Deconstructing the Crisis in Pharmaceutical R&D
For decades, the pharmaceutical industry has operated on a model of innovation that, while responsible for some of humanity’s greatest medical triumphs, is now groaning under the weight of its own inefficiencies. The traditional path of de novo drug discovery—the ground-up process of identifying a new target, designing a new molecule, and guiding it through years of rigorous testing—has become a high-stakes gamble with increasingly poor odds. Are we reaching the limits of this paradigm? The data paints a sobering picture.
Bringing a single new drug to market is a monumental undertaking, a journey that typically spans 10 to 17 years and consumes a staggering amount of capital.1 In 2016, the estimated average out-of-pocket cost per approved new compound stood at $1.4 billion, but when factoring in the cost of capital and the many failures that litter the path to success, the fully capitalized cost balloons to an astonishing $2.6 billion. This figure doesn’t even account for post-approval R&D, which pushes the total investment to nearly $2.8 billion. These costs are not static; they have been shown to increase at an annual rate of 8.5% above general price inflation, a trajectory that is simply unsustainable.
This colossal investment would perhaps be justifiable if success were common, but the opposite is true. The attrition rates in drug development are brutal. For every 5,000 compounds that show promise in preclinical testing, only five will ever be tested in humans, and of those, only one will ultimately receive regulatory approval. This translates to a failure rate of over 90% for drugs entering clinical trials, a figure that climbs to an even more daunting 97% for oncology drugs.4 Safety concerns alone account for approximately 30% of all drug failures in the clinical phase.
The result is a productivity crisis. The escalating costs and high failure rates mean that for every dollar spent on research and development, the industry, on average, now sees less than a dollar of value in return. This diminishing return on investment threatens the very engine of pharmaceutical innovation, making the industry a less desirable choice for investors and forcing companies to make increasingly conservative bets on blockbuster drugs for common diseases, leaving vast areas of unmet medical need unaddressed. This is the strategic chasm—a landscape of unsustainable costs, unacceptable risk, and slowing innovation—that has created not just an opportunity, but an urgent necessity for a new approach. Drug repurposing has emerged as the most powerful and rational response to this crisis, offering a pathway to revive innovation, manage risk, and, most importantly, deliver therapies to patients who have been left behind.
Defining Drug Repurposing: More Than Happy Accidents
Drug repurposing, known interchangeably as drug repositioning, reprofiling, or retasking, is a strategy centered on identifying new therapeutic uses for existing drugs that are outside the scope of their original, approved medical indication.9 This concept, which first appeared in the literature around 2004, has evolved significantly from its early days. It is a broad umbrella that covers several categories of compounds:
- Approved Drugs: Marketed drugs, including both branded and generic products, that are found to be effective for a new disease.
- Investigational Drugs: Compounds that have undergone clinical testing but failed to gain approval for their initial indication, often due to a lack of efficacy rather than safety concerns.
- Withdrawn or Shelved Assets: Drugs that were pulled from the market for safety reasons or discontinued during development for strategic or commercial reasons.12
The history of drug repurposing is punctuated by famous examples of serendipity—happy accidents where an unexpected clinical observation revealed a drug’s hidden potential. The story of sildenafil is a classic. Originally developed by Pfizer to treat hypertension and angina, researchers noted an unusual side effect in male participants during clinical trials, leading to its spectacular rebirth as Viagra, a blockbuster treatment for erectile dysfunction.9 Similarly, thalidomide, a drug with a tragic past as a sedative that caused severe birth defects, was later found to have potent immunomodulatory and anti-angiogenic properties, leading to its redemption as a cornerstone therapy for multiple myeloma and complications of leprosy.8
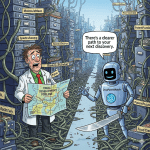
While these early successes were often opportunistic, the modern era of drug repurposing is defined by a fundamental shift from chance to strategy. The advent of powerful new technologies has transformed the field from an art of retrospective observation into a science of prospective prediction. Advanced bioinformatics, artificial intelligence (AI), network pharmacology, and a wealth of “omics” data (genomics, proteomics, transcriptomics) now allow researchers to systematically and rationally identify new drug-disease connections.9 This evolution is critical. It turns repurposing from a high-risk, occasional windfall into a predictable, scalable, and strategically vital component of the modern pharmaceutical R&D pipeline. It is no longer about stumbling upon hidden treasure; it’s about having a map that shows you exactly where to dig.
The Unassailable Value Proposition: Speed, Cost, and De-risked Development
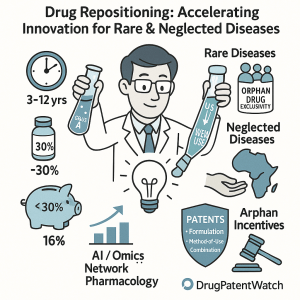
Why has drug repurposing moved from the periphery to the core of pharmaceutical strategy? The answer lies in its ability to fundamentally rewrite the brutal economics of drug development. It offers a compelling trifecta of advantages—accelerated timelines, drastically reduced costs, and a significantly de-risked development profile—that directly address the primary pain points of the traditional de novo model.4
Drastic Cost Reduction: The financial contrast is stark. Repurposing can slash R&D expenses by an estimated 50-60%.4 The average cost to bring a repurposed drug to market is estimated to be around $300 million, a fraction of the $2-3 billion required for a new chemical entity (NCE).1 In some cases, the costs can be even lower; one report estimated the average cost to relaunch a repositioned drug at just $8.4 million. This massive cost saving is achieved by leveraging the vast amount of work already completed for the drug’s original indication. The most expensive and resource-intensive early stages of development—such as extensive preclinical compound discovery, formulation, and Phase I safety and toxicity studies—are often bypassed because a wealth of existing data on the drug’s safety, pharmacology, and manufacturing processes is already available.4
Accelerated Timelines: Time is money, and in drug development, it’s a currency measured in years. Drug repurposing can shave 5 to 7 years off the conventional drug development timeline. While a new drug takes 10-15 years to reach the market, a repurposed candidate can often make the journey in just 3-12 years.1 This acceleration is a direct result of skipping the early-stage hurdles. Because the compound has already been tested in humans, researchers can often move directly into Phase II clinical trials to test for efficacy in the new indication, a significant shortcut that brings potential therapies to patients years sooner.
Higher Probability of Success: Perhaps the most critical advantage is the dramatically lower risk of failure. The primary reason drugs fail in clinical trials is unforeseen toxicity or safety issues. Repurposed drugs have a significant head start because their safety profiles are already well-characterized in humans.8 This “de-risking” has a profound impact on the probability of success. The approval rate for repurposed drugs that have completed Phase I trials can be as high as 30%, a threefold increase over the typical success rate of less than 10% for traditional NCEs.4 This fundamentally alters the risk-reward calculus for pharmaceutical investment, making repurposing projects far more attractive to both internal budget committees and external investors.
This is not merely an incremental improvement; it is a paradigm shift. The enormous sunk costs of a “failed” drug’s initial development are not lost. Instead, they are transformed into a valuable asset—a de-risked compound with a rich data package that can be acquired and leveraged by a repurposer for a fraction of the original investment. This reframes the R&D process from a series of independent, high-risk bets into a strategic ecosystem where the outputs of one process, even the failures, become the valuable inputs for another. For any business leader aiming to optimize an R&D portfolio, the economic argument is undeniable, as illustrated below.
| Feature | Traditional De Novo Drug Discovery | Drug Repurposing |
| Average Development Cost | >$2.5 billion 4 | ~$300 million (50-60% lower) 4 |
| Average Time-to-Market | 10–15 years 4 | 3–12 years (avg. 5-7 years shorter) |
| Probability of Success (from Phase I) | <10% 4 | ~30% |
| Key Development Stages Bypassed | None | Preclinical discovery, extensive toxicology, often Phase I safety trials |
| Primary IP Protection | Composition of Matter & Method of Use Patents | Primarily Method of Use; sometimes Formulation/Combination Patents |
| Commercial Exclusivity (US) | 5 years (New Chemical Entity) | 3 years (New Use/Product) or 7 years (Orphan Drug) 14 |
This stark contrast highlights why repurposing has become a strategic imperative. In an environment of punishingly high attrition rates, a dedicated repurposing program acts as a crucial portfolio management tool—a strategic hedge that provides a parallel development track with a much higher probability of success. By systematically screening their own shelved assets or actively seeking external opportunities, companies can generate a steady stream of lower-risk, mid-to-late-stage assets to balance the high-risk ventures in their innovative pipeline.14
The Two Fronts of Unmet Need: Rare vs. Neglected Diseases
While the strategic advantages of drug repurposing are universally applicable, its impact is most profound in areas where the traditional R&D model has unequivocally failed. Two such areas stand out: rare (or orphan) diseases and neglected tropical diseases (NTDs). Though often grouped together under the umbrella of “unmet medical needs,” they represent fundamentally different challenges that demand distinct strategic approaches. Understanding this dichotomy is the first step toward crafting an effective repurposing strategy. One is a problem of biological scarcity in high-value markets; the other is a problem of economic scarcity in low-resource settings.
Defining the Landscape: A Tale of Two Patient Populations
Rare/Orphan Diseases: In the United States, a rare disease is legally defined by the Orphan Drug Act of 1983 as a condition affecting fewer than 200,000 people.18 Europe uses a prevalence-based definition of not more than 5 in 10,000 people.20 While each disease is rare, collectively they are tragically common. There are an estimated 7,000 to 10,000 distinct rare diseases, affecting approximately 30 million people in the U.S. alone—nearly one in ten Americans—and a staggering 350 million people globally.19 The vast majority of these conditions—around 80%—are genetic in origin, often chronic, progressive, and life-threatening.22 Yet, for all this suffering, the therapeutic landscape is barren. It is estimated that a mere 5% to 10% of all rare diseases have a single FDA-approved treatment, leaving millions of patients and their families with little to no hope.22
Neglected Tropical Diseases (NTDs): The World Health Organization (WHO) defines NTDs as a diverse group of conditions caused by a variety of pathogens—viruses, bacteria, parasites, and fungi—that are primarily prevalent among impoverished communities in tropical and subtropical areas.27 This group includes diseases with unpronounceable names that are absent from the global health agenda, such as leishmaniasis, Chagas disease, and human African trypanosomiasis (sleeping sickness).28 These are diseases of poverty, thriving where access to clean water, sanitation, and healthcare is scarce.28 They affect more than 1 billion people worldwide, causing devastating health, social, and economic consequences that trap the world’s poorest populations in a vicious cycle of disease and poverty.29 They are “neglected” precisely because they afflict those with no political voice and no ability to pay, offering no commercial incentive for pharmaceutical investment.28
The strategic implications of this distinction are profound. For rare diseases, a potential market exists, often within well-developed healthcare systems. The challenge is scientific and logistical. For NTDs, the patient population is enormous, but a commercial market is entirely absent. The challenge is purely economic and humanitarian.
The Economics of Scarcity: The High-Stakes World of Orphan Drugs
The development of drugs for rare diseases—known as orphan drugs—is a landscape defined by daunting challenges. The very nature of these conditions creates immense hurdles for traditional R&D. Patient populations are not only small but also often highly heterogeneous in their clinical presentation and geographically dispersed, making the recruitment and execution of statistically significant clinical trials incredibly difficult and costly.33 Furthermore, for many rare diseases, there is a limited understanding of the natural history of the disease, making it hard to design trials and select appropriate endpoints.36
This combination of high R&D risk and a small target market creates a powerful disincentive for investment. Before the Orphan Drug Act, pharmaceutical companies simply “orphaned” these conditions, as there was no reasonable expectation that sales could ever recover development costs.19 To counteract this market failure, governments introduced powerful incentives, such as market exclusivity, tax credits, and grants, to make orphan drug development commercially viable.18
While these incentives have spurred the development of hundreds of new orphan drugs, they have also given rise to a unique “high price, low volume” economic model. To recoup the substantial investment from a small patient pool, approved orphan drugs command some of the highest prices in medicine. It is not uncommon for these therapies to cost upwards of $300,000 to $500,000 per patient, per year.3 For example, eculizumab for paroxysmal nocturnal hemoglobinuria can cost up to $500,000 annually, while Kalydeco for a subset of cystic fibrosis patients exceeds $300,000 per year.
