The pharmaceutical industry is in constant evolution, driven by innovation, patient needs, and economic realities. Within this dynamic environment, biosimilars have emerged as a pivotal force, poised to transform healthcare access and affordability. But what exactly are biosimilars, and how do they navigate the complex regulatory pathways to reach patients? This article delves into the intricate world of biosimilar approvals, focusing specifically on the robust frameworks established by two of the world’s leading regulatory bodies: the European Medicines Agency (EMA) and the U.S. Food and Drug Administration (FDA).
The journey of a biosimilar from concept to market is a testament to scientific rigor and regulatory oversight. It’s a journey that promises to alleviate the burden of high healthcare costs, democratize access to life-saving treatments, and foster a more competitive pharmaceutical landscape. As we unravel the nuances of EMA and FDA approvals, we’ll explore the scientific principles underpinning biosimilarity, the differences and similarities in their regulatory approaches, recent trends, and the profound impact these medicines are having on global health.
Understanding Biosimilars: More Than Just Generics
When we talk about biosimilars, it’s crucial to understand that they are not simply “generic versions” of biological medicines in the same way that a generic ibuprofen is a chemical copy of brand-name ibuprofen. The analogy falls short because biologics are vastly more complex. Think of it this way: a small molecule drug is like a simple brick, easy to replicate. A biologic, however, is more akin to a complex, intricately designed house, built with biological materials and processes. Even with the same blueprints, subtle differences in the construction process can lead to variations.
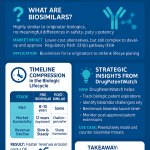
What Defines a Biosimilar?
A biosimilar is a biological medicinal product that is highly similar to an already approved reference biological medicine, also known as the “originator” or “innovator” product. This “high similarity” is the cornerstone of biosimilar development and regulation. It means that while not identical due to the inherent variability of biological systems and manufacturing processes, there are no clinically meaningful differences between the biosimilar and its reference product in terms of safety, purity, and potency (which encompasses safety and effectiveness).
The active substance in a biosimilar is fundamentally the same as that of the reference product, and they are expected to have the same mechanism of action, dosage form, strength, and route of administration. The goal of a biosimilar development program is not to independently establish the safety and effectiveness of the proposed product from scratch, but rather to demonstrate its biosimilarity to the already approved reference product. This abbreviated approval pathway is what allows for faster development and, ultimately, more affordable options for patients.
The Scientific Foundation of Biosimilarity
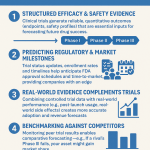
Demonstrating biosimilarity is a multi-faceted scientific endeavor. It begins with an exhaustive analytical comparison of the proposed biosimilar to the reference product. This includes detailed structural and functional characterization studies. Scientists meticulously analyze the molecular structure, post-translational modifications, and biological activity of both products.
Following extensive analytical comparability, the development program may include:
- Non-clinical (animal) studies: These studies provide toxicology and pharmacology information for the biosimilar as needed.
- Clinical pharmacology studies: These assess how the proposed biosimilar moves through the body (pharmacokinetics or PK) and its effects on the body (pharmacodynamics or PD). They also often include immunogenicity assessments to evaluate a patient’s immune response to the biosimilar.
- Comparative clinical studies: These are conducted to address any remaining uncertainties about clinically meaningful differences between the biosimilar and the reference product. However, it’s important to note that a full battery of clinical trials, as required for an original biologic, is typically not necessary for a biosimilar.
The “totality of the evidence” is the guiding principle for both the EMA and FDA. This means that regulatory agencies consider all available data and information, from analytical characterization to clinical studies, to determine if a proposed biosimilar is indeed highly similar to its reference product.
The European Medicines Agency (EMA) and its Pioneering Role
Europe has long been a trailblazer in the regulation and adoption of biosimilar medicines. The EMA, responsible for evaluating the majority of applications to market biosimilar medicines in the European Union (EU), approved the first biosimilar in 2006. This early start has provided the EU with significant experience and a robust framework that has influenced global biosimilar development.
EMA’s Regulatory Framework: A Centralized Approach
The EMA’s approval process for biosimilars operates under a centralized procedure, meaning a single application, a single evaluation, and a single authorization grant direct access to the entire European Union market. This streamlined approach benefits manufacturers and facilitates broader patient access across member states.
