I. Executive Summary
The question of whether drug companies can “bribe” the U.S. Food and Drug Administration (FDA) is often raised, reflecting public concern over pharmaceutical influence. This report clarifies that direct, illegal bribery of federal officials is strictly prohibited under U.S. law, specifically 18 U.S.C. § 201, and carries severe penalties. However, the truth behind pharmaceutical influence extends far beyond overt corruption, encompassing a complex web of legal and quasi-legal mechanisms that significantly impact FDA decisions, drug development trajectories, product safety, and market pricing.
Key findings indicate that the pharmaceutical industry exerts substantial influence through several interconnected avenues. The Prescription Drug User Fee Act (PDUFA), while a catalyst for accelerating drug approvals, creates a significant financial interdependence, with user fees constituting nearly half of the FDA’s total budget and two-thirds of its human drug program budget.1 Extensive lobbying efforts, amounting to billions of dollars, directly shape legislation and regulatory policies, and studies show a correlation between lobbying and higher drug approval rates for lobbying firms.2 The “revolving door” phenomenon, where former FDA officials transition into lucrative industry positions, raises concerns about impartiality and allows for indirect, “behind-the-scenes” influence.4 Furthermore, the industry’s pervasive role in funding and conducting clinical trials introduces inherent biases in data generation and reporting, necessitating robust FDA oversight and post-market surveillance.6
Collectively, these mechanisms, while largely legal, contribute to a perception of undue influence, potentially eroding public trust and impacting public health outcomes, particularly concerning drug safety and pricing. The report concludes that maintaining the integrity of the drug approval process requires continuous vigilance, adaptive policy reforms, and enhanced transparency to ensure that the FDA’s primary mission of public health protection remains uncompromised.
II. Introduction: Navigating the Complexities of Pharmaceutical Influence
Clarifying the “Bribery” Question: Legal Definitions vs. Public Perception
The public often questions whether pharmaceutical companies can “bribe” the FDA, a term that typically implies illegal payments for favorable regulatory outcomes. This inquiry necessitates a precise legal clarification. Under U.S. federal law, direct bribery of public officials is a serious felony. Specifically, 18 U.S.C. § 201 explicitly prohibits corruptly giving or accepting anything of value with the intent to influence an official act, a clear “quid pro quo” arrangement.8 Violations of this statute can lead to severe penalties, including up to 15 years in prison and substantial fines. The law also addresses illegal gratuities, which involve providing or receiving something of value “for or because of” an official act already performed, without a prior agreement, carrying a maximum 2-year sentence.8 The critical distinction lies in the intent and timing of the exchange; bribery involves an explicit agreement to influence a future official act, whereas a gratuity is a reward for an act already completed.
However, the user’s broader query, “Unveiling the Truth Behind Pharmaceutical Influence,” suggests a public perception that “influence” might be functionally equivalent to “bribery,” even if not explicitly illegal. This highlights a significant gap between the strict legal definition of bribery and the public’s more expansive understanding of undue influence. The report’s objective is to move beyond a simplistic yes/no answer to the bribery question and instead dissect the multifaceted, often legal, mechanisms through which the pharmaceutical industry impacts FDA decisions, drug development, safety, and pricing. This approach is crucial for a comprehensive and authoritative analysis that addresses the underlying concerns about regulatory integrity and public trust.
The FDA’s Mandate: Balancing Public Health, Innovation, and Industry Engagement
The FDA’s foundational mission is to protect and promote public health by ensuring the safety, efficacy, and security of human and veterinary drugs, biological products, medical devices, and the nation’s food supply.10 The Federal Food, Drug, and Cosmetic Act (FDCA) of 1938, enacted in response to tragedies like the elixir sulfanilamide poisoning, and its subsequent amendments, empower the FDA to rigorously oversee these products, requiring evidence of safety and effectiveness before they can be marketed.10
Simultaneously, the FDA is tasked with advancing public health by accelerating the availability of innovative medicines that are more effective, safer, and more affordable.11 This dual mandate inherently requires the agency to engage extensively with the regulated industry, fostering an environment where various forms of influence can manifest. The challenge for the FDA is to strike a delicate balance: facilitating timely access to new products while preventing harm to public health.11 This report will explore how the pharmaceutical industry navigates and shapes this complex regulatory landscape, examining the various channels through which its influence is exerted and the implications for public health.
Report Scope and Structure
This report provides a comprehensive analysis of pharmaceutical industry influence on the FDA. It begins by establishing the legal and ethical frameworks governing these interactions, distinguishing illegal bribery from other forms of influence. Subsequent sections delve into the financial interdependence created by user fees, the impact of extensive lobbying and political advocacy, the implications of the “revolving door” phenomenon, the integrity of industry-sponsored research and clinical trial data, and the role of advisory committees. The report concludes by synthesizing these findings to discuss the public health and economic consequences of pharmaceutical influence and outline existing safeguards and future directions for maintaining regulatory integrity.
III. Legal and Ethical Frameworks Governing FDA-Industry Interactions
A. Prohibitions Against Bribery and Illegal Gratuities
Federal law establishes clear prohibitions against bribery and illegal gratuities involving public officials. As detailed in 18 U.S.C. § 201, it is a felony to corruptly offer, give, or promise anything of value to any public official with the intent to influence an official act, or for a public official to corruptly demand, seek, receive, or accept anything of value in return for being influenced in the performance of an official act.8 This “quid pro quo” exchange is the hallmark of bribery, punishable by up to 15 years in prison and fines up to three times the value of the bribe. The statute also addresses illegal gratuities, which involve giving or receiving something of value “for or because of” any official act performed or to be performed, without the explicit intent to influence a future act. Gratuities carry a lesser penalty of up to two years in prison.8 This legal distinction is critical: while both involve improper benefits, bribery implies a direct exchange for a specific official action, whereas a gratuity is a reward for an action already taken or a general attempt to “curry favor”.8
The FDA, as a federal agency, operates under these stringent laws and maintains its own robust internal ethics policies and oversight mechanisms to prevent conflicts of interest. The agency’s Office of Ethics and Integrity (OEI) is tasked with providing advice and assistance to current and former employees to ensure that their decisions and actions are not, nor appear to be, tainted by any conflict of interest.14 The OEI provides mandatory ethics training to all new FDA employees within 90 days of their start date and administers annual ethics training for all staff. It also counsels employees on statutory, regulatory, and policy requirements regarding ethics and conflict of interest, and monitors compliance with financial disclosure systems.14 Beyond internal FDA policies, the FDA Alumni Association (FDAAA) has its own Code of Ethics, prohibiting members from using their affiliation to advance private economic interests, disclosing confidential information obtained from the FDA, or engaging in lobbying activities through their membership.15 These comprehensive legal and internal frameworks aim to establish a clear boundary against direct corruption.
B. Conflicts of Interest and Financial Disclosure
Beyond direct bribery, federal law broadly prohibits conflicts of interest that could compromise the integrity of government decisions. Specifically, 18 U.S.C. § 208(a) prohibits all federal employees, including Special Government Employees (SGEs) who serve on advisory committees, from participating in any particular government matter that will have a “direct and predictable effect” on their financial interests.16 This prohibition is extensive, covering not only the individual’s direct financial holdings but also those of their spouse, minor children, business partners, employer, and any organizations in which they serve as an officer, director, or trustee.16
To manage these potential conflicts, the FDA implements a rigorous screening process for advisory committee members. Prior to an advisory committee meeting, SGEs are required to complete FDA Form 3410, a Confidential Financial Disclosure Report, which identifies any financial interests that could conflict with the meeting topic.16 The FDA then reviews these reports to determine if a conflict exists.17 In certain circumstances, waivers can be granted under 18 U.S.C. § 208(b)(2) if the financial interest is deemed “too remote or too inconsequential to affect the integrity of the services of the SGE”.16 Waivers may also be issued if the need for the SGE’s unique scientific expertise outweighs the potential for a conflict of interest, provided specific criteria are met and the information is publicly disclosed within specified timeframes before the advisory committee meetings.17 This public disclosure is a key mechanism for transparency, allowing external parties to scrutinize potential biases.