This is where drug repurposing emerges as a powerful disruptive force. The entire economic justification for exorbitant orphan drug prices is predicated on the high cost and risk of de novo development. By leveraging an existing drug’s safety data and manufacturing processes, repurposing dramatically lowers this initial R&D investment. A recent study found that the capitalized clinical costs per approved orphan drug were significantly lower than for non-orphan drugs ($291 million vs. $412 million). This changes the economic equation entirely. It opens the door for companies to develop therapies for ultra-rare diseases that would be commercially unviable even with existing incentives. It also creates a competitive threat to incumbent high-priced orphan drugs, as a repurposed alternative could potentially enter the market at a lower price point, creating immense pressure on payers and providers.
The Economics of Poverty: The Humanitarian Imperative for NTDs
If the orphan drug market is a high-stakes commercial venture, the NTD space is a commercial void. There is little to no market-driven rationale for a pharmaceutical company to invest many years and billions of dollars into developing a drug for populations that cannot afford it. As a result, R&D for NTDs has historically been driven by a different set of actors: non-profit product development partnerships (PDPs) like the Drugs for Neglected Diseases initiative (DNDi), humanitarian organizations like Médecins Sans Frontières (MSF), and public-private partnerships funded by governments and philanthropic giants like the Bill & Melinda Gates Foundation.39
This ecosystem operates on a “no price, high volume” model, where the goal is not profit but public health impact. However, this model is fragile and dependent on a steady stream of funding, which is currently in jeopardy. Overall investment in R&D for neglected diseases fell from a peak of $4.7 billion in 2018 to $3.7 billion in 2023, threatening to halt progress on promising pipeline candidates that require sustained funding to reach patients.
“An analysis by Policy Cures Research estimated that every $1 invested in neglected disease research and development and developing life-saving products generates a societal and economic return of $405. Those figures reflect the impact of products — including drugs, vaccines, and diagnostic tests — that have come to market in the past 20 years, plus the anticipated impact of entirely new innovations between now and 2040. If funding stops, those gains simply won’t materialize.”
In this resource-constrained environment, drug repurposing is not just an alternative strategy; it is often the only viable strategy. It allows researchers to bypass the prohibitively expensive early stages of drug discovery and focus limited funds on clinical testing of existing, often off-patent, compounds. The strategic driver is not to disrupt a market, but to create a therapeutic solution where none could otherwise exist. It is the most efficient and cost-effective way to translate scientific knowledge into life-saving interventions for the world’s most vulnerable populations.
The incentives designed to stimulate NTD research, such as the FDA’s Priority Review Voucher (PRV) program, reflect this unique economic reality. The PRV program doesn’t make the NTD drug itself profitable. Instead, it creates a separate, tradable financial asset—the voucher—which can be sold to another company for a significant sum (often around $100 million) or used to expedite the review of a future blockbuster drug.41 The strategy for a company pursuing an NTD drug is therefore not centered on the market for that drug, but on the efficient capture and monetization of the PRV. This makes the speed and low cost of a repurposing approach particularly well-suited to the task.
The Modern Alchemist’s Toolkit: Technologies Driving Repurposing
The transformation of drug repurposing from a practice of fortunate observation to one of systematic, predictive science has been fueled by a technological revolution. The modern repurposing toolkit combines the brute-force power of high-throughput experimental screening with the sophisticated predictive capabilities of computational biology and artificial intelligence. This synergy allows researchers to generate and test hypotheses at a scale and speed that was unimaginable just a decade ago, systematically mining the world’s existing pharmacopeia for hidden therapeutic gems. Understanding this toolkit is essential for any organization aiming to build a competitive and efficient repurposing pipeline.
The Digital Revolution: Computational and In Silico Strategies
At the heart of modern repurposing lies the power of in silico analysis—the use of computational models to predict new drug-disease relationships before a single experiment is run in a lab. These approaches leverage vast repositories of biological and chemical data to identify promising candidates, drastically narrowing the search space and focusing resources on the most plausible hypotheses.44 Computational strategies can be broadly categorized into three main types.
Profile-Based Approaches: This strategy is built on the principle of pattern matching. It compares the unique “profile” or “signature” of a drug with the signature of a disease. If the patterns are complementary, a therapeutic connection is inferred. These profiles can be derived from several data types:
- Gene Expression Profiles: This is one of the most powerful methods. The core hypothesis is that an effective drug should reverse the gene expression changes caused by a disease.8 For example, if a disease causes certain genes to be over-expressed and others to be under-expressed, a promising drug candidate would do the opposite—down-regulating the over-expressed genes and up-regulating the under-expressed ones. Public databases like the Connectivity Map (cMap) contain the gene expression signatures of thousands of drugs, allowing researchers to computationally screen for these inverse relationships against the signatures of various diseases.
- Chemical Structure Profiles: Based on the pharmacological principle that similar structures often have similar biological activities, this method uses molecular docking and other chemoinformatic tools to predict new drug-target interactions. If the protein target of a known drug is structurally similar to a protein implicated in a different disease, that drug becomes a repurposing candidate.
- Side-Effect Profiles: The logic here is that drugs with similar side-effect profiles often share a similar mechanism of action or act on related biological pathways. By matching the adverse event profile of a drug to the symptom profile of a disease, researchers can uncover non-obvious therapeutic connections.44
Network-Based Approaches: Moving beyond simple one-to-one comparisons, network-based methods model the staggering complexity of human biology as an interconnected web, or network. In these models, nodes can represent drugs, proteins, genes, or diseases, and the edges represent the relationships between them (e.g., a drug binds to a protein, a protein interacts with another protein, a gene is associated with a disease).49 By applying sophisticated algorithms like random walks or label propagation to these massive networks, researchers can predict new links. For instance, the “guilt-by-association” principle suggests that if a drug’s targets are located in the same network “neighborhood” as the proteins associated with a particular disease, that drug is a strong candidate for repurposing for that disease.16
Data-Based Approaches: This strategy involves mining real-world data from vast textual and clinical databases to find evidence of new drug uses. Text-mining algorithms can scan millions of scientific publications and patents to identify co-occurrences of drug and disease names, suggesting a potential link. Similarly, analyzing large electronic health record (EHR) databases can reveal unexpected therapeutic effects; for example, if patients taking a specific drug for one condition show a statistically lower incidence of another disease, it points to a potential repurposing opportunity.
The AI Ascendancy: How Machine Learning is Predicting New Cures
If computational biology provides the strategic map for repurposing, then artificial intelligence (AI) and machine learning (ML) are the high-speed engines driving discovery. These technologies are uniquely suited to the core challenge of repurposing: finding the faint, complex signals hidden within massive, noisy, and heterogeneous datasets.53 AI is not just making the existing computational methods faster; it is enabling entirely new ways of generating hypotheses.56
AI’s impact is being felt across the entire repurposing pipeline:
- Predicting Drug-Target Interactions: Deep learning models can now analyze the 2D chemical structure of a drug, often represented as a simple text string (SMILES), and predict its binding affinity to various protein targets with remarkable accuracy. By training on vast databases of known interactions, these models learn the complex rules of molecular recognition, allowing them to screen entire drug libraries against new targets in silico.
- Integrating Multimodal Data: The true power of AI lies in its ability to learn from diverse data types simultaneously. An advanced AI platform can integrate genomic data (the genetic basis of a disease), transcriptomic data (how the disease affects gene expression), proteomic data (the proteins involved), chemical structure data, and clinical data from EHRs to build a holistic model of a disease.56 This allows the AI to identify connections that would be impossible for a human researcher to spot, such as predicting that a failed cancer drug might be effective for a rare neurological disorder because its off-target effects happen to modulate a key pathway in that disease.
- Accelerating Candidate Selection: AI-driven companies are already demonstrating the power of this approach. HealX, a UK-based company, uses its AI platform to identify and advance treatments for rare diseases, having already moved candidates for conditions like Fragile X syndrome into clinical trials. In the realm of neglected diseases, AI has been used to identify the antiarrhythmic drug amiodarone as a potential treatment for Chagas disease, showcasing its ability to find novel uses for existing medicines.
The rise of AI marks a pivotal moment for drug repurposing. It elevates the process from a data-mining exercise to a truly predictive science, increasing the quality, novelty, and ultimate success rate of the hypotheses being generated.
Grounding the Code in Biology: Experimental Validation
For all their predictive power, computational and AI-driven methods only generate hypotheses. These predictions must be rigorously tested and validated in the real world through experimental screening before they can advance toward the clinic. This experimental validation serves to confirm the in silico findings and provide the foundational biological data needed to justify a clinical trial.
High-Throughput Screening (HTS): HTS is a brute-force experimental approach that uses robotics and automation to test thousands of compounds against a specific biological target in a very short time.61 In the context of repurposing, instead of screening novel chemical libraries, researchers screen libraries of already-approved drugs (like the Broad Drug Repurposing Hub, which contains over 6,000 compounds). HTS is particularly useful when a specific, well-defined molecular target for a disease is known. The process can rapidly identify which existing drugs interact with that target, providing a list of “hits” for further investigation. The relationship with computational methods is symbiotic:
in silico predictions can drastically narrow the number of drugs that need to be screened experimentally, making HTS more focused, efficient, and cost-effective.
Phenotypic Screening: This approach represents a powerful alternative, especially when the precise molecular target of a disease is unknown.64 Instead of testing drugs against a single purified protein, phenotypic screening assesses their effect on a whole biological system—such as a cell culture or a model organism (e.g., zebrafish, fruit flies)—that mimics the disease state. The goal is to identify compounds that cause a desired change in the
phenotype, or observable characteristics, of the system, such as causing cancer cells to die, or reversing a developmental defect in a zebrafish model of a rare disease. Because it focuses on the functional outcome rather than a predefined target, phenotypic screening is exceptionally good at discovering drugs with novel mechanisms of action and is a particularly valuable tool for tackling rare and complex diseases where the underlying biology is not fully understood.
The convergence of these technologies—using AI to generate highly plausible hypotheses, then validating them with targeted phenotypic or high-throughput screens—creates a powerful, efficient, and rational engine for modern drug repurposing.
Navigating the Gauntlet: Commercial and Regulatory Strategy
Identifying a promising new use for an old drug is a monumental scientific achievement. However, it is only the first step on a long and perilous journey. The path from a validated laboratory finding to a commercially successful, regulatory-approved therapy is a gauntlet of complex intellectual property (IP) challenges, intricate global regulations, and formidable financial hurdles. For business leaders and investors, mastering this landscape is even more critical than the initial discovery. A brilliant scientific insight without a viable commercial and regulatory strategy is destined to remain a footnote in a scientific journal rather than a life-changing medicine.
Building a Defensible Moat: Advanced IP Strategies for Known Compounds
The central paradox and primary challenge of drug repurposing is that the core asset—the active pharmaceutical ingredient (API)—is already known and often in the public domain or covered by an expiring patent.14 Unlike a novel compound, where a strong composition-of-matter patent can create a 20-year fortress of market exclusivity, a repurposed drug starts from a position of IP vulnerability. Therefore, the strategy must pivot from protecting the
what (the compound) to protecting the how (the new application and its specific implementation). Building a robust and defensible IP “moat” around a repurposed drug requires a sophisticated, multi-layered approach.
