANDAs for the same drug from other generic competitors.22
This exclusivity period is the “brass ring” that drives the entire system of patent challenges. For six months, the first generic can enjoy a lucrative duopoly with the brand-name drug, capturing significant market share at a price point much higher than what would be possible in a fully competitive multi-generic market. The potential for this reward is what motivates generic firms to spend millions on litigation and challenge patents years before they are set to naturally expire, accelerating patient access to more affordable medicines. For example, generics that launched with 180-day exclusivity saved the U.S. healthcare system nearly $20 billion in 2020 alone.
The intricate structure of the Hatch-Waxman Act demonstrates that success in the generic industry is about much more than manufacturing prowess. The Act created a system of calculated risk-taking, a strategic game where timing, legal acumen, and regulatory strategy are paramount. Companies that excel are not necessarily those who make the cheapest pill, but those who best master the gameplay of this complex framework. They understand when to file a P-IV certification, how to navigate the ensuing litigation, when to settle, and how to leverage the rules to secure the coveted 180-day prize. This is why legal and regulatory experts are as critical as scientists and manufacturing heads in the C-suites of today’s leading generic pharmaceutical companies.
Section 4: When the Levee Breaks: Market Dynamics Post-Exclusivity
The moment a drug’s patent and regulatory exclusivities expire and the first generic competitor enters the market is akin to a dam breaking. The pent-up forces of competition are unleashed, and the market landscape is irrevocably and rapidly transformed. For brand-name manufacturers, this period, known as the Loss of Exclusivity (LOE), is characterized by a swift and brutal erosion of price and market share. Understanding the mechanics of this shift is crucial for both innovators seeking to defend their franchise and generics aiming for rapid market capture.
The Cascade of Price Erosion
The most immediate and dramatic impact of generic entry is on price. During its monopoly period, an innovator can command a premium price. Once that monopoly is broken, a cascade of price erosion begins, a phenomenon that has been well-documented and follows a predictable pattern.
Studies have shown that the entry of a single generic competitor typically results in only a modest discount. However, the real price collapse occurs with the entry of the second, third, and subsequent generics.32 The competition for market share among multiple manufacturers creates intense downward pressure on price. On average, generic drug prices can plummet to just 20% or even less of the original brand price.10 Some analyses have found that generics can cost 80-85% less than their brand-name counterparts.
This price decay tends to follow what is described as a “scalloped curve”. The decline is sharpest in the initial months following multi-generic entry and then gradually flattens out as the price approaches the marginal cost of production. The steepness of this curve varies depending on the product’s complexity. For simple oral solid dosage forms (like tablets and capsules) that are relatively easy to manufacture, the price erosion is typically rapid and severe, as many competitors can enter the market. For more complex products, such as sterile injectables, transdermal patches, or inhalation devices, the price decay is often slower because the technical barriers to entry are higher, resulting in fewer competitors.
The Great Market Share Migration
Hand-in-hand with price erosion is a massive and rapid shift in market share. Propelled by automatic substitution policies at the pharmacy level and the powerful incentives of payers and Pharmacy Benefit Managers (PBMs) to steer patients toward lower-cost alternatives, the brand-name drug’s dominance evaporates. It is not uncommon for a blockbuster brand to lose 80% to 90% of its prescription volume within the first one to two years of facing multi-generic competition.4 This migration is one of the most powerful forces in the pharmaceutical economy, responsible for transferring billions of dollars in spending from innovator products to generics annually.
The Innovator’s Counter-Move: The Authorized Generic
Faced with this inevitable onslaught, innovator companies are not without strategic responses. One of the most potent and widely used tactics is the launch of an Authorized Generic (AG). An AG is the innovator’s own branded drug, packaged and sold as a generic, typically through a subsidiary or a partner company.23
Crucially, an AG is not approved via the ANDA pathway like a typical generic. It is marketed under the brand’s original New Drug Application (NDA) because it is, in every respect—active ingredient, inactive ingredients, size, shape, and color—the exact same product as the brand, just without the brand name on the label. This provides a key point of differentiation from standard generics, which are only required to have the same active ingredient and be bioequivalent, but can differ in their inactive ingredients and physical appearance. This identity can be a powerful tool for patient and physician reassurance, potentially improving adherence for patients who are wary of switching.23
The strategic brilliance of the AG lies in its timing. The innovator can launch its AG to compete directly with the “first-to-file” generic challenger during their 180-day exclusivity period. This move fundamentally alters the market dynamics. What the first-filer hoped would be a lucrative duopoly (brand vs. first generic) instantly becomes a three-player market (brand vs. first generic vs. authorized generic).
This maneuver is, in essence, a “scorched earth” defensive strategy. By launching an AG, the innovator deliberately cannibalizes its own high-priced brand sales to immediately and drastically reduce the market value of the 180-day exclusivity period for its challenger. It is a powerful signal from the innovator that says, “If I can no longer have my monopoly profits, I will ensure your hard-won prize is as unprofitable as possible.” This tactic forces a generic company considering a patent challenge to rethink its financial models. The potential reward is no longer the value of a duopoly but the much lower value of a fragmented, three-way competition. The threat of an AG launch thus serves as a significant deterrent, raising the stakes and changing the entire risk/reward calculation for would-be patent challengers.
Section 5: High-Stakes Gambles: The Strategy of At-Risk Launches
In the high-stakes chess match between innovator and generic firms, few moves are as bold or as fraught with peril as the “at-risk” launch. This aggressive strategy involves a generic company launching its product into the market after receiving FDA approval but before all patent litigation with the brand-name company has been finally resolved.29 It is the ultimate expression of a company’s confidence in its legal position and its appetite for risk, a calculated gamble where the potential rewards are immense, but the potential penalties are catastrophic.
Defining the Risk: A Bet-the-Company Proposition
The “risk” in an at-risk launch is primarily financial and legal. If a generic company launches its product while a patent infringement case is still under appeal, and the appeals court ultimately sides with the brand-name company, the consequences can be devastating. The generic firm can be found liable for patent infringement and ordered to pay massive damages.29
These damages are typically calculated based on the brand’s lost profits during the period of infringement, which can be enormous for a blockbuster drug. Furthermore, if the infringement is deemed to be “willful,” the court can award treble damages, multiplying the financial penalty threefold.11 This potential exposure can easily dwarf the profits the generic company actually earned from its at-risk sales, in some cases representing a liability of two dollars or more for every one dollar of profit gained. A famous example involved Glenmark, which launched a generic version of Sanofi-Aventis’s Tarka at risk and was subsequently hit with a $16 million damages verdict. For a smaller generic company, such a loss could be an existential blow.
The Reward: Capturing the First-Mover Advantage
So, why would any company take such a monumental risk? The answer lies in the equally significant potential reward. A successful at-risk launch allows a generic company to enter the market months or even years before it could have if it had waited for all legal appeals to be exhausted.40 This early entry provides a crucial first-mover advantage, allowing the company to capture substantial market share and generate hundreds of millions of dollars in revenue that would otherwise have been unattainable. In the fast-eroding generic market, being first is everything, and an at-risk launch is the most aggressive way to secure that position.
The Economic Calculus: Modeling the Gamble
The decision to launch at-risk is not a reckless whim but a sophisticated economic calculation. As detailed in an NBER working paper, the decision hinges on a model that weighs the expected profits from early entry against the potential for damages, discounted by the probability of losing the litigation.42
The model shows that after a generic company has already won its case at the district court level, the odds shift dramatically in its favor. Appellate courts rarely overturn district court decisions in patent litigation, meaning the generic’s perceived probability of ultimate success is very high. In this scenario, the economic model predicts that an at-risk launch is almost always profitable and will occur as quickly as possible after FDA approval is granted.42 The only exception is when the cost of waiting for the appeal decision is extremely low—for instance, if FDA approval is granted just a few weeks before the appeal is expected to be decided. In that case, the limited potential for at-risk sales may not outweigh even the small risk of a reversal on appeal.
This prediction is borne out by real-world data. One study found that among generic drugs that did not settle their cases and received FDA approval prior to a favorable district court decision, 100% were launched at risk.42
An at-risk launch is far more than a simple business decision; it is a powerful piece of legal and market signaling. The act of launching communicates the generic firm’s absolute and unwavering confidence in its legal position to the innovator, to investors, to payers, and to the courts themselves. A company would not expose itself to the risk of catastrophic financial damages unless its internal assessment of winning the litigation was overwhelmingly positive. This act of “putting your money where your mouth is” is a credible, non-verbal signal that the generic company is not bluffing and is prepared to fight the legal battle to its conclusion. This can fundamentally change the dynamic of any ongoing settlement negotiations. The brand-name company, now facing a daily bleed of market share and revenue, sees that its opponent is resolute. This pressure can force the innovator to re-evaluate its own legal position and offer a more favorable settlement to the generic simply to stop the financial hemorrhaging, effectively making the market launch itself a powerful piece of litigation leverage.
Section 6: The New Frontier: Biologics, Biosimilars, and the “Patent Dance”
As the pharmaceutical industry moves deeper into the 21st century, the landscape of patent expirations is undergoing a fundamental transformation. The focus is shifting from traditional, chemically synthesized small-molecule drugs to large, complex biologics. This shift brings with it a whole new set of scientific, regulatory, and legal challenges. The “generic” versions of biologics are not generics at all; they are biosimilars, and their path to market is governed by a unique and intricate framework established by the Biologics Price Competition and Innovation Act (BPCIA) of 2009.44 At the heart of this framework is a complex, strategic process colloquially known as the “patent dance.”
Why “Biosimilar” and Not “Generic”?
The distinction in terminology is critical and stems from fundamental scientific differences. Small-molecule drugs like aspirin or atorvastatin (Lipitor) have simple, well-defined chemical structures that can be replicated exactly. A generic is, for all intents and purposes, identical to its brand-name counterpart.