The EMA emphasizes a comprehensive comparability exercise that includes:
- Quality comparability studies: These are the initial and foundational studies, involving extensive analytical and functional data to confirm the biosimilar’s structural and biological characteristics are highly similar to the reference product.
- Non-clinical and clinical studies: The extent of these studies is determined based on the quality comparability data, with the aim of ruling out any clinical performance differences. The EMA has even been exploring a “tailored clinical approach,” which could potentially reduce the amount of clinical data required for approval if strong analytical and pharmacokinetic data are presented. This reflects a maturing regulatory approach, acknowledging the extensive safety record of biosimilars and advancements in analytical technologies.
A key aspect of the EMA’s approach is that biosimilars can only be authorized once the period of data exclusivity on the reference biological medicine has expired. This typically means the reference medicine must have been authorized for at least eight years before a biosimilar application can be considered.
Interchangeability in the EU
The EMA and the Heads of Medicines Agencies (HMA) have stated that biosimilars approved in the EU are interchangeable from a scientific viewpoint. This means that, from a scientific perspective, a biosimilar can be used instead of its reference product, or vice versa, without compromising safety or efficacy. However, the practical implications of interchangeability, such as pharmacy-level substitution, often depend on national health authorities and their specific policies. This is a critical distinction that sometimes leads to confusion among prescribers and patients, and continuous education is vital.
The U.S. Food and Drug Administration (FDA) and its Evolving Pathway
While Europe led the way, the U.S. FDA established its biosimilar approval pathway with the enactment of the Biologics Price Competition and Innovation Act (BPCIA) as part of the Affordable Care Act in 2010. This legislation created an abbreviated licensure pathway for biological products demonstrated to be “biosimilar” to or “interchangeable” with an FDA-approved reference biological product.
FDA’s Regulatory Framework: A Stepwise Approach
The FDA’s approach to biosimilar approval is characterized by a “stepwise” process, starting with robust analytical comparison and progressing through additional studies as necessary. The FDA evaluates each biosimilar on a case-by-case basis, providing guidance to manufacturers on the scope of testing required.
The core components of an FDA biosimilar application typically include:
- Analytical studies: These are the cornerstone, providing extensive data on the structural and functional similarity of the proposed biosimilar to the reference product.
- Animal studies: Conducted as necessary to provide toxicology or pharmacology information.
- Clinical pharmacology studies: To demonstrate that the proposed biosimilar moves through the body similarly and has the same effects as the reference product. This often includes immunogenicity assessment.
- Additional clinical studies: May be required if there is any remaining uncertainty after the earlier studies. However, the FDA’s goal is to avoid unnecessary duplication of clinical trials.
The FDA may approve a biosimilar for an indication or patient population without direct studies in that specific indication, provided the manufacturer offers adequate scientific justification based on all available information in the application, the FDA’s previous finding of safety and efficacy for the reference product’s approved indications, and consideration of various scientific factors. This is known as “extrapolation” of indications and is a crucial aspect of the abbreviated pathway, allowing biosimilars to be used for all or some of the conditions for which the reference product is approved.
The Concept of Interchangeability in the U.S.
A unique aspect of the FDA’s framework is the concept of “interchangeability.” A biosimilar product that meets additional requirements can be approved as an interchangeable biosimilar. This designation is significant because it allows for substitution for the reference product at the pharmacy level without the intervention of the prescriber, depending on state pharmacy laws.
To achieve interchangeability, a manufacturer must demonstrate not only biosimilarity but also that:
- The proposed interchangeable product is expected to produce the same clinical result as the reference product in any given patient.
- For a product administered more than once to an individual, switching between the proposed interchangeable product and the reference product does not increase safety risks or decrease effectiveness compared to using the reference product without such switching.1
This often requires a “switching study” where patients alternate between the reference product and the interchangeable product multiple times. The interchangeability designation is seen as a key driver for biosimilar uptake in the U.S. market, as it removes a potential barrier for pharmacists and patients.
Key Differences and Similarities in EMA and FDA Approaches
While both the EMA and FDA are committed to ensuring the safety, efficacy, and quality of biosimilars, their regulatory approaches have some distinct differences and notable similarities.