Method-of-Use (MoU) Patents: This is the foundational IP tool for any repurposing project. An MoU patent, also known as a “new use” or “method-of-treatment” patent, does not protect the drug itself but rather the specific method of using that drug to treat a new disease.14 A typical claim would be structured as: “A method of treating Disease Y, comprising administering a therapeutically effective amount of Drug X.” While essential, MoU patents are notoriously difficult to enforce and are considered a relatively weak form of protection.69 The primary reason is the widespread practice of “off-label” prescribing. A generic manufacturer can legally sell a copy of Drug X for its original, off-patent indication. Physicians, in turn, are free to prescribe that cheap generic for the new, patented use (Disease Y). Suing thousands of individual doctors for patent infringement is commercially and ethically untenable, creating a significant commercial leak that can completely undermine the profitability of the repurposed product.69
Strengthening the Moat with Secondary Patents: Given the inherent weakness of a standalone MoU patent, a successful commercial strategy must build additional, stronger layers of IP protection. This is often achieved by creating new, patentable inventions related to the drug’s application, which can shift the protection back to a physical product that is harder for generics to copy.
- Formulation Patents: This is one of the most powerful strategies. Developing and patenting a new formulation of the drug—such as an extended-release tablet, a transdermal patch, a novel injectable, or a specific nanoparticle delivery system—that is tailored to the new indication can create a new, proprietary product.14 This is a much stronger form of protection because a generic competitor cannot simply use the old API; they would need to replicate the specific, patented formulation to be substitutable for the new use, which would constitute direct infringement.
- Combination Patents: Another highly effective approach is to patent a new fixed-dose combination of the repurposed drug with one or more other known drugs. If this new combination demonstrates unexpected synergy—where the combined therapeutic effect is greater than the sum of the individual drugs’ effects—it can be considered a non-obvious and highly valuable invention, potentially even qualifying for a new composition-of-matter patent.70
- Dosage and Regimen Patents: In some cases, the key innovation may lie in a specific dosing schedule or a narrow therapeutic window that is critical for efficacy and safety in the new indication. Patenting a specific dosage (e.g., “a 37.5 mg tablet”) or a regimen (e.g., “administering Drug X once weekly”) can provide an additional layer of protection, making it more difficult for a generic to be prescribed in a way that aligns with the approved label for the new use.
A truly robust IP strategy involves creating a “patent thicket”—a dense and overlapping network of these secondary patents that makes it difficult and costly for a competitor to design around.
The Regulatory Compass: Leveraging Global Incentives
Navigating the global regulatory landscape is a critical component of a successful repurposing strategy. Major regulatory bodies in the US, Europe, and Japan have established powerful incentives specifically to encourage the development of drugs for rare diseases, and these can be leveraged to create significant commercial advantages for repurposed orphan drugs.
United States (FDA): The U.S. has one of the most favorable environments for orphan drug development, built on several key pillars:
- The Orphan Drug Act (ODA) of 1983: This landmark legislation provides a suite of powerful incentives for drugs granted “orphan designation.” These include a seven-year period of market exclusivity upon approval (protecting against competition from the same drug for the same indication), tax credits for up to 25% of qualified clinical testing expenses, and a waiver of the substantial Prescription Drug User Fee (PDUFA), which can be nearly $3 million.17
- The 505(b)(2) Pathway: This streamlined regulatory pathway is particularly well-suited for repurposed drugs. It allows a sponsor to rely, in part, on existing data not developed by them (such as the original drug’s safety data or published literature), which can significantly reduce the number of new studies required for approval, saving time and money.14
- Priority Review Vouchers (PRV): To stimulate development for NTDs and rare pediatric diseases, the FDA awards a PRV to the sponsor of a newly approved drug in these categories. This voucher, which entitles the holder to an expedited six-month review for any future drug, is transferable and can be sold. These vouchers have become valuable financial assets, with sales prices historically averaging around $100 million, providing a crucial “pull” incentive for otherwise unprofitable research.41
Europe (EMA): The European Union offers a similarly robust set of incentives through its Orphan Medicinal Product Regulation:
- Market Exclusivity: A ten-year period of market exclusivity is granted to authorized orphan medicines, which can be extended to twelve years if the drug also complies with an agreed-upon pediatric investigation plan.21
- Scientific and Regulatory Support: Sponsors of designated orphan medicines have access to “protocol assistance,” which is a form of centralized scientific advice from the EMA to help guide the drug’s development program. They also benefit from a centralized authorization procedure, allowing for a single application to be valid across all EU member states.77
- Fee Reductions: Significant fee reductions are available for regulatory activities, including protocol assistance, marketing authorization applications, and inspections.21 The EMA is also actively exploring a PRV-like program to further incentivize development for neglected diseases.79
Japan (PMDA): Japan also provides strong support for orphan drug development, defined for diseases affecting fewer than 50,000 patients:
- Market Exclusivity and Priority Review: Orphan drugs receive an extended registration validity period of ten years and are granted priority review to accelerate the approval process.
- Financial Support: The government provides substantial financial incentives, including subsidies that can cover up to 50% of R&D costs and tax credits for R&D expenses.
The choice of regulatory pathway and the strategic sequencing of global filings can have a massive impact on the commercial return of a repurposed asset. A careful analysis of these frameworks is a prerequisite for any successful development plan.
| Incentive | United States (FDA) | European Union (EMA) | Japan (MHLW/PMDA) |
| Orphan Designation Criteria | Affects <200,000 people in the U.S. | Affects ≤5 in 10,000 people in the EU; or lacks profitability | Affects <50,000 people in Japan |
| Market Exclusivity | 7 years | 10 years (+2 years for pediatric use) | 10 years (extended registration validity) |
| R&D Tax Credits | 25% of qualified clinical testing costs | Varies by Member State | 6% tax reduction for R&D expenses |
| User Fee Waivers | Waiver of Prescription Drug User Fee (PDUFA) | Reduced fees for regulatory activities | N/A |
| R&D Grants / Subsidies | Orphan Product Grants Program | Funding via programs like Horizon Europe | Up to 50% reimbursement of development costs |
| Special Programs | Priority Review Voucher (PRV) for NTDs & Rare Pediatric Diseases | Protocol Assistance (scientific advice); considering a PRV program 77 | Priority review for orphan drugs |
The Valley of Death: Overcoming Financial and Market Access Barriers
Even with a clever IP strategy and a well-defined regulatory path, many promising repurposed drugs falter in the “valley of death”—the gap between clinical validation and successful commercialization. This is particularly true for off-patent, generic drugs, where the economic model is often broken.13
The core challenge is a lack of financial incentive. Why would a company invest hundreds of millions of dollars in the large-scale Phase III trials needed for regulatory approval of a generic drug’s new use, when competitors could immediately enter the market and share in the benefits? This “tragedy of the commons” means that research on repurposed generics is often left to academic institutions and non-profits that lack the resources for late-stage development and commercialization.5
The off-label use problem further complicates the financial picture. If a repurposed generic is approved for a new indication and given a higher price to reflect the new value and investment, payers and physicians may simply opt to use the much cheaper original generic off-label, completely eroding the market for the newly approved product.70 Payers are often resistant to paying a premium for an “old” drug, regardless of the new clinical data supporting its value in a different disease.85
Navigating this treacherous landscape requires rigorous competitive and market intelligence. This is where specialized platforms become indispensable. Services like DrugPatentWatch provide critical business intelligence that can inform strategy at every stage. By using such a platform, a company can:
- Map the Patent Landscape: Identify all existing patents related to a drug of interest, including composition-of-matter, formulation, and method-of-use patents, to assess freedom to operate and identify potential licensing opportunities.16
- Anticipate Generic Competition: Track patent expiration dates and monitor for Paragraph IV challenges to predict when generic versions of a drug will enter the market, which is crucial for forecasting the commercial viability of a repurposing project.
- Monitor Competitor Strategy: Analyze the clinical trial and patenting activities of competitors to uncover their research paths and anticipate their future repurposing strategies long before they become public knowledge.16
This type of deep intelligence allows a company to make informed decisions, avoid costly IP battles, and build a business case that is grounded in the realities of the market. Overcoming the financial valley of death for repurposed drugs requires more than just good science; it demands creative business models, strategic partnerships, and a clear-eyed understanding of the competitive and regulatory environment.
From Bench to Bedside: Landmark Case Studies in Repurposing
The principles and strategies of drug repurposing are best understood through the lens of real-world examples. These case studies are not just historical anecdotes; they are powerful illustrations of the diverse paths a repurposed drug can take, from serendipitous discovery to rational, mechanism-based design, and from corporate-led blockbusters to patient-driven triumphs. Each story offers critical lessons in scientific ingenuity, regulatory navigation, and commercial strategy.
The Cautionary and Redemptive Tale of Thalidomide
Few drugs carry as much historical weight as thalidomide. Initially marketed in the late 1950s as a seemingly safe, over-the-counter sedative, it was soon implicated in one of the worst medical disasters of the 20th century, causing severe birth defects in thousands of children worldwide. The drug was swiftly withdrawn from the market in disgrace.
However, years later, a compassionate-use observation by a physician in Jerusalem revealed that thalidomide had a dramatic effect in treating the painful skin lesions of erythema nodosum leprosum (ENL), a debilitating complication of leprosy. This sparked renewed scientific interest, and subsequent research uncovered the drug’s potent immunomodulatory and anti-angiogenic (inhibiting blood vessel formation) properties.9 This new understanding of its mechanism of action paved the way for its remarkable redemption. In 1998, the FDA approved thalidomide for the treatment of ENL, and in 2006, it was approved in combination with dexamethasone for newly diagnosed multiple myeloma, a blood cancer that relies on angiogenesis to grow.89 The story of thalidomide is a powerful lesson in both the potential dangers of drugs and the incredible power of repurposing to rescue a vilified compound by uncovering its true biological activity.
Serendipity Meets Science: Sildenafil for Pulmonary Arterial Hypertension (PAH)
The story of sildenafil is the quintessential example of serendipitous drug repurposing. Developed by Pfizer in the early 1990s as a potential treatment for angina, a type of chest pain caused by reduced blood flow to the heart, the drug showed disappointing results for its primary indication in early clinical trials. However, researchers noted a consistent and unexpected side effect: an increase in erections among male study participants. This observation led directly to its repositioning and subsequent launch as Viagra, one of the most commercially successful drugs in history.
But the story doesn’t end there. The same mechanism of action that proved effective for erectile dysfunction—the inhibition of an enzyme called phosphodiesterase type 5 (PDE5), which leads to the relaxation and widening of blood vessels—was also highly relevant to another, much rarer condition: pulmonary arterial hypertension (PAH).91 PAH is a life-threatening disease characterized by dangerously high blood pressure in the arteries of the lungs. By relaxing these arteries, sildenafil reduces the strain on the heart and improves patients’ ability to exercise. Following successful clinical trials, sildenafil (marketed as Revatio for this indication) was approved by the FDA in 2005 for the treatment of PAH, providing a critical new therapy for patients with this devastating rare disease. Sildenafil’s journey illustrates how an initial serendipitous finding can be followed by rational, mechanism-based development to address a significant unmet need.
Patient-Driven Repurposing in Rare Diseases
In the world of rare diseases, where commercial incentives are often weak, patients and their families have emerged as powerful catalysts for R&D. Patient advocacy groups are increasingly funding research, building patient registries, and driving the repurposing of existing drugs.