Biologics, in contrast, are massive, complex proteins or antibodies produced in or derived from living organisms (such as bacteria or mammalian cells).45 Their intricate, three-dimensional structures are highly sensitive to the manufacturing process. Even minor variations in cell lines, temperature, or purification methods can result in subtle differences in the final product. Because of this inherent variability, it is scientifically impossible to create an exact copy of a biologic. Therefore, a competitor product cannot be proven “identical,” only
“highly similar” to the innovator’s reference product, with no clinically meaningful differences in terms of safety, purity, and potency.45 This is the origin of the term “biosimilar.”
The BPCIA: A New Rulebook for a New Class of Drugs
Recognizing these complexities, Congress created a new regulatory pathway for biosimilars through the BPCIA. This act established the abbreviated Biologics License Application (aBLA), which allows a biosimilar developer to rely on some of the innovator’s clinical data, similar to the ANDA pathway for small-molecule generics.
However, the BPCIA also provided stronger protections for biologic innovators to reflect the higher cost and complexity of their development. Most notably, it granted a much longer period of regulatory exclusivity: 12 years from the date of the innovator’s first licensure, during which the FDA cannot approve a biosimilar.
The Patent Dance: A Strategic Information Exchange
The most novel and complex element of the BPCIA is the patent resolution process it created—the so-called “patent dance.” This is a highly structured, multi-step procedure for the biosimilar applicant and the reference product sponsor (the innovator) to exchange information about patents and narrow the scope of potential legal disputes before full-blown litigation begins.44 The key steps, which can take approximately eight months to complete if followed in full, include :
- The Opening Move: Within 20 days of the FDA accepting its aBLA for review, the biosimilar applicant may provide the innovator with a copy of its application and detailed information about its manufacturing process.
- The Innovator’s List: Within 60 days, the innovator may provide the applicant with a list of all patents it believes could reasonably be asserted.
- The Applicant’s Response: The applicant then responds with its own list of patents it believes should be litigated and provides detailed statements explaining why the innovator’s patents are invalid, unenforceable, or not infringed.
- The Innovator’s Rebuttal: The innovator then provides a rebuttal to the applicant’s arguments.
- Negotiation: The two parties then negotiate to agree on a final list of patents that will be litigated in the first wave of infringement lawsuits. If they cannot agree, the statute dictates a formula for determining the number of patents to be litigated.
To Dance or Not to Dance: A Crucial Strategic Choice
Here is the critical twist: in its landmark 2017 decision in Amgen v. Sandoz, the U.S. Supreme Court ruled that this entire patent dance process is optional.44 A biosimilar applicant can choose to completely bypass the dance.
This ruling transformed the patent dance from a mandatory procedure into a purely strategic choice, a “game theory” problem for every biosimilar developer. The decision to dance or not to dance has profound consequences and reveals the applicant’s entire early litigation strategy:
- Choosing to Dance: By participating in the dance, a biosimilar applicant gains a degree of predictability and control. The process forces a narrowing of the dispute, allowing the applicant to focus its resources on a limited, agreed-upon set of patents in the first wave of litigation.45 This signals a desire for a more orderly, manageable legal process.
- Choosing to Opt Out: If an applicant refuses to dance, it cedes control to the innovator. The BPCIA provides a remedy for this refusal: the innovator can immediately file a broad patent infringement lawsuit, asserting any and all patents it believes are relevant.44 This path is more chaotic, more expensive, and less predictable.
Why would an applicant ever choose this more chaotic path? The likely strategic reason is that the applicant believes the innovator’s “patent thicket” is weak and full of patents that would not stand up to scrutiny. By refusing to dance, the biosimilar applicant essentially dares the innovator to assert its entire portfolio, hoping to expose the weakness of the overall position in court. It’s an aggressive strategy that signals a willingness to engage in a wide-ranging legal battle from day one.
Separate from the optional dance is a mandatory 180-day notice of commercial marketing. The BPCIA requires that a biosimilar applicant must notify the innovator at least 180 days before it plans to launch its product. This notice gives the innovator a final opportunity to seek a preliminary injunction and litigate any patents that were not part of the initial wave of litigation, effectively creating a potential second phase of legal conflict.
The optional nature of the patent dance has made the biosimilar landscape a fascinating arena of strategic maneuvering. The very first communication between a biosimilar applicant and an innovator—the decision to engage in the dance or to decline—is a crucial piece of competitive intelligence. It is the opening move in a high-stakes chess match that tells the innovator, and the entire market, a great deal about how the challenger views the strength of its IP fortress and how it intends to fight the war to come.
Section 7: Case Study: The Fall of a Titan – Pfizer’s War for Lipitor
No event in pharmaceutical history better exemplifies the term “patent cliff” than the loss of exclusivity for Pfizer’s Lipitor (atorvastatin). For years, Lipitor was not just a drug; it was an economic juggernaut, the best-selling pharmaceutical product in the world. Its story provides a masterclass in the defensive strategies an innovator can deploy when facing the loss of its crown jewel and demonstrates a pivotal shift in how the industry approaches the final, crucial phase of a blockbuster’s lifecycle.
The Unprecedented Stakes
At its zenith, Lipitor’s financial performance was staggering. In 2006, its peak sales reached $12.9 billion, and as late as 2010, it was still generating $10.7 billion annually, accounting for a massive one-sixth of Pfizer’s total revenues. The drug had contributed over $120 billion to Pfizer’s top line over its product life. The expiration of its U.S. patent on November 30, 2011, was therefore not just a business challenge; it was an existential threat that required an unprecedented defensive campaign.
The “180-Day War”: A Multi-Front Defense
Pfizer knew it could not prevent the eventual decline of Lipitor. Instead, it focused its immense resources on a fierce, multi-front campaign to manage the slope of that decline, concentrating its efforts on the critical 180-day exclusivity period granted to the first generic filer, Ranbaxy. Pfizer’s objective was to retain as much market share and revenue as possible during this crucial window, a strategy that came to be known as the “180-day war.” The key tactics included:
- The Authorized Generic Gambit: In a masterful strategic move, Pfizer partnered with generic manufacturer Watson Pharmaceuticals to launch an authorized generic (AG) version of atorvastatin. As detailed previously, this AG was the exact same pill as Lipitor, made by Pfizer, but sold at a generic price. This move instantly transformed the market from a simple brand-vs.-generic duopoly into a three-way competition. It directly attacked the profitability of Ranbaxy’s hard-won exclusivity, with Pfizer reportedly retaining a significant portion (estimated at 70%) of the profits from Watson’s AG sales.
- Aggressive Brand Loyalty Campaign: Rather than ceding the market, Pfizer doubled down on defending the Lipitor brand. It continued to pour money into Direct-to-Consumer (DTC) advertising, investing over $150 million in TV ads and more than $220 million in overall advertising for Lipitor in 2011 alone. The goal was to reinforce brand loyalty and create hesitation among patients and physicians about switching to an unfamiliar generic.
- Pricing and Co-pay Warfare: Pfizer aggressively used pricing instruments to compete directly with the generic. It rolled out a massive co-pay card program, allowing many commercially insured patients to continue receiving branded Lipitor for a co-pay as low as $4 per month. This effectively neutralized the primary advantage of the generic—its lower cost to the patient. Pfizer even paid pharmacies to mail information about this program directly to their patients, ensuring maximum uptake.
The Financial Aftermath: A Reshaped Cliff
Did Pfizer’s war succeed? The answer is nuanced. The company could not defy gravity entirely. The financial impact of LOE was still severe. In the first quarter of 2012, Pfizer’s overall earnings fell by 19% and its revenue by 7%, while global Lipitor sales plummeted by 42% compared to the prior year. Over a two-year period, Lipitor’s annual sales dropped from nearly $11 billion in 2010 to just $4 billion in 2012.
However, the defensive strategy was remarkably effective in mitigating the damage during the crucial first six months. While a typical brand might see its market share evaporate almost overnight, Pfizer’s multi-pronged approach allowed it to hold on to a U.S. market share of approximately 30% at the end of the 180-day exclusivity period—a figure that far exceeded analyst expectations. This translated into an additional $383 million in U.S. sales in that first quarter alone, revenue that would have been completely lost under a more passive strategy. While Ranbaxy captured over 50% of the generic atorvastatin market and earned an estimated $600 million, Pfizer’s aggressive tactics ensured that the generic’s victory was far less absolute than it could have been.
The Lipitor case study represents a fundamental paradigm shift in loss-of-exclusivity strategy. Before Lipitor, the conventional wisdom was for a brand to retreat gracefully upon generic entry. Pfizer rewrote the playbook, proving that an innovator could fight back. The goal was no longer to prevent the revenue cliff but to actively reshape its slope. By aggressively competing on brand loyalty, deploying an authorized generic, and neutralizing the generic’s price advantage with co-pay cards, Pfizer transformed what could have been a vertical freefall into a more manageable, albeit still very steep, decline. This comprehensive, aggressive defensive campaign bought the company precious time and billions in revenue, establishing the modern LOE defense playbook that has been studied and emulated by innovator companies ever since.
Section 8: Case Study: The Ripple Effect of Plavix’s Expiration
If the Lipitor case study is a lesson in defensive strategy, the patent expiration of the antiplatelet blockbuster Plavix (clopidogrel) is a powerful illustration of the broader, systemic impact of a major LOE event. Marketed jointly by Bristol-Myers Squibb (BMS) and Sanofi, Plavix was another titan of the pharmaceutical world. Its fall from patent protection in 2012 not only had a devastating financial impact on its manufacturers but also sent shockwaves through its entire therapeutic class, demonstrating how the entry of a single, high-impact generic can reset the economic landscape for all competing drugs, even those still under patent.
The High Stakes for BMS and Sanofi
Like Lipitor, Plavix was a cornerstone of its marketers’ portfolios. In 2010, the drug generated $6.15 billion in U.S. sales for BMS alone, accounting for a staggering 48.79% of the company’s total U.S. revenue. The company had already had a terrifying preview of what was to come when generic manufacturer Apotex briefly launched an at-risk version in 2006, a move that wreaked havoc on sales for months and underscored the brand’s vulnerability. The official patent expiration in May 2012 was a long-dreaded event that threatened the financial stability of both BMS and Sanofi.