The legal framework surrounding FDA-industry interactions establishes a clear boundary against direct bribery, but it simultaneously acknowledges and attempts to manage a wide array of financial relationships that, while legal, can still create perceived or actual biases. The very existence of extensive conflict-of-interest regulations, internal ethics offices, and broader anti-corruption laws indicates that the legal system recognizes and attempts to manage a wide array of potentially biasing financial relationships and influence tactics within the broader pharmaceutical ecosystem. This means that while direct bribery of FDA regulators might be rare and severely punished, the ongoing efforts to manage conflicts of interest and the legality of financial relationships are a constant focus. The legal framework attempts to draw lines, but the continuous need for vigilance to maintain regulatory integrity remains.
A crucial element in mitigating perceived conflicts of interest and fostering public trust is transparency. The explicit mention of public disclosure of financial interests and waivers for FDA advisory committee members 16 underscores this principle. Furthermore, the Physician Payments Sunshine Act (Open Payments) mandates the public reporting of financial relationships between pharmaceutical companies and healthcare providers.18 The public debarment lists for companies sanctioned for fraud or integrity issues 20 and the whistleblower provisions leading to large settlements 21 also contribute to this transparency. The consistent theme of mandated public visibility suggests that legal and regulatory bodies view transparency as a key safeguard against undue influence. The underlying assumption is that if financial ties are public, they can be scrutinized, and their potential to influence decisions can be assessed by external parties, including the public, media, and other experts. The effectiveness of this transparency, however, depends on public awareness, accessibility of data, and the ability of stakeholders to interpret complex financial information and connect it to regulatory outcomes.
C. Broader Anti-Corruption Measures
Beyond direct bribery and conflicts of interest within the FDA, broader anti-corruption laws apply to the pharmaceutical industry, indirectly impacting its interactions within the healthcare ecosystem. The Anti-Kickback Statute (AKS), codified at 42 U.S.C. §1320a-7b(b), is a federal anti-fraud law that criminalizes offering or paying “anything of value” to induce someone to purchase, prescribe, or recommend a product reimbursed by federal health programs.21 While the AKS primarily targets interactions between pharmaceutical companies and healthcare professionals (HCPs) – preventing remuneration like cash, gifts, lavish meals, or extravagant speaking fees as incentives for prescribing drugs – its violations can lead to severe consequences.21 Penalties include up to 5 years in prison and fines of approximately $25,000 per offense, with the Department of Justice (DOJ) prosecuting these cases.21 Additionally, the HHS Office of Inspector General (OIG) can impose civil monetary penalties and exclude violators from federal healthcare programs like Medicare and Medicaid, a sanction often described as a “corporate death sentence” in the healthcare industry.21
Closely linked to the AKS is the False Claims Act (FCA), a Civil War-era anti-fraud law (31 U.S.C. §§3729–3733) that allows the U.S. government to recover treble damages and penalties for false or fraudulent claims submitted for payment.21 In the pharmaceutical context, the FCA is a powerful enforcement tool against schemes such as off-label promotion (promoting drugs for unapproved uses) and kickbacks. Even if a drug is prescribed for a legitimate use, if the claim for payment to a federal program (like Medicare or Medicaid) is tainted by a kickback, it is considered a false claim under the FCA.21 The FCA’s “qui tam” (whistleblower) provisions are particularly potent, incentivizing insiders with knowledge of wrongdoing to file lawsuits on behalf of the government, leading to numerous high-profile settlements. For example, Biogen paid $900 million in 2022 for alleged kickbacks, and Johnson & Johnson paid $2.2 billion in 2013 for off-label promotion and related kickbacks.21 The DOJ recovered $1.67 billion from healthcare fraud cases in FY2024, mostly involving pharmaceutical or medical device industries.21
Finally, the FDA possesses the authority to debar individuals and entities, legally prohibiting them from participating in certain activities within FDA-regulated industries, such as submitting product applications or importing regulated products.20 This action typically follows a conviction for serious violations of the Federal Food, Drug, and Cosmetic Act (FDCA) related to abuse, fraud, or integrity issues. The FDCA itself prohibits the misbranding of drugs, which includes false or misleading advertising or labeling, and mandates that prescription drug advertisements be truthful, balanced (presenting both benefits and risks), and promote only FDA-approved uses.21 Violations can result in product seizures, injunctions, or criminal charges.21 These laws collectively create a legal environment designed to deter and punish corrupt practices, even if they do not directly address the more subtle forms of influence.
IV. Financial Interdependence: The Prescription Drug User Fee Act (PDUFA)
A. PDUFA’s Origins and Operational Model
The genesis of the Prescription Drug User Fee Act (PDUFA) in 1992 was a direct response to a critical bottleneck in new medicine approvals at the FDA. Prior to PDUFA, the agency faced significant challenges due to understaffing and underfunding, leading to protracted review times. It was common for the FDA to take more than two years to review new drug applications, and over 70% of new medicines were initially approved outside the United States.22 This delay, often referred to as “drug lag,” spurred calls for reform. Historically, the FDA had resisted the concept of user fees, viewing its regulatory activities as a public benefit that should be funded by taxpayers, not the industry it regulated.25
The legislative landscape shifted in 1992 when, with cooperation between the FDA and the drug industry, PDUFA was signed into law. This act allowed the FDA to collect fees from drug manufacturers to specifically fund the new drug approval process.26 A crucial element of this agreement was the commitment that these fees would supplement, rather than replace, federal appropriations, and that the FDA would agree to target completion times for reviews.23 PDUFA is not a permanent fixture; its user fee programs require reauthorization by Congress every five years, with the current agreement in effect through September 2027.23 This periodic reauthorization provides a mechanism for ongoing negotiation and adjustment of the program’s terms and performance goals between the FDA and the biopharmaceutical industry.22
The financial impact of PDUFA on the FDA’s budget has been substantial, fundamentally altering its funding structure. In fiscal year (FY) 2022, user fees constituted 46% ($2.9 billion) of the FDA’s total budget of $6.2 billion.1 This represents a significant shift from FY 1992, when the FDA’s budget was entirely supported by congressional appropriations.1 The reliance on user fees is even more pronounced within specific programs; in FY2022, user fees accounted for 66% ($1.4 billion) of the human drugs program budget, 43% ($197 million) of the biologics program budget, and 35% ($228 million) of the medical device program budget.1 These fees are collected primarily through application fees (one-time payments for new drug or biologic submissions) and annual program fees paid by sponsors of approved and marketed products.1
Table 1: FDA Funding Sources (FY2022)
| Funding Source | Amount (Billions USD) | % of Total FDA Budget | % of Human Drugs Program Budget | |
| Total FDA Budget | $6.2 | 100% | – | |
| Total User Fees | $2.9 | 46% | – | |
| Human Drugs Program Budget (Total) | – | – | $1.4 (100%) | |
| Human Drugs Program User Fees | $1.4 | – | 66% | |
| Biologics Program User Fees | $0.197 | – | 43% | |
| Medical Device Program User Fees | $0.228 | – | 35% | |
| Source: 1 |
This table illustrates the significant financial reliance of the FDA on user fees, particularly within its human drugs program. By demonstrating that nearly half of the FDA’s overall budget and two-thirds of its human drug program budget are derived from industry fees, it underscores the substantial financial interdependence that defines the PDUFA framework. This quantitative data is essential for understanding the structural context of pharmaceutical influence.