Sirolimus (Rapamycin) for ALPS: Autoimmune Lymphoproliferative Syndrome (ALPS) is a rare genetic disorder of the immune system that leads to chronic lymph node swelling and autoimmune attacks on blood cells.94 Treatment often involved high-dose steroids with significant side effects. Researchers hypothesized that sirolimus (also known as rapamycin), an off-patent immunosuppressant commonly used to prevent organ transplant rejection, might be effective due to its ability to induce apoptosis (programmed cell death) in the abnormal immune cells that drive ALPS.94 This hypothesis was first tested in mouse models. Following promising preclinical results, the US charity Cures Within Reach funded a small pilot study in six patients with refractory ALPS. The results were dramatic. After 90 days, five of the six patients were in complete remission, and all were able to taper off steroids.94 This landmark study, driven by non-profit funding, established sirolimus as a highly effective second-line therapy for ALPS, saving an estimated $50,000 per patient per year in treatment costs.
Everolimus for Tuberous Sclerosis Complex (TSC): TSC is a genetic disorder that causes benign tumors to grow in the brain, kidneys, heart, skin, and other organs. Research revealed that the disease is caused by mutations in the TSC1 or TSC2 genes, which leads to hyperactivation of a key cellular growth pathway regulated by the protein mTOR. This provided a clear, rational target for therapy. Scientists hypothesized that an mTOR inhibitor could be effective. Everolimus, a drug already approved for use in cancer and organ transplantation, was tested in clinical trials for TSC. The results were transformative. The EXIST-1 and EXIST-2 trials showed that everolimus significantly reduced the size of brain tumors (subependymal giant cell astrocytomas, or SEGAs) and kidney tumors (angiomyolipomas) in TSC patients.99 The FDA subsequently approved everolimus for these TSC-related conditions, and later for TSC-associated seizures, making it the first therapy to target the underlying molecular basis of the disease. This case is a textbook example of a successful, mechanism-based repurposing strategy driven by a deep understanding of disease genetics.
Nitisinone for Alkaptonuria (AKU): The journey of nitisinone is a testament to the power of patient advocacy. The compound was originally developed as a herbicide. It was later repurposed to treat a rare metabolic disorder called tyrosinemia type 1. Patients with another rare disease, alkaptonuria (AKU), which causes a painful, debilitating buildup of a chemical called homogentisic acid (HGA), saw the potential of nitisinone, as it worked on the same biochemical pathway. After an initial trial in the U.S. failed, the UK-based Alkaptonuria Society refused to give up. The patient group raised funds to conduct crucial research, including developing a new metric to measure disease severity and creating a new mouse model. Their efforts led to the formation of an international consortium that secured €6 million in funding for new clinical trials. The results were overwhelmingly positive, showing that nitisinone dramatically reduced HGA levels. In 2025, nitisinone became the first and only FDA-approved treatment for AKU, a victory made possible by the relentless drive of the patient community.97
Humanitarian Triumphs in Neglected Diseases
For neglected tropical diseases, where the market has completely failed, drug repurposing has been the engine behind some of the greatest public health successes of our time. These stories are defined by collaboration, philanthropy, and a focus on humanitarian impact over profit.
Ivermectin for Onchocerciasis (River Blindness): Ivermectin was originally developed by Merck in the 1970s as a highly effective veterinary drug to treat parasites in livestock. Researchers soon realized its potential to treat onchocerciasis, or river blindness, a parasitic disease transmitted by blackflies that caused widespread blindness and debilitating skin disease across Africa and Latin America. In a landmark decision in 1987, Merck committed to donating ivermectin (under the brand name Mectizan) for as long as needed to eliminate the disease as a public health problem. This program, one of the most successful and long-running public-private partnerships in history, has enabled the treatment of hundreds of millions of people, preventing an estimated 600,000 cases of blindness and reclaiming millions of hectares of arable land.106
Eflornithine for African Trypanosomiasis (Sleeping Sickness): Eflornithine was developed in the 1970s as a potential anti-cancer drug, but was ultimately shelved for lack of efficacy.109 However, researchers discovered it was highly effective against the parasite that causes the late stage of West African trypanosomiasis, or sleeping sickness, a fatal disease.111 Despite its effectiveness, the drug was not profitable, and its manufacturer decided to cease production in the late 1990s. This prompted an international outcry, led by Médecins Sans Frontières (MSF) and the WHO, who mounted a public campaign that ultimately convinced the company to resume production and donate the drug.112 Eflornithine, the “resurrection drug,” became a cornerstone of sleeping sickness treatment for decades, saving countless lives and demonstrating the critical role of advocacy in ensuring access to repurposed medicines for neglected populations.
Miltefosine for Leishmaniasis: Originally investigated as a topical anti-cancer agent in the 1980s, miltefosine was found to have potent activity against the Leishmania parasite.114 Leishmaniasis is a devastating parasitic disease that manifests in visceral, cutaneous, and mucosal forms, and existing treatments were toxic, painful, and required lengthy intravenous infusions. Following successful clinical trials, miltefosine was repurposed and became the first-ever effective and safe oral treatment for leishmaniasis, revolutionizing the management of the disease, particularly in remote, resource-poor settings.114
The Horizon: Future Trends and Strategic Imperatives
The field of drug repurposing is not static; it is a dynamic and rapidly evolving discipline. As we look to the horizon, a convergence of powerful technologies, new collaborative models, and evolving policy frameworks promises to further accelerate the pace of discovery and unlock even greater value from the world’s existing medicines. For pharmaceutical companies, biotech innovators, and investors, understanding these future trends is not just an academic exercise—it is essential for building a sustainable strategy and securing a leadership position in the next era of therapeutic innovation.
The Next Wave of Innovation: Converging Technologies
The future of repurposing will be defined by the integration of multiple cutting-edge technologies, creating a discovery engine that is more predictive, precise, and efficient than ever before.
Precision Medicine and Patient Stratification: The era of “one-size-fits-all” medicine is ending. The rise of precision medicine, which tailors treatment to the individual characteristics of each patient, is creating unprecedented opportunities for drug repurposing.118 Advances in genomics and other ‘omics’ technologies are allowing us to deconstruct common diseases like cancer or Alzheimer’s into dozens of molecularly distinct, rare subtypes. This creates numerous “orphan-like” patient populations defined by a specific genetic mutation or biomarker. A drug that failed in a broad clinical trial for “lung cancer” might be highly effective in the small subset of patients whose tumors are driven by a specific genetic fusion that the drug happens to target. The synergy is clear: precision medicine identifies the highly specific targets, and AI-driven repurposing can screen the entire pharmacopeia to find an existing drug that hits that target. This blurs the lines between common and rare disease R&D and dramatically increases the value of a company’s library of shelved assets.16
The Continued Ascendancy of AI and Big Data: The role of artificial intelligence will only grow in importance. As biomedical datasets—from genomic sequences to electronic health records to scientific literature—continue to expand at an exponential rate, AI will be the essential tool for making sense of this complexity.57 Future AI platforms will become even more sophisticated, integrating more data modalities and employing more advanced algorithms to generate repurposing hypotheses with higher accuracy and novelty.56 The competitive advantage will shift to those who can build and curate the most comprehensive, high-quality datasets and develop the most powerful predictive algorithms to mine them.
Organ-on-a-Chip and Advanced Preclinical Models: A major bottleneck in drug development is the reliance on traditional cell cultures and animal models, which often fail to accurately predict human responses. Organ-on-a-chip technology is set to revolutionize this stage of research. These are microfluidic devices, often the size of a USB stick, that contain living human cells cultured in a way that mimics the structure and function of human organs like the lung, liver, or brain.124 These “microphysiological systems” allow for faster, more accurate, and more human-relevant testing of drug efficacy and toxicity. For repurposing, this means that a computationally-predicted candidate can be rapidly tested on a “lung-on-a-chip” or a “brain-on-a-chip” derived from patient cells, providing much stronger preclinical evidence before moving into expensive human trials.
The future lies in the seamless integration of these technologies. Imagine a workflow where AI analyzes a rare disease patient’s genomic data to identify a unique therapeutic target, computationally screens thousands of existing drugs to predict a match, and then validates that prediction on an organ-on-a-chip model built using the patient’s own stem cells. This is the future of personalized drug repurposing.
Forging Alliances: The New Ecosystem of Collaboration
The traditional model of a single, vertically integrated pharmaceutical company conducting all R&D in-house is ill-suited to the challenges and opportunities of drug repurposing, especially in areas with limited commercial potential. The future belongs to a more open, networked ecosystem of collaboration that pools resources, shares risk, and leverages the unique strengths of different stakeholders.
Public-Private Partnerships (PPPs): For neglected diseases and many ultra-rare conditions, PPPs are not just helpful; they are essential. Organizations like the DNDi and initiatives like Europe’s Innovative Medicines Initiative (IMI) have proven that a collaborative model—bringing together the compound libraries and development expertise of pharmaceutical companies, the basic science insights of academia, and the funding and focus of governments and philanthropies—can successfully develop drugs for diseases with no commercial market.129 These partnerships de-risk R&D for all parties and ensure that the primary goal remains patient impact.
The Central Role of Patient Advocacy Groups (PAGs): As the case studies of sirolimus and nitisinone demonstrate, patient advocacy groups have evolved from being passive recipients of medical care to active and powerful drivers of research. In the future, PAGs will be even more central to the repurposing ecosystem. They are uniquely positioned to:
- Fund early-stage research: Provide the seed funding needed to test initial repurposing hypotheses.
- Build patient registries: Create the invaluable databases of patient data and natural history information that are essential for designing efficient clinical trials in rare diseases.
- Drive trial recruitment: Mobilize their communities to ensure that rare disease trials can be successfully enrolled.
- Advocate with regulators and payers: Provide the crucial patient perspective to regulatory agencies and reimbursement bodies to ensure that successfully repurposed drugs reach the community.
For any company developing a repurposed drug for a rare disease, a deep and authentic partnership with the relevant PAG is a critical success factor.
Policy as a Catalyst: Evolving Frameworks to Spur Innovation
For drug repurposing to reach its full potential, particularly for off-patent generic drugs, the scientific and technological advances must be matched by policy innovation. The current system is stuck in a paradox: there is immense, untapped therapeutic value in thousands of cheap, generic drugs, but there is no sustainable business model to fund the clinical trials needed to formally approve these new uses.83 The future will require policymakers to create new frameworks that can solve this market failure.
New “Pull” Incentives for Generics: The most promising ideas focus on creating new “pull” incentives that reward successful repurposing outcomes for off-patent drugs. These could include 83:
- Transferable Exclusivity Vouchers: Similar to the PRV, a voucher could be awarded to any entity (including a non-profit or academic group) that successfully gains regulatory approval for a new use of a generic drug. This would create a monetizable asset that could fund the required research.
- Prize Funds: Governments or philanthropic funds could offer substantial prizes for achieving specific public health goals through generic repurposing, such as finding a new effective treatment for a specific rare cancer.
Streamlined Regulatory and Reimbursement Pathways: International initiatives like REPO4EU in Europe are working to create a more harmonized and efficient ecosystem for developing and accessing repurposed medicines.132 This includes advocating for streamlined regulatory requirements for label extensions of generic drugs and developing new reimbursement models.
Fair Pricing Models: A critical and contentious issue is pricing. There is a need for policy frameworks that allow for fair, value-based pricing for a repurposed generic’s new indication—a price that is high enough to incentivize investment but avoids price-gouging and is delinked from the drug’s original low cost.134 This would likely require legal changes to prevent automatic generic substitution at the pharmacy for the new, on-label use.