Market Dynamics: A Rapid and Complete Takeover
When the patent levee finally broke, the market dynamics were swift and brutal. The entry of generic clopidogrel triggered an immediate and profound market shift. Unlike the heavily contested battle for Lipitor, the generic takeover of Plavix was more akin to a rapid and complete conquest.
- Massive Price Collapse: The introduction of generic alternatives led to a dramatic and sustained reduction in price. While the initial generic entrant offered a discount, the subsequent flood of competitors drove prices into a freefall. Over time, the price of clopidogrel fell to a small fraction of its pre-expiry level, with some analyses suggesting a drop to as low as 6.6% of the original brand price. The average price of a generic is often 90% lower than the brand it replaces.
- Immediate Generic Uptake: Driven by the huge cost savings, payers, pharmacies, and healthcare systems rapidly switched from branded Plavix to generic clopidogrel. Market analyses from the years following the 2012 expiration showed that generic versions quickly saturated the market, capturing between 56% and 92% of all clopidogrel prescriptions worldwide. This rapid uptake was facilitated by efficient regulatory pathways and the clear cost-effectiveness proposition that generics offered.36
For the innovator companies, the financial impact was as severe as predicted. The massive revenue stream that had supported their operations and R&D pipelines for years was decimated, forcing them to accelerate lifecycle management strategies, desperately seek new blockbusters to fill the gap, and pivot their R&D focus toward newer, patent-protected assets.4
The Spillover Effect: Lowering the Water for the Entire Pond
The most critical strategic lesson from the Plavix case study lies in what happened beyond the brand itself. The availability of a cheap, effective, and widely trusted generic like clopidogrel did not just destroy Plavix’s market share; it fundamentally altered the competitive dynamics for the entire antiplatelet therapeutic class.
Before 2012, other branded antiplatelet agents competed primarily with Plavix and each other on the basis of clinical differentiation and marketing muscle. After 2012, they faced a new and formidable competitor: a low-cost, clinically proven generic alternative.
Payers and PBMs, whose primary goal is to manage healthcare costs, naturally seized upon the opportunity presented by generic clopidogrel. They quickly moved to make it the preferred first-line option on their formularies, often requiring patients to try and fail on the generic before they would cover a more expensive branded alternative (a practice known as step therapy).
This move put immense downward price pressure on all other branded drugs in the class, even those still enjoying patent protection. To maintain their formulary access and defend their market share, these competing brands were forced to offer much deeper rebates and discounts to PBMs. In effect, they were no longer competing against a $300 brand, but a $30 generic. The patent cliff for Plavix had the effect of lowering the water level for the entire therapeutic pond.
This “spillover effect” is a critical insight for portfolio managers and competitive intelligence teams. When assessing the risk of a patent expiration, it is not enough to analyze the single product in isolation. One must consider the entire therapeutic area. The fall of a single blockbuster can reset the pricing benchmark for all players, creating a ripple effect that diminishes the value proposition and profitability of competing brands for years to come.
Section 9: The Looming Cliff (2025-2030): A New Wave of Blockbuster Expirations
The pharmaceutical industry is currently standing at the precipice of its next great patent cliff, a wave of expirations between 2025 and 2030 that is poised to be the largest and most complex in history. This period will see dozens of blockbuster drugs, including some of the best-selling medicines of all time, lose their market exclusivity. For strategists, portfolio managers, and business development leaders, understanding the composition of this wave is not just an academic exercise; it is the essential first step in charting a course through the turbulent years ahead.
A Cliff of Unprecedented Scale and Complexity
The sheer scale of the revenue at risk is breathtaking. Conservative estimates project that nearly 70 high-revenue products will face new competition, exposing anywhere from $236 billion to over $300 billion in annual global sales to the erosive forces of generic and biosimilar entry.5
What makes this impending cliff fundamentally different from those of the past is its composition. Previous cliffs, like the one that saw the fall of Lipitor and Plavix, were dominated by small-molecule drugs. The 2025-2030 wave, however, is characterized by the expiration of patents on a host of immensely successful and complex biologic drugs.58 Mega-blockbusters like Merck’s Keytruda, BMS’s Opdivo, Johnson & Johnson’s Stelara, and Regeneron’s Eylea are all on the list.57 This introduces a new layer of complexity, as the path to market for their “generic” counterparts—biosimilars—is more challenging, more expensive, and governed by the distinct legal framework of the BPCIA and its strategic “patent dance.”
The table below provides a snapshot of some of the most significant products facing U.S. patent expiration in the coming years, consolidating data to create a strategic roadmap of the key threats and opportunities on the horizon.
Table 1: Top Blockbuster Drugs Facing U.S. Patent Expiration (2025-2029)
| Drug Name | Company | Primary Indication(s) | 2024 Global Sales (Approx. $B) | Expected U.S. Expiration Year |
| Keytruda (pembrolizumab) | Merck | Multiple Cancers (Lung, Melanoma, etc.) | $29.5 | 2028 |
| Opdivo (nivolumab) | Bristol Myers Squibb | Multiple Cancers (NSCLC, RCC, etc.) | $9.3 | 2028 |
| Darzalex (daratumumab) | Johnson & Johnson | Multiple Myeloma | $11.67 | 2029 |
| Stelara (ustekinumab) | Johnson & Johnson | Psoriasis, Crohn’s Disease | $10.0 | 2025 |
| Eylea (aflibercept) | Regeneron / Bayer | Wet AMD, Macular Edema | $9.0 | 2025 |
| Xarelto (rivaroxaban) | Bayer / Janssen (J&J) | Anticoagulant | $4.5 | 2026 |
| Eliquis (apixaban) | Bristol Myers Squibb / Pfizer | Anticoagulant | $12.0 | 2026 |
| Trulicity (dulaglutide) | Eli Lilly | Type 2 Diabetes | $5.3 – $7.0 | 2027 |
| Ocrevus (ocrelizumab) | Genentech (Roche) | Multiple Sclerosis | $7.6 | 2029 |
| Cosentyx (secukinumab) | Novartis | Psoriasis, Psoriatic Arthritis | $5.19 | 2029 |
| Perjeta (pertuzumab) | Genentech (Roche) | HER2+ Breast Cancer | $4.3 | 2025 |
| Kadcyla (ado-trastuzumab emtansine) | Genentech (Roche) | HER2+ Breast Cancer | $2.31 | 2026 |
| Taltz (ixekizumab) | Eli Lilly | Psoriasis, Psoriatic Arthritis | $3.2 | 2026 |
| Repatha (evolocumab) | Amgen | Hypercholesterolemia | $2.22 | 2027 |
| Enbrel (etanercept) | Amgen | Rheumatoid Arthritis | $3.0 | 2029 (US) |
Data compiled from multiple sources including.5 Sales figures and expiration dates are estimates and may vary based on ongoing litigation, settlements, and other factors.
This table is more than just a list; it is a strategic battle map. For an innovator, it highlights the primary threats to its portfolio. For a biosimilar or generic developer, it is a menu of the most lucrative opportunities. The sheer size of the prizes—a drug like Keytruda with nearly $30 billion in annual sales presents a fundamentally different scale of opportunity than a $2 billion drug—allows for immediate strategic prioritization and resource allocation for the decade to come.
The Paradoxical “Biosimilar Void”
While the list of expiring blockbusters presents a massive opportunity, a critical counter-narrative has emerged: the “biosimilar void.” A recent, startling report from the IQVIA Institute for Human Data Science revealed that a vast majority—potentially as high as 90%—of the 118 biologic drugs losing exclusivity in the next decade currently have no publicly disclosed biosimilars in development.
This gap is not accidental. It is the result of significant economic and regulatory hurdles that make biosimilar development a far more challenging proposition than traditional generic manufacturing. The key barriers include :
- High Development Costs: Developing a biosimilar is an expensive undertaking, with costs ranging from $100 million to $250 million, compared to just a few million for a simple generic. This high barrier to entry makes the investment risky.
- Regulatory Complexity: The BPCIA approval pathway, while abbreviated, is still far more extensive and complex than the ANDA process, requiring significant analytical, preclinical, and often clinical studies to prove biosimilarity.
- Low Return on Investment for Niche Products: The high development cost creates a threshold effect. For a biosimilar to be commercially viable, the reference biologic typically needs to be a “mega-blockbuster” with multi-billion dollar annual sales. This leaves a significant market of “mid-tier” biologics (those with sales between $500 million and $2 billion) and, especially, orphan drugs for rare diseases, largely uncontested post-patent expiration. Of the biologics with orphan indications set to lose exclusivity, 88% have no biosimilars in the pipeline.
This “biosimilar void” represents both a market failure and a profound strategic opportunity. The current model of biosimilar development is not economically feasible for a huge swath of the biologics market. This leaves a multi-billion-dollar valley of opportunity completely untapped. The company that can innovate the biosimilar development or manufacturing process—perhaps through new platform technologies, AI-driven analytics, or more efficient clinical trial designs—to profitably target these mid-tier and orphan biologics will not just be competing in the current market; it will be creating an entirely new one. Cracking the “development cost” nut for biosimilars is the next great frontier in pharmaceutical competition, with the potential to unlock a vast and currently non-competitive landscape.
Section 10: Brand-Name Defense Playbook: Strategies to Mitigate Revenue Loss
For an innovator company, the period leading up to a Loss of Exclusivity (LOE) is a time of intense strategic planning and defensive maneuvering. The goal is not to halt the inevitable but to manage the descent—to soften the landing from the patent cliff, maximize the remaining value of the franchise, and build a bridge to the company’s next generation of products. This requires a sophisticated, multi-pronged playbook that combines commercial, legal, and R&D strategies.