B. The Debate: PDUFA as a Conflict of Interest vs. Catalyst for Innovation
PDUFA has sparked a persistent debate regarding its impact on regulatory integrity. Proponents argue that the act has been a transformative force, revolutionizing the U.S. drug approval process. It has enabled the FDA to significantly reduce average drug approval times, from over 31 months before PDUFA to approximately 10 months for standard applications today, without compromising safety standards.22 This acceleration is attributed to PDUFA funding allowing the FDA to hire additional scientific and medical reviewers, modernize its systems, and provide more rapid access to safe and effective new therapies for American patients.23 As a result, the United States has solidified its position as a global leader in the introduction of innovative new medicines, with a high percentage of novel drugs receiving their first approval in the U.S..22 The program also offers biopharmaceutical companies greater regulatory predictability, which fosters industry investment in research and development.22
Despite these benefits, critics contend that PDUFA represents an “unacceptable conflict of interest”.30 The primary concern stems from the FDA’s substantial financial dependence on the very industry it is mandated to regulate. This financial relationship raises questions about potential regulatory capture and whether the agency might be subtly, or overtly, incentivized to prioritize the speed of drug approvals over rigorous scientific scrutiny to maintain its funding stream and meet performance targets.27 The fact that the FDA and drug manufacturers directly negotiate the user fees and the performance measures the FDA must meet to collect them further fuels these concerns, creating a collaborative dynamic that some argue blurs the lines of independent oversight.27 The underlying tension is that while PDUFA was enacted to address a genuine public health need for faster drug access, its funding mechanism inherently creates a financial tie that can be perceived as compromising the agency’s independence. This directly impacts public trust and the perceived integrity of drug approvals.
This situation highlights a fundamental tension in modern regulatory policy: how to adequately fund a critical public health agency to perform its duties efficiently without creating a financial dependence on the very entities it regulates. The debate is not about whether PDUFA causes illegal bribery, but whether it creates a structural incentive for the FDA to be more permissive, or at least less stringent, in its reviews to maintain its funding and meet performance targets that are, in part, negotiated with the industry.
Furthermore, the structure of PDUFA reflects a shifting financial burden. User fees, while collected from pharmaceutical companies, are ultimately “indirectly borne by consumers to the extent that fees are passed through to consumers through increased prices”.1 This means that the FDA has transitioned from being an “entirely taxpayer-funded entity to one increasingly funded by user fees paid by manufacturers”.27 This financial model suggests that while PDUFA aims to benefit public health by accelerating drug approvals, the funding mechanism itself shifts a significant portion of the cost burden from general taxpayers to pharmaceutical companies. These companies, in turn, likely pass these costs onto consumers through higher drug prices, especially given the unique pricing dynamics of the U.S. market.33 This creates a cyclical economic relationship where the industry funds the regulator, and consumers ultimately fund the industry. This economic reality adds another layer to the discussion of influence, as the industry’s financial contribution is not a “gift” but a cost of doing business, which is then recouped from the market, potentially contributing to high drug prices.
C. Proposed Reforms to Mitigate PDUFA-Related Conflicts
Recognizing the concerns about PDUFA’s potential for conflict of interest, various reforms have been proposed to enhance the FDA’s independence and public trust. One suggestion is to implement individualized user fees for each new drug application, rather than flat fees, to better reflect the variable workload associated with assessing diverse and complex clinical data.30 This approach would allow the FDA to directly solicit input from manufacturers regarding the costs and workload of analyzing their specific clinical trials, leading to more appropriate pricing for the services rendered.30
Another key proposal is to assess these additional fees post hoc, meaning after a decision (e.g., grant or denial of approval) has been made.30 This method aims to significantly reduce potential conflicts of interest or perverse incentives, as the fees would be paid purely for services rendered, irrespective of the outcome of the regulatory decision. This could also lead to a more efficient allocation of funding, as manufacturers would only pay for costs directly related to the services received, while still ensuring PDUFA’s revenue stream for the FDA.30
Additionally, some proposals suggest assessing a penalty in addition to the normal user fee for drug applications that demonstrate substandard clinical trial performance.30 This “stick” approach would incentivize higher-quality data submission from manufacturers, discouraging intentionally poor drug applications that consume FDA resources. For drugs approved under compressed timelines due to dire need, a higher-than-normal user fee could be assessed, with the additional revenue used by the FDA to communicate the circumstances of the drug’s approval to patients and physicians, providing an informative due warning.30
Finally, adjusting the user fee structure to reduce incentives for overly permissive drug approvals is a critical area for reform. Currently, a significant portion of PDUFA user fees comes from annual establishment and product fees rather than the initial application examination.30 To counteract potential perverse incentives that could lead the FDA to adopt a more permissive attitude during the drug approval process, it is proposed that the majority of user fees should be collected for the drug application examination process itself, rather than for post-approval activities.30 Even if this means over-collecting for application examination and redistributing these fees for other FDA purposes like overhead or post-market surveillance, the goal is to eliminate any systematic opportunities for the FDA to appear to “profit” from granted approvals. This addresses the core of “agency capture” arguments and aims to reassure critics while sustaining fee revenues from manufacturers.30
V. Lobbying and Political Advocacy: Direct Avenues of Influence
A. The Scale of Pharmaceutical Lobbying
The pharmaceutical and health product industry consistently ranks as one of the most prolific spenders on lobbying activities in the United States, demonstrating its strategic commitment to influencing federal policy. From 1999 to 2018, the industry collectively spent an extraordinary $4.7 billion on lobbying the U.S. federal government, averaging $233 million per year—a figure higher than any other industry during that period.2 This trend of substantial investment continued, reaching a record high of over $373.7 million in 2022 alone.34
These extensive lobbying efforts are driven by major pharmaceutical companies and influential trade associations. Prominent players such as the Pharmaceutical Research and Manufacturers of America (PhRMA), Pfizer, Amgen, Eli Lilly, Merck, Johnson & Johnson, and the Biotechnology Innovation Organization (BIO) consistently appear among the top lobbying spenders.2 For instance, PhRMA alone accounted for $422.3 million in lobbying expenditures between 1999 and 2018, while Pfizer spent $219.2 million.2 In 2022, PhRMA spent $29.2 million, and Pfizer invested over $14.8 million in lobbying, a 34% increase from the previous year.34
Beyond direct lobbying, the industry also makes significant financial contributions to political campaigns. From 1999 to 2018, the pharmaceutical and health product industry contributed $414 million to candidates in presidential and congressional elections, national party committees, and outside spending groups.2 This includes $22 million to presidential candidates and $214 million to congressional candidates, with a notable concentration of contributions to lawmakers on health-related committees.2 This demonstrates a dual approach to influence: direct advocacy through lobbying and indirect influence through campaign finance.