The path forward is clear. The convergence of technology and collaboration is creating a golden age for drug repurposing. However, to fully translate this scientific potential into patient benefit, we must also have the courage to innovate our business models, our regulatory frameworks, and our public policies to create a sustainable system that rewards the vital work of teaching old drugs new, life-saving tricks.
Conclusion
The landscape of pharmaceutical innovation is at a critical inflection point. The traditional model of de novo drug discovery, while historically successful, is now facing a crisis of sustainability, characterized by soaring costs, protracted timelines, and punishingly high failure rates. In this challenging environment, drug repurposing has emerged not as a mere cost-saving tactic, but as a core strategic imperative. It represents a paradigm shift, transforming the R&D process from a high-risk gamble into a more predictive, efficient, and rational science. By leveraging the vast, de-risked library of existing medicines, this approach offers an unassailable value proposition: the ability to deliver novel therapies to patients faster, cheaper, and with a significantly higher probability of success.
This strategy holds particular promise for the populations most failed by the traditional model: patients with rare diseases and those suffering from neglected tropical diseases. For the 350 million people worldwide with a rare disease, most of whom have no approved treatment, repurposing offers the most pragmatic and accelerated path to hope. For the more than 1 billion people afflicted by neglected diseases, for whom a commercial market will never exist, repurposing is often the only economically feasible pathway to a cure.
The engine of this revolution is technology. The convergence of computational biology, artificial intelligence, and advanced experimental screening methods has transformed repurposing from an art of serendipity into a data-driven discipline. AI and machine learning algorithms can now sift through mountains of biological and clinical data to predict novel drug-disease connections with astonishing accuracy, while experimental platforms like organ-on-a-chip technology promise to make preclinical validation more human-relevant and efficient than ever before.
However, scientific potential alone is not enough. The ultimate success of drug repurposing hinges on navigating a complex gauntlet of commercial, intellectual property, and regulatory challenges. A sophisticated, multi-layered IP strategy that moves beyond weak method-of-use patents to protect novel formulations and combinations is essential for building a defensible commercial asset. A deep understanding of the global regulatory incentives offered by bodies like the FDA, EMA, and PMDA is critical for maximizing market exclusivity and return on investment. Most urgently, new policy frameworks and collaborative models are needed to solve the market failure that prevents the repurposing of valuable off-patent generic drugs.
The future of medicine will be shaped by those who can master this new paradigm. It will require a shift in mindset—viewing “failed” drugs as valuable assets, embracing open collaboration between industry, academia, and patient groups, and building business models centered on powerful predictive platforms. By harnessing the full potential of the medicines we already have, the repurposing revolution offers a clear and compelling path toward a more innovative, efficient, and equitable future for all patients.
Key Takeaways
- Repurposing as a Strategic Answer to the R&D Crisis: Drug repurposing is a direct and powerful response to the unsustainable costs ($2-3 billion per new drug), long timelines (10-17 years), and high failure rates (>90%) of traditional drug discovery.
- Compelling Economic Advantages: The core value proposition of repurposing lies in its ability to reduce development costs by over 50%, shorten timelines by 5-7 years, and increase the probability of success threefold by leveraging existing safety and manufacturing data.
- Dual Focus on Rare and Neglected Diseases: Repurposing is uniquely positioned to address unmet needs in two distinct areas: it can act as a market disruptor in the high-price, low-volume world of rare diseases, and as a market creator in the no-price, high-volume humanitarian landscape of neglected diseases.
- Technology is the Driving Force: Modern repurposing is a data-driven science powered by computational biology, artificial intelligence, and machine learning. These technologies enable the rapid, systematic prediction of new drug-disease connections from vast and complex datasets.
- IP Strategy is Paramount: Commercial success depends on a sophisticated intellectual property strategy. Since the drug compound itself is often unpatentable, protection must be built through layers of secondary patents, such as those for new formulations, combinations, and specific dosage regimens.
- Navigating Global Regulatory Incentives is Key: Leveraging incentives like the U.S. Orphan Drug Act (7-year exclusivity), the EMA’s Orphan Regulation (10-year exclusivity), and Priority Review Vouchers is critical for maximizing the commercial viability of a repurposed asset.
- The Generic Drug Paradox: A major unresolved challenge is the lack of financial incentives to repurpose off-patent generic drugs. Issues like weak patent enforceability and off-label use create a “tragedy of the commons” that new policy frameworks and public-private partnerships must address.
- The Future is Integrated and Collaborative: The next wave of innovation will come from integrating precision medicine, AI, and advanced preclinical models like organ-on-a-chip. Success will increasingly depend on a collaborative ecosystem involving pharmaceutical companies, academic researchers, and empowered patient advocacy groups.
Frequently Asked Questions (FAQ)
1. If a repurposed drug uses an old molecule, how can it be considered innovative?
Innovation in drug repurposing lies not in the molecule itself, but in the new biological understanding and clinical application. The novelty comes from discovering a previously unknown mechanism of action or identifying a new link between a drug’s molecular targets and the pathophysiology of a different disease. For example, the innovation of using everolimus for Tuberous Sclerosis Complex was not in the drug, but in the groundbreaking realization that its mTOR-inhibiting mechanism directly addressed the genetic root cause of the disease. Furthermore, innovation can be embodied in new, patentable formulations or delivery systems designed specifically to optimize the drug for its new indication, which can improve efficacy, safety, or patient compliance.
2. How does the rise of precision medicine affect the commercial viability of drug repurposing?
Precision medicine significantly enhances the commercial viability of drug repurposing by creating new, well-defined markets. It allows for the stratification of common diseases into multiple, smaller “orphan-like” subsets based on specific biomarkers or genetic mutations. A drug that failed in a broad trial for a common disease may be highly effective in one of these smaller, targeted populations. This creates an opportunity to gain orphan drug designation and its associated incentives (like 7-10 years of market exclusivity) for an indication within a larger disease area. This strategy, sometimes called “salami-slicing,” allows companies to rescue shelved assets and target them to patient populations where they have a high probability of success, turning a failed blockbuster attempt into a successful niche product.
3. What is the single biggest barrier to repurposing off-patent generic drugs, and what is the most promising solution?
The single biggest barrier is the lack of a sustainable business model due to insufficient intellectual property protection and the threat of off-label use. A company is hesitant to spend millions on clinical trials to prove a new use for a generic drug when doctors can simply prescribe the cheaper, existing generic for that new use, allowing competitors to free-ride on the investment. The most promising solution involves policy innovation to create new “pull” incentives. A transferable exclusivity voucher, awarded to any entity that gains regulatory approval for a new use of a generic, is a leading proposal. This would create a valuable, sellable asset (~$100 million) that could finance the necessary clinical development, effectively creating a market-based solution to a market failure.
4. How can smaller biotech companies or academic institutions realistically compete in drug repurposing against large pharmaceutical companies with vast compound libraries?
Smaller entities can compete effectively by focusing on agility, specialized expertise, and collaboration. Their competitive advantage lies not in owning vast libraries, but in developing superior discovery platforms. A small biotech with a cutting-edge AI platform that can analyze public datasets more effectively than a large company’s internal system can generate higher-quality hypotheses. They can also focus on deep biological expertise in a specific rare disease, building strong relationships with patient advocacy groups to facilitate research and clinical trials. Their strategy is often not to commercialize the drug themselves, but to act as a discovery engine—identifying and de-risking a repurposed candidate through early clinical studies before partnering with or licensing the asset to a larger pharmaceutical company for late-stage development and marketing.
5. Beyond cost and speed, what is the most significant strategic value of a dedicated drug repurposing program for a large pharmaceutical company?
The most significant strategic value is portfolio risk management. A large pharmaceutical company’s innovative pipeline is inherently high-risk, with over 90% of projects failing. These failures can be catastrophic, wiping out billions in investment and market capitalization. A dedicated drug repurposing program functions as a strategic hedge against this risk. It provides a parallel stream of lower-risk, higher-probability, mid-to-late-stage assets. By investing a portion of the R&D budget into repurposing, a company can ensure a more consistent flow of new products to the market, smoothing out the volatile “boom and bust” cycle of traditional discovery and providing a more stable foundation for long-term growth. It transforms the R&D portfolio from a series of independent lottery tickets into a balanced investment strategy.
References
- How drug repurposing can advance drug discovery: challenges and opportunities – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2024.1460100/full
- The value of drug repositioning in the current pharmaceutical market – PubMed, accessed August 1, 2025, https://pubmed.ncbi.nlm.nih.gov/19330170/
- Ethical, economic and clinical aspects of financing … – Article – JHPOR, accessed August 1, 2025, https://www.jhpor.com/article/2238-ethical-economic-and-clinical-aspects-of-financing-treatment-of-rare-diseases
- Reviving Dormant Assets: A Strategic Blueprint for Drug …, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/reviving-a-discontinued-drug/
- Repurposing generic drugs can reduce time and cost to develop new treatments, accessed August 1, 2025, https://www.michiganmedicine.org/health-lab/repurposing-generic-drugs-can-reduce-time-and-cost-develop-new-treatments
- Drug Repurposing Strategies, Challenges and Successes | Technology Networks, accessed August 1, 2025, https://www.technologynetworks.com/drug-discovery/articles/drug-repurposing-strategies-challenges-and-successes-384263
- Drug Repositioning: A Review, accessed August 1, 2025, https://www.rroij.com/open-access/drug-repositioning-a-review.pdf
- Drug repurposing: progress, challenges and … – PharmaKure, accessed August 1, 2025, https://pharmakure.com/wp-content/uploads/2022/07/Drug-Repurposing-Review.pdf
- Drug repurposing: Clinical practices and regulatory pathways – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12048090/
- Accelerating Drug Development: Unleashing the Power of Drug Repurposing, accessed August 1, 2025, https://drugrepocentral.scienceopen.com/hosted-document?doi=10.58647/DRUGREPO.24.1.0013
- Drug Repurposing Strategy (DRS): Emerging Approach to Identify Potential Therapeutics for Treatment of Novel Coronavirus Infection – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.628144/full
- ecrin.org, accessed August 1, 2025, https://ecrin.org/sites/default/files/Ecrin/pdf/Chapter13_final.pdf
- Drug repurposing: a systematic review on root causes, barriers and …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9336118/
- Turning Old Gold into New Revenue: Intellectual Property and Regulatory Considerations for Drug Repurposing – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/intellectual-property-rights-and-regulatory-considerations-for-drug-repurposing/
- Advantages of Drug Repurposing – pharm-int – Pharmaceutics International, accessed August 1, 2025, https://www.pharm-int.com/resources/advantages-of-drug-repurposing/
- The Repositioning Revolution: Transforming Patent Data into Pharmaceutical Competitive Advantage – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/review-of-drug-repositioning-approaches-and-resources/
- The Orphan Drug Act: Legal Overview and Policy Considerations …, accessed August 1, 2025, https://www.congress.gov/crs-product/IF12605
- Rare Diseases Team | FDA, accessed August 1, 2025, https://www.fda.gov/about-fda/accelerating-rare-disease-cures-arc-program/rare-diseases-team
- Rare Diseases at FDA, accessed August 1, 2025, https://www.fda.gov/patients/rare-diseases-fda
- Treating rare diseases: the challenge of orphan drugs – POST Parliament, accessed August 1, 2025, https://post.parliament.uk/treating-rare-diseases-the-challenge-of-orphan-drugs/
- Orphan designation: Overview | European Medicines Agency (EMA), accessed August 1, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/orphan-designation-overview
- GAO-25-106774, RARE DISEASE DRUGS: FDA Has Steps Underway to Strengthen Coordination of Activities Supporting Drug Development, accessed August 1, 2025, https://files.gao.gov/reports/GAO-25-106774/index.html?_gl=1*fwaz7a*_ga*MjI1NDUyNzMwLjE3MzMyNDM0NTQ.*_ga_V393SNS3SR*MTczMzI0MzQ1NC4xLjEuMTczMzI0MzQ5NS4wLjAuMA..