Pre-LOE Revenue Maximization: The Surge
In the 12 to 18 months immediately preceding a patent expiration, a common and often effective tactic is “surge pricing.” This involves implementing a series of systematic, planned price increases on the branded product. Rather than one large, headline-grabbing hike, companies typically opt for several smaller increases throughout the year. The objective is simple: to maximize earnings from the product during its final months of monopoly pricing, extracting as much value as possible before the floodgates of generic competition open and prices collapse.
Lifecycle Management: The Art of “Evergreening”
The core of any long-term defensive strategy is lifecycle management, a practice often referred to by its more critical name, “evergreening.” This involves obtaining new, secondary patents on incremental improvements or modifications to an existing drug, with the aim of extending its period of market exclusivity beyond the expiration of the original composition of matter patent.17 These strategies are diverse and can include:
- New Formulations: This is one of the most common tactics. It can involve creating an extended-release (ER) or long-acting version of a drug that offers more convenient once-daily dosing, or developing a new dosage form, such as a liquid or a chewable tablet for patients who have difficulty swallowing pills.17 A successful example is GlaxoSmithKline’s Lamictal, where a patent on chewable tablets extended the product’s life by years.
- New Indications: A company may conduct new clinical trials to prove its drug is effective for a new disease or condition. If successful, this new method of use can be patented, creating a new stream of protected revenue.17
- Combination Products: This strategy involves combining the original drug with another medication into a single, fixed-dose combination pill. This new combination can be patented as a novel invention, encouraging patients to switch from the original single-agent therapy.
- “Product Hopping”: This is a more aggressive and controversial tactic. As the patent on the original product nears expiration, the innovator company heavily markets a “new and improved” version (e.g., an extended-release formulation) and may even pull the original version from the market. This can effectively force patients and physicians to “hop” to the new, patent-protected product, starving the imminent generic of its market.65
Patient and Portfolio Switching Strategies
Beyond modifying the drug itself, innovators also focus on strategically managing their patient base and product portfolio. This can involve:
- Switching to a Next-Generation Product: The ideal defensive strategy is to have a superior, next-generation follow-on product ready to launch before the original drug’s patent expires. The company can then invest heavily in marketing to switch patients to the new, patent-protected therapy, effectively migrating the revenue stream from the old asset to the new one.
- Over-the-Counter (OTC) Switch: For some drugs, a viable strategy is to switch the product from prescription-only to over-the-counter status before patent expiration. While this means lower prices and margins, it allows the company to leverage its established brand recognition and consumer loyalty to maintain a dominant market share in the OTC space, fending off private-label generic competitors.16
Legal and Regulatory Defenses
Finally, legal and regulatory tactics remain a key part of the defensive playbook. Innovator companies often engage in patent litigation against generic challengers, leveraging the 30-month stay provided by the Hatch-Waxman Act to delay generic entry, even if the lawsuit is ultimately unsuccessful.10 The strategic building of a “patent thicket”—a dense web of overlapping secondary patents—is designed to make such litigation more complex, expensive, and time-consuming for a generic challenger, acting as a powerful deterrent.
However, the practice of evergreening is a double-edged sword. While it can be highly effective in extending a product’s commercial life—one Swiss study found that evergreening strategies were successful in maintaining market share and actually contributed to increased overall healthcare costs —it also carries significant legal and reputational risk.
There is a growing backlash against what are perceived as anti-competitive abuses of the patent system. The landmark legal case involving Novartis’s cancer drug Gleevec in India is a prime example. India’s Supreme Court rejected a patent on a modified form of the drug, ruling that it lacked “enhanced therapeutic efficacy” over the original substance, setting a high bar for what constitutes genuine innovation.21 In the U.S., new legislation like the Affordable Prescriptions for Patients Act is being advanced specifically to curb practices like patent thicketing and product hopping.67
This shifting landscape suggests that the tolerance for patenting trivial modifications is waning. The most sustainable and defensible lifecycle management strategy is no longer just about what is legally patentable, but about what is clinically and economically justifiable. The focus for innovators must shift from making minor tweaks that can pass muster at the patent office to developing follow-on products that offer genuine, demonstrable improvements in efficacy, safety, or convenience—improvements that can be defended not just to lawyers, but to the physicians, payers, and patients who ultimately determine a drug’s value in the marketplace.
Section 11: Generic and Biosimilar Offense Playbook: Strategies for Market Capture
While innovators focus on defense, generic and biosimilar manufacturers are perpetually on offense. Their world is one of high-volume, low-margin competition where operational excellence, strategic timing, and regulatory acumen are the keys to victory. Success is not just about producing a copy of a drug; it’s about mastering a complex system to capture market share rapidly and efficiently. The offensive playbook for these companies is built on a foundation of smart portfolio selection, regulatory prowess, and a highly optimized supply chain.
The First Move: Strategic Portfolio Selection
The most critical decision a generic company makes is which products to pursue. With limited R&D and legal resources, portfolio selection is a high-stakes process that dictates the company’s future profitability. This decision is a multi-faceted analysis based on :
- Patent Expiration Timelines: Identifying drugs with key patents expiring in a viable timeframe.
- Market Size: Targeting drugs with significant sales to ensure a sufficient revenue opportunity.
- Technical Feasibility: Assessing the company’s capability to develop, formulate, and manufacture the drug, especially for more complex products.
- Competitive Landscape: Analyzing how many other generic competitors are likely to enter the market. A “first generic” opportunity is far more valuable than being the tenth entrant into an already crowded field.
Mastering the Game: The “First-to-File” Race
As established by the Hatch-Waxman Act, the single greatest prize for a generic challenger is the 180-day market exclusivity awarded to the “first-to-file” a Paragraph IV patent challenge. This makes the race to be the first to submit a “substantially complete” ANDA a primary strategic objective. Companies invest heavily in R&D and regulatory affairs to prepare their applications meticulously, aiming to be on the FDA’s doorstep the very first day it is legally possible to file. Winning this race can mean the difference between a highly profitable six-month duopoly and entering a market where prices have already been eroded by multiple competitors.
The Supply Chain as a Competitive Weapon
In a business where price margins are razor-thin, operational efficiency is not just a goal; it is a weapon. Generic companies face the daunting task of meeting customer expectations for near-perfect service levels (often 99% or higher) and rapid delivery (24-48 hours), all while managing highly volatile demand and keeping inventory to a minimum to control costs.
The traditional pharmaceutical supply chain is often ill-suited for this environment. A comparison to the Fast-Moving Consumer Goods (FMCG) industry is telling: the average generic company operates with three to five times the inventory of a consumer goods company, yet has a forecast accuracy that is ten percentage points lower. This highlights a massive opportunity for competitive differentiation through supply chain excellence.
Leading generic companies are increasingly adopting strategies from the more mature FMCG sector to build agile and responsive operations 71:
- End-to-End Visibility: Implementing IT systems that provide real-time visibility into demand, inventory levels, and manufacturing status across the entire global network. This often involves a central “control tower” that can proactively manage the supply chain.
- Postponement Strategies: Delaying the final stages of manufacturing, such as packaging and labeling, until the product is closer to the final market. A company might ship bulk, unpackaged tablets to a regional hub, and then package them specifically for different countries as orders come in. This decouples bulk production from volatile market-specific demand, allowing for more stable and efficient manufacturing runs.
- Deep Customer Collaboration: Working closely with large distributors and retail pharmacy chains to share forecast data and gain visibility into their inventory levels. This allows the generic company to better anticipate demand shocks (e.g., a competitor’s stockout) and proactively shape demand to smooth out volatile ordering patterns.
For a modern generic company, the supply chain is no longer a back-office cost center; it is a core source of competitive advantage. In a market where price differences can be minimal, the ability to reliably supply the market when a competitor cannot, or to flexibly manage the massive demand swings of a government tender contract, can win more sustainable market share than a slightly lower price. In the generic world, agility and reliability are the new currencies of competition. The company with the most sophisticated, data-driven, and reliable supply chain can offer superior service at a lower internal cost, creating a powerful competitive moat that is difficult for less operationally mature rivals to overcome.
Evolving Business Models: Beyond the Pill
Finally, the most forward-thinking generic companies are looking beyond their traditional role as high-volume manufacturers for developed markets. They are exploring new business models, including strategic partnerships and licensing agreements, to expand their reach. A significant opportunity lies in launching products in low- and middle-income countries (LMICs), where the original brand-name drug may never have been widely available or accessible. By adapting products and developing viable local business models, these companies are not only tapping into new growth markets but also playing a crucial role in expanding global access to essential medicines.
Section 12: The Power of Foresight: Leveraging Patent Data for Competitive Intelligence
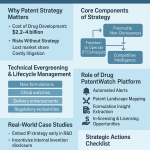
In the intricate and high-stakes environment of the pharmaceutical industry, information is power. The ability to anticipate market events, track competitor movements, and identify opportunities before they become obvious is what separates market leaders from followers. At the heart of this strategic foresight lies the discipline of competitive intelligence (CI), and its most potent raw material is patent data. Turning this vast and complex data into actionable intelligence is a critical capability for both innovator and generic firms.
The Orange Book: From Clinical Reference to Strategic Database
The primary tool for this work in the U.S. market is the FDA’s Orange Book. Before the Hatch-Waxman Act of 1984, the Orange Book was primarily a clinical reference. However, the Act’s mandate that innovators list all relevant patents and regulatory exclusivities for their approved drugs transformed it into an indispensable CI database. It provides a public, transparent record of the intellectual property barriers protecting every brand-name drug, serving as the starting point for nearly all strategic planning related to patent expiration.
Sophisticated CI teams use the Orange Book to perform several core activities:
- Tracking Patent Expiration Timelines: This is the most fundamental application. It involves systematically monitoring the expiration dates of all patents listed for a target drug, including any Patent Term Extensions (PTEs) or pediatric exclusivities that may have been granted. This allows for the creation of precise timelines for potential market entry.18
- Identifying Generic and Biosimilar Opportunities: By analyzing the Orange Book, companies can identify attractive targets for development. This analysis goes beyond just the expiration date to assess the complexity of the “patent thicket,” the number and type of patents that would need to be challenged or designed around, and the size of the market prize.