Table 2: Pharmaceutical Industry Federal Lobbying Expenditures (1999-2022)
| Metric | Value (USD) | Source |
| Total Lobbying (1999-2018) | $4.7 billion | 2 |
| Average Annual Lobbying (1999-2018) | $233 million | 2 |
| Total Campaign Contributions (1999-2018) | $414 million | 2 |
| Total Lobbying (2022) | >$373.7 million (record high) | 34 |
| Top Lobbying Spenders (1999-2018) | ||
| PhRMA | $422.3 million | 2 |
| Pfizer | $219.2 million | 2 |
| Amgen | $192.7 million | 2 |
| Eli Lilly and Company | $166.2 million | 2 |
| BIO | $153.4 million | 2 |
| Top Campaign Contributors (1999-2018) | ||
| Pfizer | $23.2 million | 2 |
| Amgen | $14.7 million | 2 |
| Eli Lilly and Company | $13.3 million | 2 |
Source: 2
This table quantifies the immense financial resources the pharmaceutical industry dedicates to influencing federal policy and political campaigns. By presenting the scale of spending over time and identifying the key corporate and trade association players, it provides concrete, empirical evidence of the industry’s commitment to shaping the regulatory and legislative landscape. This directly supports the argument that lobbying is a significant and strategic mechanism of “pharmaceutical influence,” moving beyond anecdotal evidence to demonstrate a pervasive and well-funded effort.
B. Impact on Legislation and Policy Outcomes
The substantial financial investment in lobbying by the pharmaceutical industry is not a charitable act but a calculated business strategy designed to yield measurable returns in terms of favorable regulatory outcomes and market value. This is evident in the industry’s significant impact on legislation and policy.
Lobbying efforts have been instrumental in shaping critical legislation, particularly concerning drug pricing. A prominent example is the Medicare Modernization Act of 2003, where intense lobbying successfully ensured the exclusion of government negotiation for drug prices, a policy that has contributed to higher drug costs in the U.S..35 More recently, the industry aggressively lobbied against the Inflation Reduction Act of 2022 (IRA), which introduced Medicare drug price negotiation. Despite PhRMA spending $29.2 million in 2022 lobbying on this bill, and other major companies like Pfizer increasing their lobbying spending significantly, the IRA was ultimately signed into law.34 While the industry claimed the IRA would harm innovation, studies have since debuked these claims, showing R&D spending actually increased after the law passed.36 This demonstrates that while lobbying can be powerful, it does not always guarantee desired legislative outcomes, but it consistently aims to protect industry profits.
Beyond pricing, lobbying has influenced regulatory pathways. The 21st Century Cures Act (2016), for instance, was influenced by pharmaceutical lobbying efforts and has been criticized for streamlining drug approvals and potentially reducing regulatory hurdles, prioritizing industry interests over patient safety.35 There are also ongoing debates about proposals to change the FDA’s mission to include job creation, which critics argue could reduce the scrutiny applied to medical devices.40
Academic studies provide empirical evidence of a correlation between lobbying activities and drug approval success. Research from 1998 to 2013 found that pharmaceutical firms actively engaged in lobbying had a “67.3 percent higher chance” of getting their new prescription drugs approved by the FDA compared to non-lobbying firms.3 This correlation also extends to financial markets, with lobbying firms experiencing, on average, a 1.1% higher stock market reaction around FDA drug approval announcements than their non-lobbying peers.3 This pattern indicates that lobbying acts as a strategic investment designed to yield measurable returns in terms of favorable regulatory outcomes and market value.
Furthermore, a study analyzing FDA product recalls between 2012 and 2019 suggested that firms engaged in lobbying appeared more likely to receive favorable (i.e., less severe) recall classifications from the FDA. While this finding was more pronounced for food recalls, it indicates a potential for lobbying to influence regulatory enforcement actions beyond initial approvals.41
This pervasive and well-funded lobbying effort serves as a legal, institutionalized mechanism for the pharmaceutical industry to shape the regulatory environment and specific agency decisions in its favor. It achieves outcomes that, in some ways, parallel what one might imagine illegal bribery would achieve, but through policy advocacy, access, and the cultivation of relationships rather than direct illicit payments. This raises fundamental questions about the fairness of the democratic process and whether public health interests are adequately represented against such concentrated financial and political power.
C. Revolving Door and Indirect Lobbying
A significant aspect of pharmaceutical influence is the “revolving door” phenomenon, where individuals transition between government service and industry roles. A substantial number of lobbyists working for pharmaceutical trade groups previously held positions in the federal government. For instance, in 2022, 145 out of 206 lobbyists for PhRMA and 8 out of 11 lobbyists for the Pharmaceutical Care Management Association (PCMA) were former federal employees.34 This movement of personnel provides the industry with invaluable insider knowledge of regulatory processes, internal personnel, and decision-making nuances.
Internal FDA emails, obtained through Freedom of Information Act requests, have revealed a particularly concerning aspect of this phenomenon: FDA ethics staff proactively inform officials leaving for industry jobs about their ability to influence the agency indirectly.5 This includes advice on how to run lobbying campaigns “behind the scenes” without directly contacting their former colleagues.5 This practice has been highlighted as a “critical loophole” in post-employment restrictions, effectively allowing for continued influence peddling and potentially advancing the interests of “big pharma”.5 Peter Lurie, former associate commissioner at the FDA, expressed concern over the perils of allowing such behind-the-scenes work, noting that “this policy likely plays out in a way that advances the interests of big pharma, as that’s where many officials head after FDA”.5
The revolving door transforms abstract lobbying into highly targeted and informed influence. It allows the industry to leverage deep institutional knowledge and personal relationships, potentially giving them an unfair advantage in shaping policy and regulatory outcomes. This mechanism, while also legal, contributes significantly to concerns about “regulatory capture,” where the regulated entity unduly influences the regulator’s agenda and decisions, potentially to the detriment of public interest.
VI. The “Revolving Door”: Personnel Transitions and Enduring Influence
A. Dynamics and Concerns of Post-Government Employment
The movement of personnel between the FDA and the pharmaceutical industry, often termed the “revolving door,” is a frequent occurrence and a persistent source of concern regarding regulatory impartiality and public trust.4 Studies have documented this trend: for example, nearly half of hematology-oncology medical reviewers who left the FDA between 2001 and 2010 (15 out of 26, or 57.7%) subsequently found employment or consulting roles within the biopharmaceutical industry.4 More broadly, it has been observed that almost every former FDA commissioner from the early 1980s through Dr. Scott Gottlieb’s tenure accepted positions in the pharmaceutical industry after leaving the agency.4
This pattern of personnel movement raises serious questions about the impartiality and independence of high-level FDA regulators.4 The prospect of lucrative private-sector employment in a regulated industry can create a “risk of bias” in favor of regulated entities, even if such influence is unconscious.4 This phenomenon is seen as eroding public confidence in agency decision-making, as institutional legitimacy suffers whenever the potential for bias exists.4 The corrosive effects on public perceptions of agency decision-making are noted as resistant to easy solutions, largely because external observers often lack the specialized information and expertise needed to fully assess complex, technical decisions like drug approvals.4 The problem is framed as an “institutional problem” rather than solely a matter of individual ethics, as the very structure of these transitions can foster a bias that is difficult to detect or prove.4
B. Navigating Post-Employment Restrictions and Indirect Influence
While the “revolving door” is a recognized concern, legal and ethical frameworks exist to manage these transitions. The FDA maintains internal ethics policies that prohibit former employees from participating in any regulatory action before the FDA that involves their former employer for a period of one year.43 Additionally, any FDA employee who previously worked at a regulated entity and holds a financial interest in that entity (e.g., from stock options) is prohibited from working on a matter related to that former employer.43 Federal law also sets specific restrictions on post-employment lobbying activities by former government employees, aiming to prevent direct influence peddling.5
However, the effectiveness of these restrictions is a subject of ongoing debate. Internal FDA emails, obtained through Freedom of Information Act requests, have revealed that FDA ethics staff proactively inform departing officials about their ability to influence the agency indirectly. This can include running lobbying campaigns from “behind the scenes,” as long as they do not directly contact their former officials.5 This practice has been highlighted as a “critical loophole” that effectively allows for continued influence peddling and is suspected of advancing the interests of “big pharma”.5 Critics argue that this form of indirect lobbying leverages the former officials’ deep understanding of FDA processes and internal dynamics, providing an inherent advantage to their new industry employers, even if direct contact is avoided.5
Several notable examples illustrate the impact of the revolving door. Jeffrey Siegel, an FDA regulator who oversaw the review of Genentech’s Actemra, later joined Genentech as Global Head of Rheumatology and Rare Diseases.4 Similarly, former FDA Commissioner Dr. Scott Gottlieb joined the Board of Directors of Pfizer within four months of his resignation, a rapid transition that drew pointed criticism.4 More recently, controversies surrounding the FDA’s approvals of Alzheimer’s therapy Aduhelm and Duchenne muscular dystrophy therapy Exondys 51 have also raised concerns about “atypical associations” between FDA regulators and pharmaceutical company sponsors, leading to questions about undue influence.4 In the case of Aduhelm, a House report corroborated “atypical procedures and deviat[ions] from the agency’s own guidance” during its review, leading to multiple federal investigations and resignations from the FDA advisory committee.4
The “revolving door” is thus not merely a series of isolated ethical dilemmas but a systemic, institutionalized feature of the regulatory landscape. The high frequency of transitions and the explicit guidance on “behind-the-scenes” influence suggest that this phenomenon creates a perpetual cycle of potential influence. Even if former officials scrupulously avoid direct violations of post-employment rules, their deep understanding of FDA processes, internal personnel, and regulatory priorities, combined with their new industry roles, provides an inherent and significant advantage to their new employers. This challenges the fundamental perception of an independent regulatory body and can lead to a subtle form of “regulatory capture,” where the agency’s long-term interests might align too closely with the industry it is mandated to regulate.