Similarities: Core Principles
Both agencies share fundamental principles:
- Totality of the Evidence: Both rely on a comprehensive evaluation of all available data (analytical, non-clinical, clinical) to establish biosimilarity.
- No Clinically Meaningful Differences: The ultimate goal for both is to ensure that the biosimilar has no clinically meaningful differences from its reference product.
- Rigorous Standards: Despite the abbreviated pathway, both maintain rigorous standards for quality, safety, and efficacy for biosimilar approval, aligning with the high standards applied to all biological medicines.
- Focus on Comparability: The bedrock of both regulatory systems is the comparative nature of biosimilar development, rather than independent efficacy and safety trials.
Differences: Nuances in Application
Despite these commonalities, there are several key differences:
- Definition of Biosimilarity: While conceptually similar, the precise wording in their definitions can vary. The FDA defines biosimilars as “highly similar” with “no clinically meaningful differences in safety, purity, and potency.” The EMA defines them as “biological medicinal products containing the same active substance as the reference product and similar in quality characteristics, biological activity, safety, and efficacy.” These subtle differences can sometimes lead to different interpretations during development.
- Interchangeability: As discussed, the FDA has a distinct “interchangeable” designation, allowing pharmacy-level substitution. The EMA, while asserting scientific interchangeability, defers to national authorities for practical substitution policies. This is a significant differentiator in market dynamics.
- Reference Product Sourcing: When a biosimilar has both U.S. and EU reference products, sponsors often need to conduct “bridging studies” comparing the biosimilar to both the U.S.-licensed and EU-approved reference products, and also comparing the two reference products to each other. The EMA permits the use of foreign-approved comparators with certain caveats, whereas the FDA often requires these “three-way comparisons” to ensure comparability to the U.S.-licensed product. This can add complexity and cost to global development programs.
- Data Exclusivity Periods: While both have data exclusivity periods for reference products, the specific durations and interpretations can vary, impacting when biosimilars can enter the market in each region.
- Evolution of Guidelines: Both agencies continually refine their guidelines based on scientific advancements and accumulated experience. However, the pace and nature of these refinements can differ, presenting a dynamic regulatory landscape for developers.
Recent Trends in Biosimilar Approvals (2023-2025)
The biosimilar landscape is experiencing a surge in activity, particularly in the period from 2023 to 2025. This acceleration is driven by the expiry of patents for numerous blockbuster biologics, creating significant market opportunities.
FDA Approvals: A Record-Breaking Momentum
The FDA has witnessed a remarkable increase in biosimilar approvals. 2024 saw the highest number of biosimilars approved by the FDA in a calendar year, with 19 biosimilars greenlit, a sharp jump from the five approved in 2023. Projections suggest that 2025 could surpass even this milestone.
Notable FDA approvals in 2024 and early 2025 include:
- Ustekinumab biosimilars: Several biosimilars referencing Johnson & Johnson’s blockbuster autoimmune drug Stelara (ustekinumab) have gained FDA approval, including Wezlana (ustekinumab-auub) in 2024, followed by Starjemza (ustekinumab-hmny), Steqeyma (ustekinumab-stba), and Yesintek (ustekinumab-kfce) in late 2024 and early 2025. Stelara generated over $10 billion in sales in 2023, making its biosimilar competition a significant event.
- Aflibercept biosimilars: Five new biosimilars referencing Regeneron’s ophthalmology drug Eylea (aflibercept) received FDA approval in 2024. Eylea also had substantial sales, highlighting the impact of biosimilar entry in this therapeutic area.
- Denosumab biosimilars: Multiple denosumab biosimilars, referencing Xgeva and Prolia, such as Bomyntra (denosumab-bnht), Conexxence (denosumab-bnht), Osenvelt (denosumab-bmwo), Stoboclo (denosumab-bmwo), Ospomyv (denosumab-dssb), and Xbryk (denosumab-dssb) were approved in early 2025 for osteoporosis and cancer-induced bone loss.
- Omalizumab biosimilars: Omlyclo (omalizumab-igec) referencing Xolair (omalizumab) was approved in March 2025 for asthma.