- Monitoring Litigation Activity: The Orange Book ecosystem provides early warning signals of competitive threats. When a generic manufacturer files an ANDA with a Paragraph IV certification, it is a public event. Tracking these filings and the subsequent patent infringement lawsuits provides a real-time view of who is challenging which patents, offering crucial insights into imminent competition and the potential for at-risk launches.11
- Conducting Patent Landscaping: Advanced CI involves combining Orange Book data with information from broader patent databases (like those from the USPTO). This allows for “patent landscaping,” a process of creating visual maps of the entire intellectual property terrain for a given therapeutic area. This can reveal which companies own the dominant patents, how patents are related to one another, and, most importantly, where the “white space” might be for future innovation and product development.
Commercial Platforms: Sharpening the Focus
While the Orange Book provides the raw data, sifting through it can be a complex and time-consuming task. This has given rise to specialized commercial intelligence platforms that aggregate, analyze, and visualize this information, making it more accessible and actionable. Services like DrugPatentWatch provide robust platforms designed specifically for pharmaceutical CI. They offer integrated tools and adaptive reports that help companies anticipate generic entry, track the momentum of launches by monitoring authorized generic activity, follow litigation in real-time, and assess the competitive landscape for both small molecules and biologics. These platforms streamline the monitoring process, allowing strategic teams to focus their energy on analysis and decision-making rather than data collection.75
The Next Frontier: Predictive Analytics in Litigation
The next evolution in pharmaceutical CI is the move from reactive monitoring to proactive forecasting, particularly in the realm of litigation. A patent lawsuit is not a random event; it is a process rich with data and patterns. By systematically analyzing historical litigation outcomes, companies can build sophisticated predictive models.
This goes far beyond simply noting that a lawsuit has been filed. A forward-thinking CI team can dissect the case, analyzing factors such as:
- The specific type of patent being challenged (e.g., composition of matter vs. a more tenuous formulation patent).
- The specific patent claims at the heart of the dispute.
- The historical track record of the law firms representing both the innovator and the generic challenger.
- The legal precedents and past rulings of the specific court and judge overseeing the case.
By applying data science and machine learning techniques to a large dataset of past litigation, a company can begin to model the probable outcome of a new case. They can assign a quantitative probability to a generic challenger’s likelihood of success. This probabilistic forecast is an immensely powerful strategic tool. It allows a company to make more nuanced risk assessments for its own portfolio, better evaluate the threat posed by a competitor, and make more informed decisions about capital allocation, R&D investment, and potential at-risk launch scenarios. This is the future of competitive intelligence: transforming legal data from a historical record into a predictive weapon.
Section 13: The Ecosystem’s Influence: PBMs, Patients, and Payers
The success or failure of a drug in the post-exclusivity market is not decided in a vacuum. The battle between the innovator and the generic/biosimilar manufacturers is profoundly influenced by a complex ecosystem of powerful external stakeholders. Two of the most influential groups are Pharmacy Benefit Managers (PBMs), the powerful gatekeepers who control market access, and patients, whose perceptions, behaviors, and adherence patterns can ultimately determine a product’s fate. Understanding their motivations and influence is critical for any company seeking to compete effectively.
The PBM: The Market’s Powerful Middleman
Pharmacy Benefit Managers are one of the most powerful and least understood players in the U.S. healthcare system. These large companies act as middlemen, hired by health insurers, large employers, and government plans to manage their prescription drug benefits.77 Their influence on the generic drug market is immense, primarily through three key business practices:
- Formulary Design and Tiering: PBMs create and maintain formularies, which are the lists of drugs that an insurance plan will cover. They typically group drugs into tiers, with each tier having a different patient co-payment. Tier 1 is usually reserved for low-cost preferred drugs, almost always generics, and has the lowest co-pay. Higher tiers are for preferred brands and non-preferred brands, with progressively higher co-pays.78 This tiered structure is a powerful tool to steer patients and physicians toward the most cost-effective options, driving the rapid uptake of generics.
- The Rebate System: PBMs negotiate with brand-name drug manufacturers to secure large rebates (discounts) in exchange for placing a brand’s drug on a favorable formulary tier.77 This practice, however, can create what critics call a “perverse incentive.” Because rebates are often calculated as a percentage of a drug’s high list price, a PBM may be financially motivated to favor a high-cost brand drug that offers a large rebate over a low-cost generic that offers little or no rebate. The PBM’s profit may be greater with the rebated brand, even if the net cost to the health plan and the patient is higher.
- Spread Pricing: This practice is particularly relevant for generic drugs. Spread pricing occurs when a PBM charges the health plan a certain price for a dispensed generic drug but reimburses the pharmacy a lower amount for that same drug. The PBM then pockets the difference, or the “spread”.77 This allows PBMs to generate significant profit from generics, but it means that the full cost savings from the low-priced generic are not passed on to the payer or the patient. One study found that PBMs can make four times more in gross margin from generics than from brands, largely due to this practice.
The generic drug market is therefore not a simple two-player game between the innovator and the generic firm. It is a three-player game, and the PBM is often the most powerful player on the board. A generic product’s success is determined less by its absolute price and more by its “formulary position,” which is dictated by the PBM’s complex and often opaque financial incentives. For a generic company, securing favorable formulary placement is the key to unlocking market access, which means its most important negotiation is often not with the pharmacy over wholesale price, but with the PBM over the terms of its inclusion in the formulary.
The Patient: The Final Arbiter of Success
While PBMs control access, the patient is the ultimate consumer, and their perceptions and behaviors are a critical factor in a generic’s success.
- The Psychology of the Switch: The transition from a familiar brand-name drug to a generic can be a source of anxiety and confusion for patients. A lack of awareness about the FDA’s rigorous standards for generic approval can lead to hesitation and suspicion. If patients believe the generic is inferior, they may be less likely to take it as prescribed, leading to non-adherence and potentially worse health outcomes.82 Medication adherence is a critical factor in managing chronic disease and reducing overall healthcare costs, so any factor that disrupts it is a serious concern.
- The Importance of Physical Appearance: Patients are highly sensitive to the physical characteristics of their medication. Numerous studies have shown that an unexpected change in a pill’s shape, color, or size can cause confusion and lead patients to believe they have received the wrong medicine. This can result in them stopping their medication altogether. One randomized controlled trial found that a generic label alone could negatively affect treatment adherence and even lead to patients reporting higher levels of pain, a powerful demonstration of the nocebo effect.
- The Power of Cost Savings: On the other hand, the primary driver of generic use—lower cost—is a powerful motivator for adherence. Higher out-of-pocket costs are consistently associated with decreased use of prescription drugs. The significantly lower co-pays for generics make medications more affordable, which generally improves a patient’s ability to consistently fill their prescriptions and adhere to their treatment regimen.
This complex interplay of factors underscores the importance of communication. Pharmacists and physicians play a crucial role in managing the switch to a generic. By proactively informing patients about the change, explaining the bioequivalence and rigorous FDA standards, and reassuring them about the safety and efficacy of the generic, healthcare providers can significantly increase patient confidence and ensure continuity of care.
Section 14: The Shifting Legal Landscape: The Future of Pharmaceutical Patents
The delicate balance of the Hatch-Waxman Act, which has governed the pharmaceutical patent landscape for nearly four decades, is facing its most significant challenge in a generation. A growing chorus of criticism from policymakers, payers, and patient advocates, combined with a series of bipartisan legislative and regulatory proposals, is threatening to rewrite the rules of the game. The primary targets of these reforms are long-standing innovator strategies perceived as anti-competitive, such as “patent thickets” and “product hopping,” which critics argue are used to unfairly delay the entry of lower-cost generic and biosimilar drugs.67
The Legislative Pushback: The Affordable Prescriptions for Patients Act
A leading example of this new legislative environment is the Affordable Prescriptions for Patients Act, a bipartisan bill that passed the U.S. Senate with unanimous consent in July 2024.67 The bill’s stated purpose is to “impose limitations on patent litigation involving biological products” to accelerate biosimilar market entry and lower drug prices.
Its key provision directly targets the “patent thicket” strategy used in biosimilar litigation. Under the proposed law, when an innovator sues a biosimilar applicant for patent infringement, it would be limited in the number and type of patents it can assert in the lawsuit. Specifically, the innovator could assert no more than 20 patents that meet certain criteria, such as having been filed more than four years after the biologic drug was first approved, or claiming a manufacturing process that the innovator does not actually use itself.67
This cap is designed to force innovators to litigate only their strongest and most relevant patents, rather than burying a biosimilar applicant in a legal war of attrition over dozens or even hundreds of weaker, secondary patents. While the bill includes exceptions and allows courts to expand the limit for “good cause,” its intent is clear: to streamline and simplify patent litigation, thereby reducing the barriers to entry for biosimilars.
The Regulatory Squeeze: The USPTO’s Proposed Rule Change
In parallel with legislative efforts, regulatory agencies are also taking action. The U.S. Patent and Trademark Office (USPTO) has proposed a significant rule change aimed at dismantling patent thickets through the mechanism of “terminal disclaimers”.
A terminal disclaimer is a tool innovators use to get around “obviousness-type double patenting” rejections. It allows them to obtain a later patent on a modification of an earlier invention, provided they agree that the later patent will expire at the same time as the earlier one. However, under the current system, even though the patents are linked for expiration, a generic challenger must still invalidate each patent separately in court.
The USPTO’s proposed rule would require that when a terminal disclaimer is filed, it must include language stating that the later patent will be unenforceable if the earlier patent it is linked to is ever found to be invalid or unenforceable. This could have a profound impact. It means that a generic challenger could potentially collapse an entire family of linked patents in a thicket by successfully invalidating just one key reference patent. This would dramatically lower the cost and complexity of litigation and incentivize innovators to focus on the quality and novelty of their inventions, not just the quantity of their patents.