The most insidious aspect of the revolving door is its capacity to foster unconscious bias. The dangers are understood as a “product of conscious and unconscious influence,” and it is recognized that “biased decision-making is often the result of unconscious processes”.4 This means that even without direct quid pro quo, the anticipation of future employment or the natural alignment of interests cultivated over time can subtly steer regulatory decisions. This makes the influence harder to detect and prove, yet its cumulative effect on regulatory outcomes can be significant. The resulting erosion of public trust is a critical consequence, regardless of whether actual, provable bias is demonstrated, because it undermines the credibility and perceived fairness of the FDA’s vital public health decisions.
VII. FDA Advisory Committees: Expertise, Transparency, and Influence
A. Role and Composition of Advisory Committees
FDA advisory committees serve a vital function in the agency’s mission, providing independent expert advice on complex scientific, technical, and policy matters.44 These committees are particularly crucial when the FDA faces internal disagreements, ambiguous scientific evidence, or requires external validation for a potential decision.45 Their primary purpose is to help the FDA make sound decisions based on rigorous scientific principles and to enhance transparency in the regulatory process.44 The Federal Advisory Committee Act (FACA) outlines their activities and operations, emphasizing their advisory role; while they provide recommendations, the FDA retains final decision-making authority.44
The composition of these committees is designed to bring diverse perspectives to the table. Members typically include scientific experts such as physician-researchers, statisticians, engineers, chemists, and biologists, who possess specialized knowledge relevant to the committee’s function.44 In addition to scientific experts, committees include consumer representatives, who voice the consumer perspective, and patient representatives, who provide input from the patient’s viewpoint.44 Crucially, FDA advisory committees also include non-voting industry representatives.44 These individuals act on behalf of the regulated industry’s general perspective, rather than a specific firm, and are explicitly prohibited from voting or attending closed sessions.47 Their role is to provide industry insights and engage in discussions, contributing to a more comprehensive understanding of the issues.47
B. Managing Financial Conflicts and Perceived Bias
The presence of individuals with potential financial ties to the pharmaceutical industry on advisory committees has long been a source of public and congressional concern.50 A conflict of interest for an advisory committee member arises when their financial interests could be impacted by their work on the committee.16 Federal law (18 U.S.C. 208(a)) strictly prohibits federal employees and SGEs from participating in matters that would have a “direct and predictable effect” on their financial interests.16
The FDA employs a rigorous vetting process, requiring SGEs to submit Confidential Financial Disclosure Reports (FDA Form 3410) to identify potential conflicts.16 While the agency aims to exclude individuals with substantial conflicts, waivers can be granted under 18 U.S.C. 208(b)(2) if the financial interest is deemed “too remote or too inconsequential” to affect integrity, or if the individual’s unique scientific expertise is critical and outweighs the potential for conflict.16 However, the granting of such waivers has drawn significant scrutiny, with a widely cited study finding that 73% of advisory meetings involved at least one member with a conflict of interest.50 Critics argue that granting waivers to experts with financial ties can undermine the objectivity of committee recommendations and public trust.50
In response to persistent concerns about perceived industry influence, FDA Commissioner Martin A. Makary recently announced a new policy directive. This policy limits individuals employed at FDA-regulated companies, such as pharmaceutical firms, from serving as official voting members on FDA advisory committees, where statutorily allowed.51 While industry employees are still permitted to attend meetings and present their views, this measure aims to avoid the appearance of a “cozy relationship” and restore “impeccable integrity” to the process, especially given low public trust in the healthcare-industrial complex.51 This policy change reflects an acknowledgment of these concerns and an attempt to bolster public trust.
C. Influence of Presentations and Public Testimony
The format of FDA advisory committee meetings provides avenues for various stakeholders to present their perspectives, which can influence committee deliberations. Sponsoring companies strategically design their presentations to persuade committee members to recommend approval for their products.52 This involves a deep understanding of the audience’s thinking, priorities, and potential biases, with a focus on presenting key data points related to efficacy and safety in a compelling manner.52 To ensure a balanced presentation, equal time is generally allotted for both the sponsor’s and the FDA’s presentations, allowing the committee to hear “both sides” of the scientific and regulatory arguments.47
Advisory committee meetings also include an open public hearing segment, where members of the public can provide testimonies.44 While speakers are asked, but not legally required, to disclose any conflicts of interest before speaking, this voluntary disclosure can be problematic.53 A study investigating public speakers at Psychopharmacologic Drugs Advisory Committee (PDAC) meetings found that speakers who disclosed a conflict of interest were associated with increased odds of providing a favorable testimony for the psychiatric drug in question.53 This finding raises concerns that undisclosed or acknowledged conflicts of interest could “skew public speaker’s testimonies and persuade committee members through emotionally charged tactics,” potentially impacting the scientific objectivity of the discussion.53
Despite these influences, it is important to reiterate that advisory committee recommendations are strictly advisory in nature; the FDA makes the final decisions on all matters.44 While there have been controversial instances where the FDA’s final regulatory decisions have deviated from advisory committee recommendations (e.g., the approval of Aduhelm despite committee objections 4), such instances are in the minority, with agency decisions largely aligning with committee advice.45 However, the presence of industry representatives (even non-voting ones) and the persuasive nature of sponsor presentations, combined with the potential for biased public testimonies, contribute to a perception of influence that the FDA is actively trying to mitigate through policy changes like the one limiting voting industry members.