- Insulin Aspart biosimilar: Merilog (insulin aspart-szjj) was approved in February 2025 as an affordable option for diabetes care, referencing Novolog (insulin aspart).
This surge reflects a broader governmental push in the U.S. to increase biosimilar use to drive down prescription drug costs. The FDA continues to expedite the development of lower-cost generic medicines and biosimilars, recognizing their potential to enhance patient access.
EMA Approvals: Continued Leadership
Europe continues to be a leader in biosimilar adoption, and the EMA has maintained a steady pace of approvals. While specific numbers for 2024 and 2025 approvals might vary depending on the reporting period, the trend remains one of consistent growth.
Recent EMA approvals, often mirroring or preceding FDA approvals due to earlier patent expirations in Europe, include biosimilars for:
- Denosumab: Jubereq (denosumab) and Osvyrti (denosumab) were approved by the EMA in March 2025 for skeletal-related events in advanced malignancies and prostate cancer, respectively.
- Pegfilgrastim: Dyrupeg (pegfilgrastim) was approved in January 2025, which supports white blood cell production during chemotherapy.
The EMA is actively proposing streamlined approval processes for biosimilars to further enhance patient access. A public consultation period for a proposal that focuses on structural and functional comparability along with pharmacokinetic data, potentially reducing or eliminating the need for extensive clinical efficacy studies, is open until September 2025, with implementation expected in 2026 if approved. This signals a forward-thinking approach, recognizing the maturity of the biosimilar field.
Impact on Healthcare Systems and Patients
The growing number of biosimilar approvals by the EMA and FDA has profound implications for healthcare systems, patients, and the broader pharmaceutical market.
Cost Savings and Increased Access
Perhaps the most tangible benefit of biosimilars is their ability to generate significant cost savings. Biologics are among the most expensive therapies, and their high price tags can create access barriers for patients and strain healthcare budgets. Biosimilars introduce competition, which drives down prices.
- Illustrative Statistic: In the European Union, biosimilar competition has led to price reductions as high as 80% off the original biologic drug in some instances. The UK and Germany, early adopters of biosimilars, have saved millions.
- Industry Quote: “Biosimilars are not just a budget solution—they’re a long-term path to more access, better outcomes and a more just healthcare system,” according to an article in the Los Angeles Times [1].
For patients, lower drug prices translate to reduced out-of-pocket expenses, potentially leading to fewer treatment delays and improved adherence. For healthcare systems, these savings free up resources that can be reinvested in newer treatments, expanded patient services, or other critical areas.
Fostering Competition and Innovation
The introduction of biosimilars challenges the market dominance of innovator biologics, encouraging a more competitive environment. This competition can stimulate further innovation by compelling innovator companies to develop next-generation therapies or explore new indications for their existing products. It also incentivizes biosimilar manufacturers to invest in research and development, not just for new biosimilars but also potentially for novel biologics down the line.
Challenges to Adoption
Despite the undeniable benefits, the widespread adoption of biosimilars still faces hurdles:
- Physician and Patient Education: There’s an ongoing need to educate healthcare professionals and patients about the safety and efficacy of biosimilars. Misconceptions, often fueled by originator companies, can create hesitancy. A significant barrier to biosimilar adoption is the lack of comprehensive understanding among key stakeholders, as noted by DrugPatentWatch [7].
- Payer Policies and Rebate Traps: Innovator companies sometimes offer substantial rebates to payers, making it difficult for biosimilars to compete on price, even if their list price is lower. Step therapy requirements by some insurers, mandating patients try the reference product first, can also impede biosimilar uptake.
- Naming Conventions: In the U.S., FDA-approved biosimilars are assigned a four-letter suffix to their core name (e.g., ustekinumab-auub). While intended for pharmacovigilance, some argue this naming convention inadvertently suggests differences between biosimilars and reference products, potentially affecting perceptions.
The Future of the Biosimilar Landscape
The trajectory of the biosimilar market is unequivocally upward. Several factors indicate continued growth and evolution.