The Innovator’s Defense: The PhRMA Counter-Argument
The pharmaceutical industry, represented by its powerful lobbying group PhRMA, has pushed back strongly against these proposed changes. Their core argument is that these reforms are not only unnecessary but will actively harm patients by stifling innovation.86
PhRMA contends that the current patent system is working as intended, having successfully created a market where over 90% of prescriptions are filled by low-cost generics. They argue that what critics dismiss as “evergreening” is in fact crucial post-approval innovation. This ongoing research leads to genuine patient benefits, such as new indications that allow a drug to treat more diseases, new formulations that improve safety or convenience, and new dosage forms that expand use to different patient populations (like children). Weakening the patent protections for these incremental but important improvements, they argue, would remove the incentive for companies to continue investing in their products after initial approval, leaving patients with fewer treatment options.
These proposed legal and regulatory reforms represent a potential tectonic shift in pharmaceutical strategy. For decades, the winning approach for many innovators was to build the largest and densest patent thicket possible, creating a formidable quantitative barrier to entry. The new rules, if enacted, would force a pivot from a quantity-based patent strategy to a quality-based one. The focus would no longer be on the sheer number of patents in a portfolio, but on the strength, novelty, and defensibility of a smaller number of core, high-quality patents. The entire calculus of lifecycle management and patent litigation would change, potentially heralding the end of an era where legal battles could be won by sheer volume.
Section 15: Conclusion: Navigating the Future in a Post-Exclusivity World
The expiration of a pharmaceutical patent is not an endpoint, but a transition point. It marks the end of a period of monopoly and the beginning of a new, intensely competitive market phase. As this report has detailed, this transition is the central, defining dynamic of the pharmaceutical industry—a predictable and recurring event that simultaneously poses an existential threat to innovators and creates immense opportunity for generic and biosimilar manufacturers, all while generating hundreds of billions of dollars in savings for the global healthcare system.
Success in this environment is not achieved by attempting to defy the gravity of the patent cliff, but by mastering the complex forces that shape it. It demands a strategic foresight that begins years, if not decades, before a patent’s expiration date. The most successful organizations, whether on the brand or generic side, understand that this is not a market for the reactive. It is a market for the proactive, the agile, and the deeply informed.
Our journey through this landscape has revealed a series of interconnected strategic realities:
- The “patent cliff” is a failure of planning, not a sudden crisis. The companies that thrive are those with proactive, long-term strategies to manage this scheduled economic event.
- The competitive battleground is not a single patent wall but a complex “fortress” of overlapping intellectual property and regulatory exclusivities. Navigating this fortress requires sophisticated intelligence and legal acumen.
- The Hatch-Waxman Act created more than a market; it created a strategic “game” with defined rules and prizes. Mastery of this regulatory gameplay is a core competency for any generic firm.
- The market itself is a multi-player ecosystem where the actions of one player create powerful ripple effects. The launch of an authorized generic is a “scorched earth” defense. An at-risk launch is a powerful signal of legal confidence. The fall of one blockbuster lowers the pricing benchmark for its entire therapeutic class.
- The new frontier of biologics and biosimilars has its own unique rulebook. The “patent dance” is a game of strategic signaling, where the opening move can reveal a company’s entire litigation posture.
- In a world of eroding margins and complex data, the most durable competitive advantages are no longer found solely in the lab. They are found in data-driven competitive intelligence, where predictive analytics can forecast litigation outcomes, and in hyper-efficient supply chains that deliver reliability and agility as a core value proposition.
- The market’s dynamics are heavily influenced by powerful third parties, particularly PBMs, whose financial incentives can dictate market access and pricing in ways that are often opaque and conflicted. Understanding and navigating these relationships is paramount.
- Finally, the legal and regulatory ground is shifting. A growing movement to curb perceived abuses of the patent system is forcing a strategic pivot from a focus on the quantity of patents to the quality and defensibility of innovation.
Looking ahead, the next decade will be defined by the great biologic patent cliff and the rise of the biosimilar market. This market is poised for explosive growth, with forecasts predicting it will reach over $76 billion by 2030.59 Yet, this growth is challenged by the paradoxical “biosimilar void,” where the high cost of development leaves a vast, multi-billion-dollar segment of the biologics market uncontested. The companies that will lead the next era of pharmaceutical competition will be those that can solve this puzzle—those that can innovate the very process of development to make biosimilars for mid-tier and orphan drugs a commercial reality.
Ultimately, the ticking clock of patent expiration sets the rhythm for the entire industry. It is a force of creative destruction that clears the way for new innovations while making established therapies accessible to all. The future will belong not to those who fear this rhythm, but to those who learn to conduct it, transforming the inevitable challenge of patent loss into a durable and decisive competitive advantage.
Key Takeaways
- Patent Expiration is a Predictable Strategic Challenge, Not a Sudden Crisis: The “patent cliff” is a scheduled event. Companies that suffer a catastrophic revenue loss often do so due to a failure in long-term strategic planning, not an unforeseen market shock. Success requires proactive lifecycle management and portfolio diversification years in advance.
- The Hatch-Waxman Act Created a Strategic “Game”: The U.S. generic market operates under a complex set of rules established by the Hatch-Waxman Act. Key elements like the Paragraph IV certification, the 30-month stay, and the 180-day “first-to-file” exclusivity are not just administrative procedures but strategic moves in a high-stakes game that requires legal and regulatory mastery.
- Price and Market Share Erosion are Swift and Severe: Upon multi-generic entry, a brand-name drug can expect to lose 80-90% of its market share, with prices falling by 80% or more. This dynamic is the primary driver of savings for the healthcare system but represents the core threat that innovators must manage.
- Authorized Generics and At-Risk Launches are Powerful Strategic Weapons: Innovators use Authorized Generics (AGs) as a “scorched earth” defense to devalue the 180-day exclusivity prize for the first generic challenger. Conversely, generics use “at-risk” launches as a high-stakes gamble to gain early market entry and signal unwavering confidence in their legal position.
- The Biologic Frontier is Defined by the “Patent Dance” and the “Biosimilar Void”: The BPCIA governs the entry of biosimilars. Its “patent dance” is an optional, strategic choice that reveals a company’s litigation strategy. A major challenge is the “biosimilar void,” where high development costs ($100M-$250M) leave up to 90% of expiring biologics without a biosimilar competitor, creating a significant untapped market opportunity.
- Data Analytics and Supply Chain are Core Competitive Advantages: In this complex environment, turning patent and litigation data into predictive intelligence is a key differentiator. For generics operating on thin margins, a hyper-efficient, agile, and reliable supply chain is not a support function but a primary competitive weapon.
- PBMs are Powerful Gatekeepers: Pharmacy Benefit Managers (PBMs) wield immense power through formulary design. Their business practices, such as rebates and spread pricing, can create incentives that are not always aligned with the lowest net cost, making the PBM relationship a critical factor for market access.
- The Legal Landscape is Shifting to Favor Patent Quality over Quantity: New legislation and proposed regulatory rules are targeting “patent thickets” and “product hopping.” This signals a move away from a strategy based on the sheer volume of patents to one that requires innovators to defend a smaller number of high-quality, genuinely innovative patents.
Frequently Asked Questions (FAQ)
1. What is the difference between a drug’s statutory patent life and its effective patent life, and why is this distinction so important?
A drug’s statutory patent life is the full legal term of the patent, which is typically 20 years from the date the patent application is filed.10 However, this is highly misleading in a commercial context. The
effective patent life is the actual period a drug is on the market with exclusivity, which is much shorter—often 7 to 14 years.16 This is because the 20-year clock starts at filing, but a significant portion of that time (often 10-15 years) is consumed by lengthy R&D, clinical trials, and regulatory review before the drug can be sold. This distinction is critically important because it defines the limited window a company has to recoup its massive R&D investment, creating immense pressure to maximize revenue and driving strategies like “evergreening” to extend this commercial window.
2. How does the 180-day exclusivity for the “first-to-file” generic actually accelerate competition?
The 180-day exclusivity is a powerful incentive created by the Hatch-Waxman Act that acts as a catalyst for competition. It grants the first generic company that successfully challenges a brand’s patent a six-month period of protection from other generic competitors.22 This “prize” motivates generic firms to invest millions in litigation to challenge patents years before they would naturally expire. Without this incentive, most generics would simply wait for patents to expire, delaying the availability of lower-cost medicines. By encouraging and rewarding these early patent challenges, the 180-day rule accelerates the entire timeline of generic entry, bringing lower-cost drugs to patients faster and generating significant healthcare savings.
3. Why would a biosimilar developer choose not to participate in the “patent dance” if it leads to a more predictable legal process?
While participating in the “patent dance” under the BPCIA leads to a more orderly and predictable legal process by narrowing the number of patents litigated upfront, choosing to opt out is a calculated, aggressive strategy.44 A biosimilar developer might opt out if they believe the innovator’s “patent thicket” is fundamentally weak and contains many patents that are invalid or not infringed. By refusing to dance, they dare the innovator to sue on its entire portfolio at once. This can be a high-risk, high-reward move. If the biosimilar company is correct, it can expose the weakness of the innovator’s overall patent position early on. It signals extreme confidence and a willingness to engage in a broader, more chaotic legal battle from the start, which can sometimes pressure the innovator into a more favorable settlement.
4. What is the “spillover effect” of a blockbuster patent expiration, and how does it impact competing brand-name drugs?
The “spillover effect” refers to the market-wide impact that a major patent expiration has on its entire therapeutic class, not just the brand drug itself. When a blockbuster like Plavix goes off-patent, a cheap, effective generic becomes available. Payers and PBMs quickly make this low-cost generic the preferred first-line treatment in their formularies to control costs. This action fundamentally resets the competitive landscape. Other brand-name drugs in the same class, even if they are still on-patent, are now forced to compete not against another high-priced brand, but against a highly effective, low-cost generic. To maintain their formulary access and market share, these competing brands must offer significantly deeper rebates and discounts, which lowers their net price and erodes their profitability. The patent cliff for one drug, therefore, “spills over” and lowers the economic value of the entire therapeutic category.