VIII. Industry-Sponsored Research and Data Integrity
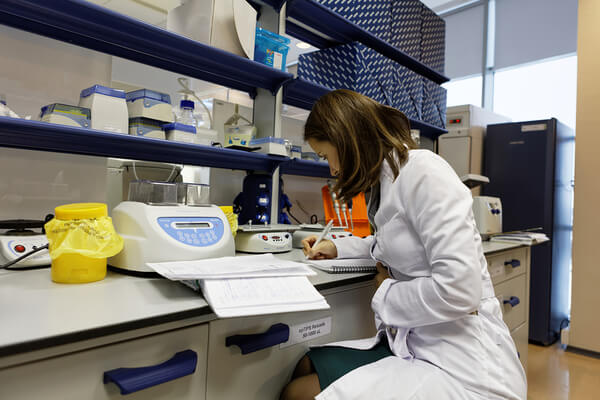
A. Prevalence and Influence of Industry Funding
The vast majority of clinical trials conducted to support regulatory approval of drugs, devices, or vaccines are sponsored by manufacturers.6 Former FDA Commissioner Robert Califf estimated that approximately 70% of all clinical trials in the United States are industry-funded.6 While industry funding is crucial for advancing medical progress, especially given the substantial costs of clinical trials (e.g., new respiratory medicines average about $115.3 million per trial) 7, it also introduces significant concerns about potential bias and the integrity of research findings.
Studies have consistently shown that industry-sponsored trials are more likely to yield positive results than government-sponsored trials.6 This raises questions about whether financial interests influence research outcomes. Critics suggest that pharmaceutical companies may selectively fund trials on drugs they believe are superior, or that positive results could stem from poor-quality research.54 There is also concern that industry influence could lead drug companies to focus on the benefits of a drug while downplaying its risks for the sake of profit, potentially leading to biased information that influences prescribing practices.7
B. Impact on Clinical Trial Design and Reporting
The influence of industry funding extends to the very design and reporting of clinical trials. Pharmaceutical companies, driven by the motivation for “big profits,” may design studies and report results “in a manner that is biased toward showing a favorable risk-benefit profile”.7 This can manifest in several ways:
- Selective Funding and Dosing: Companies may selectively fund trials on drugs they expect to perform well or use non-equivalent doses, often giving the study drug at a higher dose than a comparator, potentially biasing results in their favor.54
- Researcher Alignment: Clinical trials are often run, designed, and analyzed by researchers on the drug company’s payroll. Some principal investigators (PIs) in such roles have reported viewing themselves more as businessmen than researchers, aligning their ethics with industry goals.7
- Data Manipulation and Suppression: There are allegations of companies falsifying questionnaire answers, omitting side effects in reports to the FDA (e.g., Essure Permanent Birth Control case).7 A significant problem is “publication bias,” where studies with negative or unfavorable results are rarely published, creating a body of evidence that does not reflect the true risk-benefit profile of a medicine.7 Companies have also been accused of attempting to block the publication of articles showing their products were no better than placebo.54
- Ghostwriting and Marketing as Science: Postmarketing trials are sometimes initiated primarily to create familiarity with a product rather than to determine scientific outcomes, effectively using “marketing wearing the mask of science”.54 Evidence suggests that participation in such trials shapes physicians’ prescribing habits by increasing their familiarity with the drug.54 Furthermore, pharmaceutical companies may write up and analyze data collected by academic researchers, paying them to present it, a practice seen as an attempt to circumvent publication guidelines and promote a product.56
The reliance on industry-funded and conducted research for drug approval creates an inherent conflict, as the entity with a direct financial stake is also the primary generator of the evidence used for regulatory decisions. This situation necessitates robust FDA oversight to ensure the integrity and reliability of the data.
C. FDA Scrutiny and Safeguards
The FDA recognizes the importance of data integrity and implements various mechanisms to scrutinize industry-generated clinical trial data and mitigate bias. Its oversight spans the full trial lifecycle, from investigational new drug (IND) applications to post-market surveillance.57
- Pre-Trial Phase: Before a clinical trial begins, sponsors must submit INDs (for drugs/biologics) or Investigational Device Exemptions (IDEs) for devices, detailing the trial protocol, manufacturing processes, and preclinical findings. The FDA reviews these submissions, focusing on patient safety, scientific integrity, and data reliability. The agency may require protocol adjustments to improve statistical rigor, define patient eligibility, or revise monitoring practices to reduce bias and ensure data acceptability for approval decisions.57 FDA guidance documents serve as blueprints for trial design, and aligning protocols with these expectations minimizes the risk of clinical holds or rejections.57
- Trial Conduct and Monitoring: During the trial, the FDA enforces strict requirements for data monitoring, adverse event reporting, and informed consent. Investigators must maintain detailed records and adhere to Good Clinical Practice (GCP) standards.57 FDA inspections at clinical study sites focus on identifying deviations from protocol, falsification of records, or lapses in safety monitoring.57 The Bioresearch Monitoring Program, established in the late 1970s, aims to detect misconduct and ensure data integrity.58 Institutional Review Boards (IRBs) also play a crucial role in protecting human subjects’ rights and welfare, with the FDA conducting nearly 200 IRB inspections annually.58
- Post-Market Surveillance: Approval is not the end of regulatory oversight. The FDA continues to monitor drug safety through post-market surveillance programs like MedWatch for adverse events and may require Phase IV (post-marketing) studies.57 The agency can issue label changes, require additional warnings, or mandate recalls if significant safety concerns emerge.57 The FDA is increasingly leveraging real-world data (RWD) and real-world evidence (RWE) from sources like electronic health records and claims databases to supplement traditional trials and enhance post-market safety monitoring.61
Despite these safeguards, concerns persist about the FDA’s reliance on industry-generated clinical data. Critics argue that the accelerated approval pathways, while beneficial for urgent needs, may lead to drugs entering the market with less information about their risks and benefits.62 Some studies suggest that drugs approved under expedited programs can later be found to have dangerous side effects or be less effective than initially believed.62 There are also criticisms regarding the inconsistency and underdevelopment of robust, real-time post-market monitoring mechanisms for certain technologies, like AI-enabled medical devices, which can lead to performance degradation and biased outcomes not anticipated during pre-market evaluations.64
Given the inherent limitations of pre-market trials, which involve controlled populations and durations, effective post-market surveillance is crucial for identifying rare or long-term adverse events that only become apparent with broader real-world use. This ongoing monitoring serves as a critical backstop to ensure drug safety and efficacy throughout a product’s lifecycle.
IX. Public Health and Economic Consequences of Influence
The various forms of pharmaceutical influence on the FDA and the broader regulatory landscape have significant public health and economic consequences, shaping drug development, pricing, and safety outcomes.