- Rare Disease: How Common is the Uncommon? – Indiana University School of Medicine, accessed August 1, 2025, https://medicine.iu.edu/blogs/rare-disease-research/rare-disease-common-uncommon
- List of Rare Diseases | A-Z Database | NORD, accessed August 1, 2025, https://rarediseases.org/rare-diseases/
- Policymaking for Orphan Drugs and Its Challenges – AMA Journal of Ethics, accessed August 1, 2025, https://journalofethics.ama-assn.org/article/policymaking-orphan-drugs-and-its-challenges/2015-08
- Drug Repurposing: Potential to Expand Rare Disease Treatment …, accessed August 1, 2025, https://advisory.avalerehealth.com/insights/drug-repurposing-potential-to-expand-rare-disease-treatment
- Neglected tropical diseases — GLOBAL, accessed August 1, 2025, https://www.who.int/health-topics/neglected-tropical-diseases
- Neglected tropical diseases – World Health Organization (WHO), accessed August 1, 2025, https://www.who.int/news-room/questions-and-answers/item/neglected-tropical-diseases
- Neglected Tropical Diseases (Human) – UNDRR, accessed August 1, 2025, https://www.undrr.org/understanding-disaster-risk/terminology/hips/bi0021
- The new reality of R&D funding for neglected tropical diseases | Devex, accessed August 1, 2025, https://www.devex.com/news/the-new-reality-of-r-d-funding-for-neglected-tropical-diseases-109128
- Neglected Tropical Diseases | NIAID, accessed August 1, 2025, https://www.niaid.nih.gov/research/neglected-tropical-diseases
- SUPPORTING RESEARCH IN NEGLECTED TROPICAL DISEASES – Harvard Kennedy School, accessed August 1, 2025, https://www.hks.harvard.edu/sites/default/files/centers/mrcbg/programs/cri/files/NTD(final).pdf
- Three rare disease drug development challenges and opportunities – Alcimed, accessed August 1, 2025, https://www.alcimed.com/en/insights/rare-disease-drug-development/
- Four Challenges to rare disease drug development | Insights – ICON plc, accessed August 1, 2025, https://www.iconplc.com/insights/blog/2019/10/24/4-challenges-to-successful-rare-disease-drug-development
- Challenges and Innovations in Conducting Clinical Trials in Rare …, accessed August 1, 2025, https://www.ijsrtjournal.com/article/Challenges+and+Innovations+in+Conducting+Clinical+Trials+in+Rare+and+Orphan+Diseases
- Economic Modeling Considerations for Rare Diseases – RTI Health Solutions, accessed August 1, 2025, https://www.rtihs.org/sites/default/files/29341%20Rothawell%202018%20Economic%20modeling%20considerations%20for%20rare%20diseases.pdf
- Rare Diseases: Meeting the Unique Challenges of Orphan Drug Development, accessed August 1, 2025, https://www.appliedclinicaltrialsonline.com/view/rare-diseases-meeting-unique-challenges-orphan-drug-development
- Orphan Drugs Have Lower Drug Development Costs Compared With Nonorphan Drugs, accessed August 1, 2025, https://www.ajmc.com/view/orphan-drugs-have-lower-drug-development-costs-compared-with-nonorphan-drugs
- Who we are | DNDi, accessed August 1, 2025, https://dndi.org/about/who-we-are/
- Innovation in neglected tropical disease drug discovery and development – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6022351/
- Priority review – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Priority_review
- Priorities for the Priority Review Voucher – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5239680/
- Priority Review Vouchers – Sites @ Fuqua, accessed August 1, 2025, https://sites.fuqua.duke.edu/priorityreviewvoucher/
- (PDF) Computational Approaches in Drug Repurposing, accessed August 1, 2025, https://www.researchgate.net/publication/371383178_Computational_Approaches_in_Drug_Repurposing
- Computational Drug Repurposing: Approaches and Case Studies – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/computational-drug-repurposing-approaches-and-case-studies/
- A review of computational drug repurposing – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6989243/
- Computational Drug Repositioning: Current Progress and Challenges, accessed August 1, 2025, https://www.mdpi.com/2076-3417/10/15/5076
- novel computational approach for drug repurposing using systems …, accessed August 1, 2025, https://academic.oup.com/bioinformatics/article/34/16/2817/4925258
- Network-based drug repositioning | Request PDF – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/236048311_Network-based_drug_repositioning
- network-based drug repurposing method via non-negative matrix factorization | Bioinformatics | Oxford Academic, accessed August 1, 2025, https://academic.oup.com/bioinformatics/article/38/5/1369/6454947
- A genome-wide positioning systems network algorithm for in silico drug repurposing – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6677722/
- A Comparison of Network-Based Methods for Drug Repurposing along with an Application to Human Complex Diseases – MDPI, accessed August 1, 2025, https://www.mdpi.com/1422-0067/23/7/3703
- Machine Learning and Artificial Intelligence in drug repurposing – challenges and perspectives, accessed August 1, 2025, https://drugrepocentral.scienceopen.com/hosted-document?doi=10.58647/DRUGARXIV.PR000007.v1
- (PDF) Machine Learning and Artificial Intelligence in drug repurposing – challenges and perspectives – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/378950581_Machine_Learning_and_Artificial_Intelligence_in_drug_repurposing_-_challenges_and_perspectives
- AI-powered drug discovery for neglected diseases: accelerating public health solutions in the developing world – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11719738/
- Artificial intelligence in drug repurposing for rare diseases: a mini-review – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1404338/full
- AI in Drug Repurposing: Finding New Uses for Existing Medications – Astrix, accessed August 1, 2025, https://astrixinc.com/blog/ai-in-drug-repurposing-finding-new-uses-for-existing-medications/
- Machine-learning Repurposing of DrugBank Compounds for Opioid …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10202846/
- DrugCLIP: Contrastive Drug-Disease Interaction For Drug Repurposing – arXiv, accessed August 1, 2025, https://arxiv.org/html/2407.02265v1
- (PDF) AI-powered drug discovery for neglected diseases: accelerating public health solutions in the developing world – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/387920368_AI-powered_drug_discovery_for_neglected_diseases_accelerating_public_health_solutions_in_the_developing_world
- www.scdiscoveries.com, accessed August 1, 2025, https://www.scdiscoveries.com/blog/high-throughput-screening-accelerate-drug-discovery/#:~:text=Drug%20repurposing%3A%20Researchers%20can%20also,and%20accelerate%20drug%20development%20timelines.
- High-throughput screening (HTS) | BMG LABTECH, accessed August 1, 2025, https://www.bmglabtech.com/en/blog/high-throughput-screening/
- HIGH-THROUGHPUT SCREENING – MSU Drug Discovery, accessed August 1, 2025, https://drugdiscovery.msu.edu/facilities/high-throughput-screening.aspx
- Phenotypic screening – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Phenotypic_screening
- Phenotypic Screening: A Powerful Tool for Drug Discovery – Technology Networks, accessed August 1, 2025, https://www.technologynetworks.com/drug-discovery/articles/phenotypic-screening-a-powerful-tool-for-drug-discovery-398572
- Phenotype-Based Drug Screening – Creative Bioarray, accessed August 1, 2025, https://dda.creative-bioarray.com/phenotype-based-drug-screening.html
- Biopharmaceuticals: The Patent Implications of Drug Repurposing – PatentPC, accessed August 1, 2025, https://patentpc.com/blog/patent-implications-of-drug-repurposing
- Patenting New Uses for Old Inventions – Scholarship@Vanderbilt Law, accessed August 1, 2025, https://scholarship.law.vanderbilt.edu/cgi/viewcontent.cgi?article=2919&context=vlr
- Why Method of Treatment Patents for Repurposed Drugs Are Worth the Investment, accessed August 1, 2025, https://www.jdsupra.com/legalnews/why-method-of-treatment-patents-for-92813/
- Repurposing – Finding New Uses for Old (and Patented) Drugs …, accessed August 1, 2025, https://scholarship.law.marquette.edu/cgi/viewcontent.cgi?article=1243&context=iplr
- On-Label or Off-Label? Overcoming Regulatory and Financial …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7006723/
- Patent protection strategies – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3146086/
- Patenting Repurposed Drugs, accessed August 1, 2025, https://www.patentdocs.org/2018/09/patenting-repurposed-drugs.html
- Optimizing Your Drug Patent Strategy: A Comprehensive Guide for Pharmaceutical Companies – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/optimizing-your-drug-patent-strategy-a-comprehensive-guide-for-pharmaceutical-companies/
- Orphan Drug Credit: What It Is, How It Works – Investopedia, accessed August 1, 2025, https://www.investopedia.com/terms/o/orphan-drug-credit.asp
- Drug Repurposing: Legal and Regulatory Issues in the US, accessed August 1, 2025, https://drugrepocentral.scienceopen.com/hosted-document?doi=10.14293/S2199-rexpo22011v1
- Orphan incentives | European Medicines Agency (EMA), accessed August 1, 2025, https://www.ema.europa.eu/en/human-regulatory-overview/research-development/orphan-designation-research-development/orphan-incentives
- Orphan incentives | European Medicines Agency (EMA), accessed August 1, 2025, https://www.ema.europa.eu/en/orphan-incentives
- MAKING A CASE FOR A PRIORITY REVIEW VOUCHER PROGRAMME IN THE EU – Deutsche Stiftung Weltbevölkerung, accessed August 1, 2025, https://www.dsw.org/wp-content/uploads/2024/01/DSW_Introducing_PRV_EU_digital.pdf
- European priority review vouchers for neglected disease product development – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10828857/
- Quality charter – Orphanet, accessed August 1, 2025, https://www.orpha.net/en/other-information/about-orphan-drugs?stapage=japan
- Why promising drugs are shelved and barriers and facilitators to re-purposing them: A systematic literature review | medRxiv, accessed August 1, 2025, https://www.medrxiv.org/content/10.1101/2021.09.28.21264254v1.full-text
- Incentivizing Generic Drug Repurposing in the United States – Market Shaping Accelerator, accessed August 1, 2025, https://marketshaping.uchicago.edu/wp-content/uploads/2025/04/Generic-drug-repurposing-AMC.pdf
- Repurposing generic drugs can reduce time and cost to develop new treatments, accessed August 1, 2025, https://deepblue.lib.umich.edu/bitstream/handle/2027.42/175351/Repurposing%20generic%20drugs%20can%20reduce%20time%20and%20cost%20to%20develop%20new%20treatments%20%E2%80%93%20but%20low%20profitability%20remains%20a%20barrier.pdf?sequence=2
- How does prevalence affect pricing of rare disease drugs? | Insights & Events, accessed August 1, 2025, https://www.crai.com/insights-events/publications/how-does-prevalence-affect-pricing-rare-disease-drugs/
- Drug Repurposing of Generic Drugs: Challenges and the Potential …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10627937/
- DrugPatentWatch | Software Reviews & Alternatives – Crozdesk, accessed August 1, 2025, https://crozdesk.com/software/drugpatentwatch
- Thalidomide – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Thalidomide
- Thalidomide: Uses, Interactions, Mechanism of Action | DrugBank …, accessed August 1, 2025, https://go.drugbank.com/drugs/DB01041
- Thalidomide (oral route) – Side effects & dosage – Mayo Clinic, accessed August 1, 2025, https://www.mayoclinic.org/drugs-supplements/thalidomide-oral-route/description/drg-20066301
- Sildenafil – Pulmonary Hypertension Association, accessed August 1, 2025, https://phassociation.org/patients/treatments/sildenafil/
- Repurposing of the PDE5 Inhibitor Sildenafil for the Treatment of Persistent Pulmonary Hypertension in Neonates – PubMed, accessed August 1, 2025, https://pubmed.ncbi.nlm.nih.gov/32964819/
- The Prospect and Challenges of Repurposing Established Drugs in …, accessed August 1, 2025, https://www.mdpi.com/2673-6411/4/3/12
- Treatment with sirolimus results in complete responses in patients …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2819393/
- Efficacy of sirolimus for treatment of autoimmune lymphoproliferative syndrome: a systematic review of open label clinical studies | Request PDF – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/353985031_Efficacy_of_sirolimus_for_treatment_of_autoimmune_lymphoproliferative_syndrome_a_systematic_review_of_open_label_clinical_studies
- Treatment with sirolimus results in complete responses in patients with Autoimmune Lymphoproliferative Syndrome | Request PDF – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/23998606_Treatment_with_sirolimus_results_in_complete_responses_in_patients_with_Autoimmune_Lymphoproliferative_Syndrome
- Drug repurposing in rare diseases | Beacon for rare diseases, accessed August 1, 2025, https://www.rarebeacon.org/research/drug-repurposing/
- Profile of everolimus in the treatment of tuberous sclerosis complex – Dove Medical Press, accessed August 1, 2025, https://www.dovepress.com/profile-of-everolimus-in-the-treatment-of-tuberous-sclerosis-complex-a-peer-reviewed-fulltext-article-NDT