5. What is the “biosimilar void” and what does it signify for the future of the pharmaceutical market?
The “biosimilar void” is a phenomenon where a vast majority—potentially up to 90%—of biologic drugs that are losing patent protection in the next decade have no biosimilar competitors in development. This is primarily because the cost of developing a biosimilar is extremely high (upwards of $100 million to $250 million), making it commercially viable only for “mega-blockbuster” drugs with multi-billion dollar sales. This leaves a huge, untapped market of mid-tier and orphan biologics without competition after their patents expire. This signifies both a market failure (as potential savings are not being realized) and a major strategic opportunity. The company or technology that can significantly lower the cost of biosimilar development will be able to unlock this multi-billion dollar uncontested market, potentially creating a new paradigm for competition and access in the biologics space.
References
- bailey-walsh.com, accessed July 28, 2025, https://bailey-walsh.com/news/patent-cliff-impact-on-pharmaceutical-industry/#:~:text=A%20patent%20cliff%20occurs%20when,in%20sales%20upon%20patent%20expiration.
- Patent Cliff: What It Means, How It Works – Investopedia, accessed July 28, 2025, https://www.investopedia.com/terms/p/patent-cliff.asp
- Patent cliff – Wikipedia, accessed July 28, 2025, https://en.wikipedia.org/wiki/Patent_cliff
- What is a patent cliff, and how does it impact companies? – Patsnap Synapse, accessed July 28, 2025, https://synapse.patsnap.com/article/what-is-a-patent-cliff-and-how-does-it-impact-companies
- Blockbuster Drugs on Patent Cliffs Research Report 2025 | – GlobeNewswire, accessed July 28, 2025, https://www.globenewswire.com/news-release/2025/07/28/3122199/0/en/Blockbuster-Drugs-on-Patent-Cliffs-Research-Report-2025-2030-Patent-Cliff-to-Be-Largest-Since-2010-Hitting-Blockbusters-Like-Keytruda-Eliquis-and-Darzalex.html
- The Patent Cliff: From Threat to Competitive Advantage – Esko, accessed July 28, 2025, https://www.esko.com/en/blog/patent-cliff-from-threat-to-competitive-advantage
- 5 Steps to Take When Your Drug Patent is About to Expire, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/5-steps-to-take-when-your-drug-patent-is-about-to-expire/
- What are Patent Cliffs and How Pharma Giants Face Them in 2024 – PatentRenewal.com, accessed July 28, 2025, https://www.patentrenewal.com/post/patent-cliffs-explained-pharmas-strategies-for-2024-losses
- The Patent Cliff’s Shadow: Impact on Branded Competitor Drug Sales – DrugPatentWatch, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/the-effect-of-patent-expiration-on-sales-of-branded-competitor-drugs-in-a-therapeutic-class/
- When does a drug patent expire? – Patsnap Synapse, accessed July 28, 2025, https://synapse.patsnap.com/article/when-does-a-drug-patent-expire
- The Role of Litigation Data in Predicting Generic Drug Launches – DrugPatentWatch, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/the-role-of-litigation-data-in-predicting-generic-drug-launches/
- Generic and Biosimilar Medicines Save $445 Billion in 2023 …, accessed July 28, 2025, https://accessiblemeds.org/resources/press-releases/generic-and-biosimilar-medicines-save-445-billion/
- Report: 2023 U.S. Generic and Biosimilar Medicines Savings Report …, accessed July 28, 2025, https://accessiblemeds.org/resources/reports/2023-savings-report-2/
- 40th Anniversary of the Generic Drug Approval Pathway | FDA, accessed July 28, 2025, https://www.fda.gov/drugs/cder-conversations/40th-anniversary-generic-drug-approval-pathway
- Generic Drug Access & Savings in the U.S., accessed July 28, 2025, https://accessiblemeds.org/wp-content/uploads/2024/12/2017-AAM-Access-Savings-Report-2017-web2.pdf
- Navigating pharma loss of exclusivity | EY – US, accessed July 28, 2025, https://www.ey.com/en_us/insights/life-sciences/navigating-pharma-loss-of-exclusivity
- When Do Drug Patents Expire: Understanding the Lifecycle of …, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/when-do-drug-patents-expire/
- The Strategic Value of Orange Book Data in Pharmaceutical …, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/the-strategic-value-of-orange-book-data-in-pharmaceutical-competitive-intelligence/
- Drug Patent Life: The Complete Guide to Pharmaceutical Patent Duration and Market Exclusivity – DrugPatentWatch, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/how-long-do-drug-patents-last/
- Comparative Analysis of Us, Uk And India Drug Patent Laws, accessed July 28, 2025, https://www.globalpatentfiling.com/blog/Comparative-Analysis-of-Us-Uk-And-India-Drug-Patent-Laws
- Patent Evergreening In The Pharmaceutical Industry: Legal Loophole Or Strategic Innovation? – IJLSSS, accessed July 28, 2025, https://ijlsss.com/patent-evergreening-in-the-pharmaceutical-industry-legal-loophole-or-strategic-innovation/
- Exclusivity and Generic Drugs: What Does It Mean? | FDA, accessed July 28, 2025, https://www.fda.gov/files/drugs/published/Exclusivity-and-Generic-Drugs–What-Does-It-Mean-.pdf
- Authorized Generics – AWS, accessed July 28, 2025, https://pfe-pfizercom-prod.s3.amazonaws.com/about/Authorized_Generics_2018.pdf
- www.fda.gov, accessed July 28, 2025, https://www.fda.gov/drugs/abbreviated-new-drug-application-anda/hatch-waxman-letters#:~:text=The%20%22Drug%20Price%20Competition%20and,Drug%2C%20and%20Cosmetic%20Act%20(FD%26C
- What is Hatch-Waxman? – PhRMA, accessed July 28, 2025, https://phrma.org/resources/what-is-hatch-waxman
- Hatch-Waxman Act – Westlaw, accessed July 28, 2025, https://content.next.westlaw.com/Glossary/PracticalLaw/I2e45aeaf642211e38578f7ccc38dcbee
- Small Business Assistance | 180-Day Generic Drug Exclusivity | FDA, accessed July 28, 2025, https://www.fda.gov/drugs/cder-small-business-industry-assistance-sbia/small-business-assistance-180-day-generic-drug-exclusivity
- Generic Drugs: Questions & Answers – FDA, accessed July 28, 2025, https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/generic-drugs-questions-answers
- “At-risk” generic launches can be unpredictable, accessed July 28, 2025, https://www.managedhealthcareexecutive.com/view/risk-generic-launches-can-be-unpredictable
- The Hatch-Waxman 180-Day Exclusivity Incentive Accelerates Patient Access to First Generics, accessed July 28, 2025, https://accessiblemeds.org/resources/fact-sheets/the-hatch-waxman-180-day-exclusivity-incentive-accelerates-patient-access-to-first-generics/
- The Law of 180-Day Exclusivity (Open Access) – Food and Drug Law Institute (FDLI), accessed July 28, 2025, https://www.fdli.org/2016/09/law-180-day-exclusivity/
- Drug Competition Series – Analysis of New Generic Markets Effect of Market Entry on Generic Drug Prices – HHS ASPE, accessed July 28, 2025, https://aspe.hhs.gov/sites/default/files/documents/510e964dc7b7f00763a7f8a1dbc5ae7b/aspe-ib-generic-drugs-competition.pdf
- Price Declines after Branded Medicines Lose Exclusivity in the US – IQVIA, accessed July 28, 2025, https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/price-declines-after-branded-medicines-lose-exclusivity-in-the-us.pdf
- How Are Generics Affecting Drug Prices? – Cato Institute, accessed July 28, 2025, https://www.cato.org/regulation/winter-2019-2020/how-are-generics-affecting-drug-prices
- Generic pharmaceutical price decay – Wikipedia, accessed July 28, 2025, https://en.wikipedia.org/wiki/Generic_pharmaceutical_price_decay
- Understanding Patent Expiries and Their Impact on Drug Prices – East Street Pharmacy, accessed July 28, 2025, https://eaststreetpharmacy.com/understanding-patent-expiries-and-their-impact-on-drug-prices.html
- Authorized generics – Wikipedia, accessed July 28, 2025, https://en.wikipedia.org/wiki/Authorized_generics
- Understanding authorized generics-A review of the published clinical data – PubMed, accessed July 28, 2025, https://pubmed.ncbi.nlm.nih.gov/33829528/
- At-Risk Generic Drug Launch – Secretariat-intl.com, accessed July 28, 2025, https://secretariat-intl.com/engagements/at-risk-generic-drug-launch/
- Lessons From Mylan v Gilead for Those Seeking To “Launch at Risk” | Potter Clarkson, accessed July 28, 2025, https://www.potterclarkson.com/insights/lessons-from-mylan-v-gilead-for-those-seeking-to-launch-at-risk-and-those-seeking-to-stop-them/
- Launch-at-Risk Analysis – Secretariat-intl.com, accessed July 28, 2025, https://secretariat-intl.com/wp-content/uploads/2023/11/CaseStudy-Launch-at-Risk-Analysis-Draft.pdf
- No Free Launch: At-Risk Entry by Generic Drug Firms | NBER, accessed July 28, 2025, https://www.nber.org/papers/w29131
- No Free Launch: At-Risk Entry by Generic Drug Firms, accessed July 28, 2025, https://www.nber.org/system/files/working_papers/w29131/w29131.pdf
- Five key questions about the ‘patent dance’ answered – Generics and Biosimilars Initiative, accessed July 28, 2025, https://gabionline.net/switchlanguage/to/gabi_online_en/policies-legislation/Five-key-questions-about-the-patent-dance-answered