Impending Patent Expirations
A significant driver for future growth is the wave of upcoming patent expirations for blockbuster biologics. Data from GlobalData indicates that 18 biologics are set to lose patent protection in 2025, up from 14 in 2024. This includes highly anticipated products like Amgen’s Prolia (denosumab) and Roche’s Perjeta (pertuzumab), opening vast new opportunities for biosimilar development. Between now and 2030, a substantial number of biologics in both Europe and the U.S. will lose exclusivity, creating a market opportunity far larger than in previous decades.
Market Growth Projections
The global biosimilars market is projected for substantial growth. Estimates vary slightly, but the consensus is clear:
- Coherent Market Insights estimates the global biosimilars market to be valued at USD 42.53 billion in 2025 and reach USD 136.37 billion by 2032, exhibiting a compound annual growth rate (CAGR) of 18.1% [2].
- Fortune Business Insights anticipates the market to reach USD 175.99 billion by 2034, growing at a robust CAGR of 17.78% from its 2025 valuation of approximately USD 40.36 billion [3].
- ResearchAndMarkets.com projects the market to reach US93.1billionby2030fromUS34.8 billion in 2024, with a CAGR of 17.8% [4].
These projections underscore the increasing demand for affordable options and the growing trust in biosimilars.
Harmonization and Streamlined Approvals
There’s a growing call for greater global harmonization in biosimilar regulatory requirements. While complete uniformity may be challenging, efforts to align guidelines and reduce the need for redundant studies across regions would significantly benefit developers and accelerate patient access. The EMA’s proposed streamlined approval process, potentially reducing the need for extensive clinical efficacy studies, is a step in this direction, and the FDA is also exploring ways to optimize its review processes.
Expansion into New Therapeutic Areas
Historically, biosimilar development has concentrated heavily on oncology and immunology, given the high cost and prevalence of biologic treatments in these areas. However, as the market matures, we can expect to see an expansion into other therapeutic areas where biologics play a crucial role, such as diabetes (with insulin biosimilars already making strides), ophthalmology, and various rare diseases.
The Role of DrugPatentWatch and Market Intelligence
In this rapidly evolving landscape, tools and insights from platforms like DrugPatentWatch become invaluable for business professionals. DrugPatentWatch offers strategies for biosimilar developers to navigate regulatory agency interactions, identify hurdles, and leverage real-world evidence to accelerate approval timelines [7]. Understanding patent expiry dates, market intelligence on emerging biosimilar pipelines, and regulatory nuances across different regions are critical for strategic decision-making and achieving market domination.
As Juliana Reed, executive director of the Biosimilars Forum, stated, “We are pleased to see meaningful action on several fronts, including reforms to make biosimilars available quickly and efficiently to all Americans who need them.” This sentiment encapsulates the collective ambition of the biosimilar industry.
Conclusion
The biosimilar landscape is a vibrant and critical component of modern healthcare. The robust regulatory frameworks established by the EMA and FDA, though with their own distinct nuances, serve as cornerstones for ensuring the safety, efficacy, and quality of these vital medicines. From the meticulous analytical comparability studies to the strategic clinical trials, every step in the approval process is designed to build confidence in biosimilars.
The increasing pace of approvals, driven by patent expiries and a global push for cost containment, is transforming market dynamics. Biosimilars are not just alternatives; they are essential drivers of competition, affordability, and broader patient access to life-changing therapies. While challenges remain, particularly in education and overcoming market access barriers, the future of biosimilars is undeniably bright. As these innovative medicines continue to gain traction, they hold the promise of a more sustainable and equitable healthcare system for all.
Key Takeaways
- Biosimilars are highly similar biological medicines, not generic copies: They undergo rigorous comparative testing against reference biologics to ensure no clinically meaningful differences in safety, purity, and potency.
- EMA is a pioneer in biosimilar regulation: It approved the first biosimilar in 2006 and operates a centralized approval process for the EU market, emphasizing scientific interchangeability.
- FDA established its pathway under the BPCIA: It uses a stepwise approach and uniquely offers an “interchangeable” designation, allowing pharmacy-level substitution.
- Regulatory differences exist but core principles are shared: Both agencies prioritize a “totality of the evidence” approach and rigorous standards, but differ on aspects like interchangeability practicalities and reference product sourcing for global development.
- Biosimilar approvals are accelerating: Driven by significant patent expirations of blockbuster biologics (e.g., Stelara, Eylea, Prolia), both the FDA and EMA have seen a surge in approvals from 2023-2025.