A. Impact on Drug Prioritization and Innovation
Pharmaceutical influence can subtly, or overtly, impact which therapeutic areas and types of drugs are prioritized for development and expedited review. Lobbying and financial incentives can steer research and development (R&D) towards areas that promise higher returns, potentially at the expense of public health needs for less profitable conditions.55
The FDA’s Commissioner’s National Priority Voucher (CNPV) program, a pilot initiative designed to accelerate the review of drugs serving U.S. national interests, exemplifies this tension. While intended to speed urgently needed drugs to market, critics express concerns that its “amorphous” criteria for prioritization could lead to “rent-seeking, lobbying, corruption, and excessive bureaucratic discretion” in drug value assessments.67 This system, which allows companies to shorten drug review times from 10-12 months to just one or two months, introduces potential for political interests to overshadow patient needs in research prioritization.67 While Operation Warp Speed during the COVID-19 pandemic demonstrated the FDA’s capacity for rapid review when highly prioritized, the CNPV’s non-transferable nature and broad applicability across a company’s pipeline introduce an “unnecessary arbitrariness” that could further incentivize lobbying for these expedited pathways.68
B. Drug Pricing and Access
Perhaps one of the most direct and widely felt economic consequences of pharmaceutical influence is its impact on drug pricing and patient access. Intellectual property (IP) rights, primarily patents, play a crucial role in enabling pharmaceutical companies to charge higher-than-competitive prices for their products.33 Patents grant exclusive rights to manufacture and sell a drug for typically 20 years, allowing companies to recoup substantial R&D costs.69
However, critics argue that pharmaceutical companies engage in “patenting practices that unduly extend the period of exclusivity,” contributing to high drug prices without significant benefits for consumers or innovation.69 These strategies, often termed “evergreening,” involve filing numerous secondary patents on existing drugs—such as new formulations, delivery methods, or methods of use—long after the primary patent has been granted or even after FDA approval.71 For instance, 66% of patent applications for top-selling drugs in 2021 were filed
after FDA approval.73 This creates “patent thickets”—dense webs of overlapping patents—that deter generic and biosimilar competition due to the high costs and risks of patent litigation.69 Examples like AbbVie’s Humira, which had over 250 patents extending its U.S. exclusivity to 39 years, illustrate how these strategies can delay affordable alternatives for decades.73
The pharmaceutical industry’s lobbying efforts directly impact drug pricing legislation. The industry has historically thwarted attempts at government negotiation of drug prices, arguing that such measures would stifle R&D.37 While the Inflation Reduction Act of 2022 (IRA) finally allowed Medicare to negotiate some drug prices, the industry spent massive sums lobbying against it.34 Despite industry claims, studies indicate the IRA’s impact on drug development risk is minimal, saving billions for the federal government and Medicare patients.36 This demonstrates the ongoing battle over drug pricing, where industry influence seeks to maintain high profit margins, often leading to prohibitively expensive medications for patients.33 The tension between incentivizing innovation through market exclusivity and ensuring affordable access to essential medicines is a central policy challenge, often exacerbated by industry influence.
C. Drug Safety and Public Trust
The cumulative effect of pharmaceutical influence mechanisms, particularly when linked to drug safety controversies or high prices, can significantly erode public trust in both the pharmaceutical industry and the FDA. Historical tragedies, such as the thalidomide crisis in the 1960s (causing severe birth defects) and the sulfanilamide poisoning in 1938, underscore the critical importance of rigorous drug safety regulation.10
However, concerns persist that industry influence can compromise drug safety. Critics allege that the FDA has sometimes overlooked safety concerns due to industry pressure or has been slow to withdraw unsafe drugs from the market.79 Notable examples include:
- Vioxx (Rofecoxib): This painkiller, approved by the FDA despite a senior medical officer noting a threefold increase in cardiovascular problems, was later linked to up to 140,000 heart attacks and strokes before its voluntary withdrawal by Merck in 2004.63 Reports suggested both Merck and the FDA ignored evidence of dangerous side effects for years.77
- Opioid Crisis: The FDA has been criticized for regulatory mistakes in approving and labeling new analgesics, contributing to the opioid crisis. The agency failed to properly enforce the FDCA when it approved Purdue Pharma’s extended-release oxycodone with a broad indication in 1995, despite drug makers being prohibited from promoting off-label uses without premarket review.82 The President’s Commission on Combatting Drug Addiction and the Opioid Crisis found “inadequate oversight by the Food and Drug Administration” as a contributing factor.82
- Aduhelm (Aducamumab) and Exondys 51 (Eteplirsen): Recent controversies surrounding the FDA’s approval of these drugs, despite fierce internal disputes and advisory committee objections, raised questions about undue influence and “atypical associations” between FDA regulators and pharmaceutical sponsors.4 Aduhelm’s approval, in particular, was scrutinized for “atypical procedures and deviat[ions] from the agency’s own guidance,” leading to multiple federal investigations.4 Exondys 51, approved under accelerated pathways, has yet to complete confirmatory trials six years later, and its high price (approx. $1 million/year) despite unproven effectiveness further fuels concerns.4
Beyond specific drug approvals, industry marketing practices can lead to less evidence-based prescribing and higher medication costs.55 Pharmaceutical companies spend vast sums on marketing—sometimes twice as much as on R&D—to influence doctor’s prescribing decisions, even through seemingly inconsequential gifts or “educational” materials that may exaggerate benefits and minimize risks.55 This can result in physicians being “under the influence” of drug companies, leading to inappropriate prescribing.86
The cumulative effect of these influence mechanisms, particularly when linked to drug safety controversies or high prices, can significantly erode public trust in both the pharmaceutical industry and the FDA. When patients perceive that profit motives override public health considerations, the credibility of the entire drug approval and regulatory system is undermined.
X. Safeguards and Future Directions
A. Existing Safeguards and Oversight Mechanisms
The FDA and the broader federal government employ a multi-layered system of safeguards and oversight mechanisms to counter undue pharmaceutical influence and maintain regulatory integrity:
- Internal FDA Mechanisms:
- Ethics Office: The FDA’s Office of Ethics and Integrity (OEI) provides mandatory ethics training, counsels employees on conflict of interest rules, and reviews financial disclosure forms annually to prevent and mitigate conflicts.14 Employees are required to seek approval for outside activities that could pose conflicts.87
- Scientific Integrity Policies: The FDA has policies to promote scientific integrity, ensuring that decisions are based on rigorous scientific research free from political suppression or distortion.88 The Office of Scientific Integrity (OSI) leads the development of agency-wide policies, coordinates dispute resolution, and investigates allegations of research misconduct.59
- Internal Audits and Data Integrity: The FDA expects regulated companies to conduct regular internal audits to monitor compliance with regulatory standards and identify issues before FDA inspections.91 The agency also scrutinizes clinical trial data submitted by industry, conducting its own audits and inspections to verify accuracy and ensure compliance with Good Clinical Practice (GCP) standards.58 The Bioresearch Monitoring Program and Institutional Review Boards (IRBs) are key to protecting human subjects and data integrity.58 The FDA has also taken action against firms submitting falsified or unreliable testing data.92
- External Oversight:
- Congressional Oversight: Congress plays a critical role in overseeing the FDA, including reauthorizing user fee programs and scrutinizing agency decisions and policies.23
- Government Accountability Office (GAO) & OIG: The GAO and the HHS Office of Inspector General (OIG) conduct investigations into FDA operations and industry practices, identifying areas of concern and recommending reforms.4
- Whistleblower Protections: Federal laws, such as the Whistleblower Protection Act (WPA) and provisions within the FDA Food Safety Modernization Act (FSMA), protect federal employees and employees of regulated entities from retaliation for reporting violations, fraud, waste, abuse, or dangers to public health.93 The False Claims Act’s “qui tam” provisions also incentivize insiders to expose fraud, leading to significant recoveries.21
- Transparency Measures: The Physician Payments Sunshine Act (Open Payments) mandates public disclosure of financial relationships between pharmaceutical companies and healthcare providers, increasing transparency and allowing public scrutiny of potential conflicts of interest.18
- Appeals Process: The FDA provides formal dispute resolution mechanisms for sponsors and applicants to appeal agency decisions that cannot be resolved at lower levels, ensuring a pathway for review of scientific or medical disagreements.98
B. Calls for Reform and Enhanced Scrutiny
Despite existing safeguards, the dynamic nature of industry influence necessitates continuous vigilance, adaptation of policies, and robust enforcement to protect public health. Calls for reform and enhanced scrutiny are ongoing:
- PDUFA Reform: Proposals aim to mitigate the conflict of interest inherent in PDUFA funding, suggesting individualized user fees, post-hoc fee assessment (after approval decisions), and penalties for substandard clinical trial data.30 Rebalancing the fee structure to focus more on the application examination process rather than post-approval activities is also proposed to counter arguments of “agency capture”.30
- Advisory Committee Integrity: The FDA has already taken steps to limit industry employees from serving as official voting members on advisory committees, a move aimed at enhancing public trust and perceived independence.51 Further reforms could involve stricter conflict of interest rules for all members, including those with indirect financial ties to competing firms.45
- Clinical Trial Data Transparency and Independence: There are ongoing calls for greater transparency in industry-funded clinical trials, including mandatory publication of all trial results (positive and negative) to combat publication bias.7 Enhanced scrutiny of trial design, especially concerning potential biases in methodology (e.g., non-equivalent dosing, functional unblinding), is crucial.54 Greater investment in independent, publicly funded research could also provide a counterbalance to industry-sponsored studies.6
- Post-Market Surveillance Strengthening: Given that many serious side effects are detected only after drugs are on the market, strengthening post-market surveillance is vital.24 This includes robust, real-time monitoring mechanisms and standardized post-market evaluation practices, particularly for new technologies like AI-enabled devices where current oversight may be inconsistent.64
- Addressing the “Revolving Door”: While post-employment restrictions exist, the “critical loophole” of “behind-the-scenes” lobbying by former officials remains a concern.5 Legislative proposals to further restrict former health sector employees from joining industry boards after public service have been introduced, though none have passed.5
These ongoing efforts reflect a recognition that while direct bribery of FDA officials is illegal and rare, the complex interplay of financial ties, lobbying, personnel movement, and industry-funded research creates a pervasive environment where influence can subtly, yet profoundly, shape regulatory outcomes. Continuous adaptation of policies and robust enforcement are essential to ensure the FDA’s core mission of public health protection remains paramount.