- Biosimilar Patent Dance: BPCIA Framework & Litigation Guide – Effectual Services, accessed July 28, 2025, https://www.effectualservices.com/article/biosimilar-patent-dance
- A Comparison of US, Europe, Japan and India Biosimilar Regulation, accessed July 28, 2025, https://www.ijdra.com/index.php/journal/article/download/745/395
- What Is the Patent Dance? | Winston & Strawn Law Glossary …, accessed July 28, 2025, https://www.winston.com/en/legal-glossary/patent-dance
- Patent Dance Insights: A Q&A on Reducing Legal Battles in the Biosimilar Landscape, accessed July 28, 2025, https://www.centerforbiosimilars.com/view/patent-dance-insights-a-q-a-on-reducing-legal-battles-in-the-biosimilar-landscape
- Case Note: Sandoz v. Amgen – Food and Drug Law Institute (FDLI), accessed July 28, 2025, https://www.fdli.org/2017/08/case-note-sandoz-v-amgen/
- The Biosimilar Patent Dance What Can We Learn From Recent …, accessed July 28, 2025, https://www.biosimilardevelopment.com/doc/the-biosimilar-patent-dance-what-can-we-learn-from-recent-bpcia-litigation-0001
- Federal Circuit Sides With Biosimilar Developer Sandoz in Landmark Decision, accessed July 28, 2025, https://www.centerforbiosimilars.com/view/federal-circuit-sides-with-biosimilar-developer-sandoz-in-landmark-decision
- Amgen v. Sandoz: The Supreme Court’s First Biosimilars Ruling | Mintz, accessed July 28, 2025, https://www.mintz.com/insights-center/viewpoints/2017-06-14-amgen-v-sandoz-supreme-courts-first-biosimilars-ruling
- Pfizer’s 180-Day War for Lipitor | PM360, accessed July 28, 2025, https://www.pm360online.com/pfizers-180-day-war-for-lipitor/
- Another Lurking Patent Cliff: Industry Challenges and Strategies for the Future – Medium, accessed July 28, 2025, https://medium.com/@gianlucaradesich/another-lurking-patent-cliff-industry-challenges-and-strategies-for-the-future-ef73ca405aa1
- 10 largest U.S. patent losses | Fierce Pharma, accessed July 28, 2025, https://www.fiercepharma.com/special-report/10-largest-u-s-patent-losses
- When does the patent for Clopidogrel expire? – Patsnap Synapse, accessed July 28, 2025, https://synapse.patsnap.com/article/when-does-the-patent-for-clopidogrel-expire
- 2025 Pharmaceutical Pipeline: Major Patent Expirations Set to Transform Drug Market with Generics and Biosimilars – MedPath, accessed July 28, 2025, https://trial.medpath.com/news/011e13abab731ac2/2025-pharmaceutical-pipeline-major-patent-expirations-set-to-transform-drug-market-with-generics-and-biosimilars
- 15 Biologics are Going Off Patent (2025–2029) – Clival Database, accessed July 28, 2025, https://clival.com/blog/15-biologics-are-going-off-patent-2025-to-2029
- The golden era of biosimilars: patent expiration wave and their …, accessed July 28, 2025, https://mabxience.com/the-golden-era-of-biosimilars-patent-expiration-wave-and-their-impact-on-global-healthcare/
- Expected Patent Expiry Drugs List: Top Drugs Losing Patent Protection By 2030 – Artixio, accessed July 28, 2025, https://www.artixio.com/post/patent-expiry-alert-drugs-expected-to-lose-protection-in-the-next-five-years
- Biosimilars Markets Global Forecast Report 2025-2035 | – GlobeNewswire, accessed July 28, 2025, https://www.globenewswire.com/news-release/2025/07/24/3120835/0/en/Biosimilars-Markets-Global-Forecast-Report-2025-2035-Launch-of-Glp-1-Biosimilars-Increasing-Strategic-Partnerships-and-Collaborations-Growing-Focus-on-Advanced-R-D-Fueling-Opportun.html
- The Future of Top-Selling Biologics: Biosimilars on the Rise – Pharmacy Times, accessed July 28, 2025, https://www.pharmacytimes.com/view/the-future-of-top-selling-biologics-biosimilars-on-the-rise
- 25 High-Value Drugs Losing Patent Protection in 2025: What It Means for Healthcare, accessed July 28, 2025, https://biopharmaapac.com/analysis/60/5727/25-high-value-drugs-losing-patent-protection-in-2025-what-it-means-for-healthcare.html
- The Biosimilar Void: 90% of Biologics Coming Off Patent Will Lack Biosimilars, accessed July 28, 2025, https://www.centerforbiosimilars.com/view/the-biosimilar-void-90-of-biologics-coming-off-patent-will-lack-biosimilars
- Does Drug Patent Evergreening Prevent Generic Entry …, accessed July 28, 2025, https://www.drugpatentwatch.com/blog/does-drug-patent-evergreening-prevent-generic-entry/
- Evergreening Strategy: Extending Patent Protection, Innovation or Obstruction?, accessed July 28, 2025, https://kenfoxlaw.com/evergreening-strategy-extending-patent-protection-innovation-or-obstruction
- Senate Unanimously Passes Bipartisan Pharma Patent Reform Bill …, accessed July 28, 2025, https://newcityinsurance.com/senate-unanimously-passes-bipartisan-pharma-patent-reform-bill/
- Patented Drug Extension Strategies on Healthcare Spending: A Cost-Evaluation Analysis, accessed July 28, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3672218/
- U.S. Senate Passes Affordable Prescriptions for Patients Act of 2023 to Limit Number, Nature of Patents in Biosimilar Litigation – Sidley Austin LLP, accessed July 28, 2025, https://www.sidley.com/en/insights/newsupdates/2024/08/us-senate-passes-affordable-prescriptions-for-patients-act-of-2023
- Reforms targeting “patent thickets” would speed up the arrival of lower-cost drugs, accessed July 28, 2025, https://www.niskanencenter.org/reforms-targeting-patent-thickets-would-speed-up-the-arrival-of-lower-cost-drugs/
- Low cost, high stakes: Five strategies for generic supply … – McKinsey, accessed July 28, 2025, https://www.mckinsey.com/~/media/McKinsey/Business%20Functions/Operations/Our%20Insights/Low%20cost%20high%20stakes%20Five%20strategies%20for%20generic%20supply%20chains/20150723_low_cost_high_stakes_opp_comp.pdf
- 7 Supply Chain Strategies Pharma Brands Can Use Against Generic Drugs, accessed July 28, 2025, https://supplychainbeyond.com/7-supply-chain-strategies-for-pharma-brands-vs-generics/
- Generics companies are exploring new ways to increase access to medicine, accessed July 28, 2025, https://accesstomedicinefoundation.org/news/generics-companies-are-exploring-new-ways-to-increase-access-to-medicine
- Patent Intelligence – IQVIA, accessed July 28, 2025, https://www.iqvia.com/solutions/commercialization/commercial-analytics-and-consulting/brand-strategy-and-management/patent-intelligence
- Integrated Scientific Computing and Information Technologies …, accessed July 28, 2025, https://www.iscitech.com/drugcustommarket.htm
- DrugPatentWatch 2025 Company Profile: Valuation, Funding & Investors | PitchBook, accessed July 28, 2025, https://pitchbook.com/profiles/company/519079-87
- PBM Regulations on Drug Spending | Commonwealth Fund, accessed July 28, 2025, https://www.commonwealthfund.org/publications/explainer/2025/mar/what-pharmacy-benefit-managers-do-how-they-contribute-drug-spending
- 5 Things To Know About Pharmacy Benefit Managers – Center for American Progress, accessed July 28, 2025, https://www.americanprogress.org/article/5-things-to-know-about-pharmacy-benefit-managers/
- A Blueprint for Pharmacy Benefit Managers to Increase Value – PMC – PubMed Central, accessed July 28, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2737824/
- GAO-12-371R, Drug Pricing: Research on Savings from Generic Drug Use, accessed July 28, 2025, https://www.gao.gov/assets/gao-12-371r.pdf
- The generic drug pricing game: What employers need to know. – Rightway, accessed July 28, 2025, https://www.rightwayhealthcare.com/blog/the-generic-drug-pricing-game
- Utilizing Generic Drug Awareness to Improve Patient Outcomes with …, accessed July 28, 2025, https://www.fda.gov/drugs/news-events-human-drugs/utilizing-generic-drug-awareness-improve-patient-outcomes-dr-sarah-ibrahim
- The impact of generic labels on the consumption of and adherence to medication: a randomized controlled trial – ResearchGate, accessed July 28, 2025, https://www.researchgate.net/publication/327602802_The_impact_of_generic_labels_on_the_consumption_of_and_adherence_to_medication_a_randomized_controlled_trial
- The impact of medication adherence on health outcomes and cost reduction, accessed July 28, 2025, https://wmpllc.org/ojs/index.php/jom/article/view/3870
- Medication Adherence and the Use of Generic Drug Therapies – PMC – PubMed Central, accessed July 28, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2918380/
- Patent policy changes proposed by USPTO and FDA would leave patients behind | PhRMA, accessed July 28, 2025, https://phrma.org/blog/patent-policy-changes-proposed-by-uspto-and-fda-would-leave-patients-behind
- New report: How intellectual property drives U.S. innovation and …, accessed July 28, 2025, https://phrma.org/blog/new-report-how-intellectual-property-drives-u-s-innovation-and-biopharma-s-impact
- Biosimilars Market Size to Hit $76.2 Billion by 2030 – Driving Value …, accessed July 28, 2025, https://www.prnewswire.com/news-releases/biosimilars-market-size-to-hit-76-2-billion-by-2030—driving-value-based-care-for-drugmakers-regulators–emerging-markets–the-research-insights-302495541.html
- Biosimilars Market Outlook 2025 – Chemxpert Database, accessed July 28, 2025, https://chemxpert.com/blog/biosimilars-market-outlook-2025?