- Profound impact on healthcare: Biosimilars drive significant cost savings, increase patient access to treatments, and foster market competition, with projections indicating robust market growth in the coming years.
- Challenges remain: These include the need for ongoing education for healthcare professionals and patients, and overcoming market access hurdles like payer policies and brand loyalty.
- Market intelligence is crucial: Resources like DrugPatentWatch are vital for navigating the complex regulatory and commercial landscape of biosimilars.
5 Unique FAQs
Q1: If biosimilars are “highly similar,” does that mean they are less effective or have more side effects than the original biologic?
A1: No, absolutely not. The “highly similar” designation means that extensive analytical, non-clinical, and clinical studies have demonstrated there are no clinically meaningful differences in terms of safety, purity, and potency between the biosimilar and its reference product. Both the EMA and FDA apply rigorous standards to ensure that approved biosimilars are as safe and effective as their reference products. The slight structural differences inherent in biological manufacturing do not translate to meaningful clinical differences.
Q2: What is the significance of the “interchangeable” designation in the U.S., and why doesn’t the EU have a similar formal designation?
A2: In the U.S., an “interchangeable” biosimilar can be substituted for the reference product at the pharmacy level without the prescribing physician’s direct intervention, similar to how generic drugs are substituted. This is a powerful driver for uptake. The EU, while scientifically affirming interchangeability, leaves the practical aspects of pharmacy-level substitution to individual member states. This difference reflects varying healthcare system structures and legal frameworks, with the U.S. seeking to actively facilitate substitution through a specific regulatory pathway.
Q3: How do patent expirations of reference biologics directly influence the biosimilar market?
A3: Patent expirations are the primary catalyst for biosimilar market entry. Once a reference biologic’s key patents expire, other manufacturers are legally able to develop and seek approval for biosimilar versions. This opens the door for competition, leading to new product launches, increased treatment options, and often substantial price reductions for patients and healthcare systems. The wave of upcoming patent expirations for multi-billion dollar biologics is a major reason for the projected rapid growth in the biosimilar market.
Q4: Beyond cost savings, what other benefits do biosimilars bring to the broader healthcare ecosystem?
A4: While cost savings are paramount, biosimilars offer other critical benefits. They increase patient access to essential treatments, especially for chronic and life-threatening conditions where biologics are the standard of care but may be prohibitively expensive. They also foster competition within the pharmaceutical market, which can encourage innovation from both originator and biosimilar companies. Furthermore, increased access can lead to better health outcomes for populations by reducing treatment gaps and improving adherence.
Q5: What role does real-world evidence play in the ongoing development and perception of biosimilars?
A5: Real-world evidence (RWE), gathered from routine clinical practice rather than strictly controlled clinical trials, is becoming increasingly important for biosimilars. RWE can further reinforce confidence in biosimilar safety and effectiveness post-approval, providing additional data on long-term use and diverse patient populations. It can help address any lingering concerns among healthcare providers and patients about switching from originator biologics. Regulatory bodies are also exploring how RWE can be integrated into future regulatory processes, potentially streamlining some aspects of development and post-market surveillance.
Cited Information:
- Los Angeles Times. “How Biosimilars Lower Cancer Drug Costs for Patients.” May 21, 2025.
- Coherent Market Insights. “Biosimilars Market Trends, Share, Size & Forecast, 2025-2032.”
- Fortune Business Insights. “Biosimilars Market Outlook 2025.”
- ResearchAndMarkets.com. “Biosimilars Market Products, Applications and Regulations Overview 2025: Increasing Cost of Biologic Drugs, Leading to a Greater Demand for More Affordable Options – Global Forecasts 2024-2030.” Business Wire. March 11, 2025.
- Pharmaceutical Technology. “FDA biosimilar approvals set for record-breaking year amid US pricing reforms.” May 16, 2025.
- Aptitude Health. “Most FDA and EMA Oncology Drug Approvals in Q1 2025 Were New Indications for Biologics and Biosimilars.”
- DrugPatentWatch. “Understanding the Barriers to US Biosimilars: Navigating Challenges for Market Success.” November 4, 2024.