- The Therapeutic Potential of Oral Everolimus for Facial Angiofibromas in Pediatric Tuberous Sclerosis Complex: A Case-Based Analysis of Efficacy – MDPI, accessed August 1, 2025, https://www.mdpi.com/2079-9721/12/12/334
- Long-Term Use of Everolimus in Patients with Tuberous Sclerosis …, accessed August 1, 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0158476
- FDA approves everolimus for tuberous sclerosis complex-associated partial-onset seizures, accessed August 1, 2025, https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-everolimus-tuberous-sclerosis-complex-associated-partial-onset-seizures
- Nitisinone – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Nitisinone
- Nitisinone for Alkaptonuria – NIHR Innovation Observatory, accessed August 1, 2025, https://io.nihr.ac.uk/techbriefings/nitisinone-for-alkaptonuria/
- Nitisinone Becomes First and Only FDA-Approved Treatment for HGA in Adults With AKU, accessed August 1, 2025, https://www.pharmacytimes.com/view/nitisinone-becomes-first-and-only-fda-approved-treatment-for-hga-in-adults-with-aku
- Repositioning of an existing drug for the neglected tropical disease Onchocerciasis – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2840490/
- Ivermectin: repurposing a multipurpose drug for Venezuela’s …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7258829/
- Clinical Treatment of Onchocerciasis | Filarial Worms – CDC, accessed August 1, 2025, https://www.cdc.gov/filarial-worms/hcp/clinical-care/onchocerciasis.html
- Treatment of Onchocerciasis | Filarial Worms – CDC, accessed August 1, 2025, https://www.cdc.gov/filarial-worms/treatment/onchocerciasis.html
- Eflornithine hydrochloride | DrugBank Online, accessed August 1, 2025, https://go.drugbank.com/salts/DBSALT001150
- Eflornithine for the treatment of human African trypanosomiasis – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/10703208_Eflornithine_for_the_treatment_of_human_African_trypanosomiasis
- Eflornithine – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Eflornithine
- Eflornithine: Uses, Interactions, Mechanism of Action | DrugBank …, accessed August 1, 2025, https://go.drugbank.com/drugs/DB06243
- Trypanosomiasis, human African (sleeping sickness), accessed August 1, 2025, https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)
- Miltefosine (Impavido): The first oral treatment against leishmaniasis …, accessed August 1, 2025, https://www.researchgate.net/publication/9077850_Miltefosine_Impavido_The_first_oral_treatment_against_leishmaniasis
- Miltefosine: Uses, Interactions, Mechanism of Action | DrugBank Online, accessed August 1, 2025, https://go.drugbank.com/drugs/DB09031
- Miltefosine (oral route) – Side effects & dosage – Mayo Clinic, accessed August 1, 2025, https://www.mayoclinic.org/drugs-supplements/miltefosine-oral-route/description/drg-20095231
- Miltefosine – Drug Targets, Indications, Patents – Patsnap Synapse, accessed August 1, 2025, https://synapse.patsnap.com/drug/eacb3f16676d42d5977b8fb5473f5138
- Drug repositioning for personalized medicine – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3446277/
- Repurposing Drugs for Precision Medicine – Number Analytics, accessed August 1, 2025, https://www.numberanalytics.com/blog/drug-repurposing-precision-medicine-guide
- Precision Medicine through Drug Repurposing – Number Analytics, accessed August 1, 2025, https://www.numberanalytics.com/blog/precision-medicine-drug-repurposing
- How is AI used for drug repurposing in biopharma? – Patsnap Synapse, accessed August 1, 2025, https://synapse.patsnap.com/article/how-is-ai-used-for-drug-repurposing-in-biopharma
- Applications of Artificial Intelligence in Drug Repurposing – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11984889/
- Organ-on-a-Chip: A new paradigm for drug development – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7990030/
- Organ-on-a-chip meets artificial intelligence in drug evaluation – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10465229/
- How Organ-on-a-Chip Technology is Transforming Drug Development – AZoLifeSciences, accessed August 1, 2025, https://www.azolifesciences.com/article/How-Organ-on-a-Chip-Technology-is-Transforming-Drug-Development.aspx
- Revolutionizing drug development: harnessing the potential of organ-on-chip technology for disease modeling and drug discovery – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1139229/full
- Organ Chips Enable Rapid Drug Repurposing – Syntec Optics, accessed August 1, 2025, https://syntecoptics.com/organ-chips-rapid-drug-repurposing/
- Public-Private Partnerships (PPP) for Drug Development – Frost Brown Todd, accessed August 1, 2025, https://frostbrowntodd.com/public-private-partnerships-ppp-for-drug-development/
- Scientific Public Private Partnerships and Consortia – FDA, accessed August 1, 2025, https://www.fda.gov/drugs/science-and-research-drugs/scientific-public-private-partnerships-and-consortia
- Public-Private Partnerships: Compound and Data Sharing in Drug Discovery and Development – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/349292307_Public-Private_Partnerships_Compound_and_Data_Sharing_in_Drug_Discovery_and_Development
- (PDF) PUBLIC-PRIVATE PARTNERSHIPS FOR PANDEMIC PREPAREDNESS IN THE PHARMACEUTICAL SECTOR – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/392963796_PUBLIC-PRIVATE_PARTNERSHIPS_FOR_PANDEMIC_PREPAREDNESS_IN_THE_PHARMACEUTICAL_SECTOR
- What can drug repurposing mean to patients with rare diseases?, accessed August 1, 2025, https://www.eurordis.org/what-can-drug-repurposing-mean-to-patients-with-rare-diseases/
- Role of Patient Advocacy Organizations in drug repurposing and a successful repurposing case – FutureLearn, accessed August 1, 2025, https://www.futurelearn.com/info/courses/introduction-to-translational-research-for-rare-diseases/0/steps/325860
- New publication: Policy changes needed for a reliable business model in drug repurposing, accessed August 1, 2025, https://remedi4all.org/new-publication-policy-changes-needed-for-a-reliable-business-model-in-drug-repurposing/
- Orphan Medicine Incentives: How to Address the Unmet Needs of Rare Disease Patients by Optimizing the European Orphan Medicinal Product Landscape Guiding Principles and Policy Proposals by the European Expert Group for Orphan Drug Incentives (OD Expert Group) – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.744532/full
- Hybrid Policy Kick-off Event: Innovative & Sustainable Models for Drug Repurposing, accessed August 1, 2025, https://repo4.eu/research-innovation-policy-event/
- 21 CFR Part 316 — Orphan Drugs – eCFR, accessed August 1, 2025, https://www.ecfr.gov/current/title-21/chapter-I/subchapter-D/part-316
- Orphan drug development: Challenges, regulation, and success stories – PubMed, accessed August 1, 2025, https://pubmed.ncbi.nlm.nih.gov/38383975/
- Navigating challenges and opportunities in orphan medicines: A spotlight commentary on rare diseases – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11992654/
- FDA approval, clinical trial evidence, efficacy, epidemiology, and price for non-orphan and ultra-rare, rare, and common orphan cancer drug indications: cross sectional analysis | The BMJ, accessed August 1, 2025, https://www.bmj.com/content/381/bmj-2022-073242
- WVU research shows how much pharmaceutical companies are capitalizing on rare drug incentives, accessed August 1, 2025, https://wvutoday.wvu.edu/stories/2023/06/12/wvu-research-shows-how-much-pharmaceutical-companies-are-capitalizing-on-rare-drug-incentives
- Rare Disease Drug Pipeline and Clinical Trials – Pfizer, accessed August 1, 2025, https://www.pfizer.com/science/focus-areas/rare-disease/research
- DNDi – Best science for the most neglected, accessed August 1, 2025, https://dndi.org/
- Source data from neglected disease R&D pipeline review – DNDi, accessed August 1, 2025, https://dndi.org/research-development/portfolio/fatalimbalance_data/
- Development Pipeline – Bayer Global, accessed August 1, 2025, https://www.bayer.com/en/pharma/development-pipeline
- Rare Diseases are Not Rare – A Training on Rare Disease Resources – YouTube, accessed August 1, 2025, https://www.youtube.com/watch?v=kLBq6V1_wc4&pp=0gcJCfwAo7VqN5tD
- Rare versus common diseases: a false dichotomy in precision medicine – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/349557294_Rare_versus_common_diseases_a_false_dichotomy_in_precision_medicine
- Repositioning Drugs for Rare Diseases Based on Biological Features and Computational Approaches – MDPI, accessed August 1, 2025, https://www.mdpi.com/2227-9032/10/9/1784
- Rare Disease Drug Repurposing – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12053540/
- The Promise of Drug Repurposing: A Faster, Cost-Effective Path to New Therapies, accessed August 1, 2025, https://www.agilisium.com/blogs/the-promise-of-drug-repurposing-a-faster-cost-effective-path-to-new-therapies
- The many advantages of repurposing existing drugs – European Pharmaceutical Review, accessed August 1, 2025, https://www.europeanpharmaceuticalreview.com/article/122023/the-many-advantages-of-repurposing-existing-drugs/
- Drug repurposing for rare: progress and opportunities for the rare disease community – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10828010/
- The Utility of Drug Repurposing in Orphan Disease Research – Worldwide Clinical Trials, accessed August 1, 2025, https://www.worldwide.com/wp-content/uploads/2023/03/Rare-Disease-Whitepaper-Drug-Repurposing-In-Orphan-Disease-Research-20230327.pdf
- Sustainable approaches for drug repurposing in rare diseases: recommendations from the IRDiRC Task Force – University of Twente Research Information, accessed August 1, 2025, https://research.utwente.nl/en/publications/sustainable-approaches-for-drug-repurposing-in-rare-diseases-reco
- Sustainable approaches for drug repurposing in rare diseases: recommendations from the IRDiRC Task Force – OAE Publishing Inc., accessed August 1, 2025, https://www.oaepublish.com/articles/rdodj.2023.04
- Drug Repurposing in the Chemotherapy of Infectious Diseases – MDPI, accessed August 1, 2025, https://www.mdpi.com/1420-3049/29/3/635
- A Multilayer Network Approach for Guiding Drug Repositioning in Neglected Diseases, accessed August 1, 2025, https://journals.plos.org/plosntds/article?id=10.1371/journal.pntd.0004300
- The dark side of drug repurposing. From clinical trial challenges to antimicrobial resistance: analysis based on three major fields, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11094707/
- Advantages and barriers of drug repurposing. – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/figure/Advantages-and-barriers-of-drug-repurposing_fig1_354191076
- Drug repurposing: approaches, methods and considerations – Elsevier, accessed August 1, 2025, https://www.elsevier.com/industry/drug-repurposing
- Drug Repurposing Strategic Research Business Report 2024-2025 & 2030 – Patent Expiry Pressures Encourage Pharma Companies to Extend Value of Existing Assets via New Indications – ResearchAndMarkets.com, accessed August 1, 2025, https://www.businesswire.com/news/home/20250528921205/en/Drug-Repurposing-Strategic-Research-Business-Report-2024-2025-2030—Patent-Expiry-Pressures-Encourage-Pharma-Companies-to-Extend-Value-of-Existing-Assets-via-New-Indications—ResearchAndMarkets.com
- The Quest for Secondary Pharmaceuticals: Drug Repurposing/Chiral-Switches Combination Strategy | ACS Pharmacology & Translational Science, accessed August 1, 2025, https://pubs.acs.org/doi/10.1021/acsptsci.2c00151
- Drug Repurposing Market Outlook, Assessment | CAGR of 4.5%, accessed August 1, 2025, https://market.us/report/drug-repurposing-market/
- The Benefits and Pitfalls of Repurposing Drugs – PHETAIROS, accessed August 1, 2025, https://www.phetairos.com/insights/integrated-product-development/the-benefits-and-pitfalls-of-repurposing-drugs/
- Drug repurposing from the perspective of pharmaceutical companies – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5758385/
- In silico drug repurposing using molecular docking and dynamics to target the protein interaction between the SARS-CoV-2 S-glycoprotein and the ACE2 receptor. – F1000Research, accessed August 1, 2025, https://f1000research.com/articles/12-1452
- A Review of Current In Silico Methods for Repositioning Drugs and Chemical Compounds, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8340770/
- Machine Learning and Artificial Intelligence in Drug Repurposing—Challenges and Perspectives, accessed August 1, 2025, https://drugrepocentral.scienceopen.com/hosted-document?doi=10.58647/DRUGREPO.24.1.0004
- Proteomics and genomics: perspectives on drug and target discovery – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2386992/
- Bioinformatics for Rare Disease Treatment – Number Analytics, accessed August 1, 2025, https://www.numberanalytics.com/blog/bioinformatics-rare-disease-treatment
- Genomes2Drugs: Identifies Target Proteins and Lead Drugs from Proteome Data, accessed August 1, 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0006195
- pmc.ncbi.nlm.nih.gov, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11719738/#:~:text=APPLICATIONS%20AND%20IMPACT-,The%20application%20of%20AI%20in%20drug%20discovery%20for%20neglected%20diseases,potential%20drug%20candidates%20for%20malaria.
- Machine learning-based drug-drug interaction prediction: a critical review of models, limitations, and data challenges – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1632775/full
- Computational drug repurposing: approaches, evaluation of in silico resources and case studies – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/389972642_Computational_drug_repurposing_approaches_evaluation_of_in_silico_resources_and_case_studies
- Applications of Genome-Wide Screening and Systems Biology Approaches in Drug Repositioning – MDPI, accessed August 1, 2025, https://www.mdpi.com/2072-6694/12/9/2694
- Systems biology platform for efficient development and translation of multitargeted therapeutics – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/systems-biology/articles/10.3389/fsysb.2023.1229532/full
- Computational/in silico methods in drug target and lead prediction – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7673338/
- In Silico Target Prediction – Creative Biolabs, accessed August 1, 2025, https://www.creative-biolabs.com/drug-discovery/therapeutics/in-silico-target-prediction.htm
- Machine learning approaches and databases for prediction of drug …, accessed August 1, 2025, https://academic.oup.com/bib/article/22/1/247/5681786
- Innovation and the Orphan Drug Act, 1983-2009: Regulatory and Clinical Characteristics of Approved Orphan Drugs – Rare Diseases and Orphan Products – NCBI, accessed August 1, 2025, https://www.ncbi.nlm.nih.gov/books/NBK56187/
- Drug Repurposing Discussion | Office of Innovation and Economic Development, The Ohio State University, accessed August 1, 2025, https://oied.osu.edu/drug-repurposing-discussion
- What is the process of expanding a drug patent by changing the molecule (or formulation etc.) called again? – Patsnap Synapse, accessed August 1, 2025, https://synapse.patsnap.com/article/what-is-the-process-of-expanding-a-drug-patent-by-changing-the-molecule-or-formulation-etc-called-again
- Patents and Exclusivity | FDA, accessed August 1, 2025, https://www.fda.gov/media/92548/download
- Drug patent Navigating Drug Patents: A Guide for Entrepreneurs – FasterCapital, accessed August 1, 2025, https://fastercapital.com/content/Drug-patent-Navigating-Drug-Patents–A-Guide-for-Entrepreneurs.html
- Navigating Drug Patents: A Comprehensive Strategy Involves Monitoring New Filings, Expirations, and Litigation. – GeneOnline, accessed August 1, 2025, https://www.geneonline.com/navigating-drug-patents-a-comprehensive-strategy-involves-monitoring-new-filings-expirations-and-litigation/
- ClinicalTrials.gov: Home, accessed August 1, 2025, https://clinicaltrials.gov/
- Drug Repurposing Data Package – DrugBank Online, accessed August 1, 2025, https://go.drugbank.com/data_packages/drug_repurposing
- Drug Repurposing Online – Gold standard drug repurposing online database, accessed August 1, 2025, https://drugrepurposing.info/
- Pat-INFORMED – The Gateway to Medicine Patent Information – WIPO, accessed August 1, 2025, https://www.wipo.int/pat-informed/en/
- Evergreen Drug Patent Database – UC College of the Law, accessed August 1, 2025, https://sites.uclawsf.edu/evergreensearch/
- Thalidomide-Revisited: Are COVID-19 Patients Going to Be the Latest Victims of Yet Another Theoretical Drug-Repurposing? – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.01248/full
- Repurposing of the PDE5 Inhibitor Sildenafil for the Treatment of Persistent Pulmonary Hypertension in Neonates – Bohrium, accessed August 1, 2025, https://www.bohrium.com/paper-details/repurposing-of-the-pde5-inhibitor-sildenafil-for-the-treatment-of-persistent-pulmonary-hypertension-in-neonates/812564394813685760-11013
- Evolution of disease activity and biomarkers on and off rapamycin in 28 patients with autoimmune lymphoproliferative syndrome | Haematologica, accessed August 1, 2025, https://haematologica.org/article/view/7986
- Familial Mediterranean Fever (FMF): What It Is & Symptoms, accessed August 1, 2025, https://my.clevelandclinic.org/health/diseases/familial-mediterranean-fever
- Rilonacept for Treatment of Familial Mediterranean Fever (FMF) – ClinicalTrials.gov, accessed August 1, 2025, https://clinicaltrials.gov/study/NCT00582907
- Re-evaluation of MEFV carriers previously diagnosed with FMF: a colchicine discontinuation study – Oxford Academic, accessed August 1, 2025, https://academic.oup.com/rheumatology/advance-article-pdf/doi/10.1093/rheumatology/keaf340/63484955/keaf340.pdf
- Colchicine, Biologic Agents and More for the Treatment of Familial Mediterranean Fever. The Old, the New, and the Rare – PubMed, accessed August 1, 2025, https://pubmed.ncbi.nlm.nih.gov/26572612/
- Repurposing the orphan drug nitisinone to control the transmission of African trypanosomiasis | PLOS Biology – Research journals, accessed August 1, 2025, https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3000796
- Dapsone (oral route) – Side effects & dosage – Mayo Clinic, accessed August 1, 2025, https://www.mayoclinic.org/drugs-supplements/dapsone-oral-route/description/drg-20063327
- Dapsone: Leprosy Uses, Warnings, Side Effects, Dosage – MedicineNet, accessed August 1, 2025, https://www.medicinenet.com/dapsone_antibacterial/article.htm
- Dapsone – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Dapsone
- Dapsone – American Osteopathic College of Dermatology (AOCD), accessed August 1, 2025, https://www.aocd.org/?page=Dapsone
- Drug repositioning: Progress and challenges in drug discovery for various diseases – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8883737/
- Challenges for Drug Repurposing in the COVID-19 Pandemic Era – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.588654/full
- Intellectual Property Rights and Regulatory Considerations Throughout Drug Repurposing | Request PDF – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/publication/383522148_Intellectual_Property_Rights_and_Regulatory_Considerations_Throughout_Drug_Repurposing
- The role of IP in strategies for repurposing medicines – Pinsent Masons, accessed August 1, 2025, https://www.pinsentmasons.com/out-law/analysis/the-role-of-ip-strategies-repurposing-medicines
- Off-Label Medication: From a Simple Concept to Complex Practical Aspects – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8508135/
- Repurposing Old Drugs for New Uses in Innovative Cancer Care | Emory University, accessed August 1, 2025, https://winshipcancer.emory.edu/magazine/issues/2024/spring/features/repurposing-old-drugs-for-new-uses-in-innovative-cancer-care/index.html
- Clinical Trials in Rare Disease: Challenges and Opportunities – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3964003/
- Pathways for non-manufacturers to drive generic drug repurposing for cancer in the U.S., accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1419772/full
- Examples of repurposed drugs for NTDs | Download Table – ResearchGate, accessed August 1, 2025, https://www.researchgate.net/figure/Examples-of-repurposed-drugs-for-NTDs_tbl2_256076547
- View of The dark side of drug repurposing. From clinical trial challenges to antimicrobial resistance: analysis based on three major fields – AboutScience, accessed August 1, 2025, https://journals.aboutscience.eu/index.php/dti/article/view/3019/3558
- Drug Repositioning in Rare/Orphans and Neglected Diseases – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/drug-repositioning-concept-classification-methodology-and-importance-in-rare-orphans-and-neglected-diseases/
- Drug Repositioning: New Approaches and Future Prospects for Life-Debilitating Diseases and the COVID-19 Pandemic Outbreak – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7551028/
- Current Drug Repurposing Strategies for Rare Neurodegenerative Disorders – Frontiers, accessed August 1, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2021.768023/full
- The Role of AI in Drug Discovery: Challenges, Opportunities, and Strategies – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10302890/
- Public Private Partnerships: Convene meetings to accelerate drug development, accessed August 1, 2025, https://www.nia.nih.gov/research/milestones/research-resources/public-private-partnerships-convene-meetings-accelerate-drug
- International regulatory and publicly-funded initiatives to advance drug repurposing, accessed August 1, 2025, https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2024.1387517/full
- Drug repositioning: current approaches and their implications in the precision medicine era – CONICET, accessed August 1, 2025, https://ri.conicet.gov.ar/bitstream/handle/11336/94633/CONICET_Digital_Nro.68168c01-26b2-4ca6-ab33-3950d6f2e7f6_A.pdf?sequence=2&isAllowed=n
- Impact of Precision Medicine on Drug Repositioning and Pricing: A Too Small to Thrive Crisis, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6313451/
- accessed December 31, 1969, https://www.who.int/news/item/13-03-2023-who-starts-review-of-miltefosine-for-the-treatment-of-leishmaniasis