XI. Conclusion
The question of whether drug companies can bribe the FDA is met with a clear legal answer: direct bribery of federal officials is illegal and carries severe penalties under U.S. law. The FDA, supported by federal statutes and its own ethics policies, maintains a strict stance against such overt corruption, implementing training, financial disclosures, and oversight to prevent conflicts of interest.
However, the comprehensive analysis reveals that the pharmaceutical industry exerts significant and multifaceted influence through legal and quasi-legal channels. This influence is not a matter of explicit, illegal bribery but rather a systemic reality woven into the fabric of the regulatory ecosystem. Key mechanisms include:
- Financial Interdependence (PDUFA): User fees, while vital for the FDA’s operational efficiency and accelerated drug approvals, create a substantial financial reliance on the regulated industry. This structural relationship, where the FDA’s budget is significantly funded by industry fees, raises legitimate concerns about potential regulatory capture and the perception of compromised independence.
- Lobbying and Political Advocacy: The pharmaceutical industry’s massive financial investment in lobbying and campaign contributions directly shapes legislation and regulatory policies. This strategic investment correlates with favorable drug approval outcomes and has demonstrably influenced critical policy decisions, such as drug pricing regulations.
- The “Revolving Door”: The frequent transition of former FDA officials into lucrative positions within the pharmaceutical industry, coupled with the legality of “behind-the-scenes” influence, creates a persistent risk of bias and erodes public trust in the impartiality of regulatory decisions.
- Industry-Sponsored Research: The pervasive reliance on industry-funded and conducted clinical trials for drug approval introduces inherent biases in data generation, analysis, and reporting. This necessitates rigorous FDA scrutiny and robust post-market surveillance to detect and address potential safety issues that may not be apparent during initial approvals.
The interplay of these mechanisms creates a complex dynamic where the pursuit of innovation and timely drug access must be carefully balanced against the imperative of public health protection and maintaining regulatory integrity. The tension between incentivizing pharmaceutical innovation through market exclusivity and ensuring affordable access to essential medicines remains a central policy challenge, often exacerbated by the industry’s powerful influence.
Ultimately, the truth behind pharmaceutical influence on the FDA lies in this intricate web of legal interactions that, while not constituting illegal bribery, can still lead to outcomes that raise profound ethical questions and impact public health and economic well-being. The cumulative effect of these influences, particularly when linked to drug safety controversies or high drug prices, can significantly erode public trust in both the pharmaceutical industry and the FDA. Therefore, continuous vigilance, adaptive policy reforms that address structural vulnerabilities, and enhanced transparency are essential to ensure that the FDA’s primary mission—to protect and advance public health—remains uncompromised.
Works cited
- FDA-User-Fee-Issue-Brief.pdf – HHS ASPE – HHS.gov, accessed July 23, 2025, https://aspe.hhs.gov/sites/default/files/documents/e4a7910607c0dd76c40aa61151d154f9/FDA-User-Fee-Issue-Brief.pdf
- Lobbying Expenditures and Campaign Contributions by the Pharmaceutical and Health Product Industry in the United States, 1999-2018 – PMC, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7054854/
- Two Faces of Corporate Lobbying: Evidence from the Pharmaceutical Industry – Merrimack ScholarWorks, accessed July 23, 2025, https://scholarworks.merrimack.edu/cgi/viewcontent.cgi?article=1003&context=fin_facpub
- FDA’S REVOLVING DOOR: RECKONING AND REFORM – Stanford Law School, accessed July 23, 2025, https://law.stanford.edu/wp-content/uploads/2023/03/SLPR_Karas.pdf
- FDA staff leaving for industry jobs given “behind the scenes” lobbying advice – BMJ Group, accessed July 23, 2025, https://bmjgroup.com/fda-staff-leaving-for-industry-jobs-given-behind-the-scenes-lobbying-advice/
- The Price of Knowledge: Industry-Sponsored Studies in the Era of Evidence-Based Medicine | tctmd.com, accessed July 23, 2025, https://www.tctmd.com/news/price-knowledge-industry-sponsored-studies-era-evidence-based-medicine
- Big Pharma & Clinical Trials – Funding, Influence & Corruption – Drugwatch.com, accessed July 23, 2025, https://www.drugwatch.com/featured/clinical-trials-and-hidden-data/
- 2041. Bribery Of Public Officials | United States Department of Justice, accessed July 23, 2025, https://www.justice.gov/archives/jm/criminal-resource-manual-2041-bribery-public-officials
- 18 U.S. Code § 201 – Bribery of public officials and witnesses – Law.Cornell.Edu, accessed July 23, 2025, https://www.law.cornell.edu/uscode/text/18/201
- Food, Drug, and Cosmetic Act – StatPearls – NCBI Bookshelf, accessed July 23, 2025, https://www.ncbi.nlm.nih.gov/books/NBK585046/
- The Public Health Role of Drug Regulation in the US | FDA, accessed July 23, 2025, https://www.fda.gov/files/about%20fda/published/The-Public-Health-Role-of-Drug-Regulation-in-the-US.pdf
- Food, Drug, and Cosmetic Act – PubMed, accessed July 23, 2025, https://pubmed.ncbi.nlm.nih.gov/36251824/
- The Scientist’s Guide to Understanding FDA Drug Approval – Excedr, accessed July 23, 2025, https://www.excedr.com/blog/fda-drug-approval-process-guide
- Office of Ethics and Integrity – FDA, accessed July 23, 2025, https://www.fda.gov/about-fda/office-operations/office-ethics-and-integrity
- Code of Ethics – Food and Drug Administration Alumni Association, accessed July 23, 2025, https://www.fdaaa.org/about-fdaaa/code-of-ethics/
- FDA Advisory Committees: Financial Conflicts of Interest Overview, accessed July 23, 2025, https://www.fda.gov/media/87421/download
- Public Availability of Advisory Committee Members’ Financial Interest Information and Waivers | FDA, accessed July 23, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/public-availability-advisory-committee-members-financial-interest-information-and-waivers
- What is the Physician Payments Sunshine Act? – The HIPAA Journal, accessed July 23, 2025, https://www.hipaajournal.com/physician-payments-sunshine-act/
- Physician financial transparency reports (Sunshine Act) – American Medical Association, accessed July 23, 2025, https://www.ama-assn.org/practice-management/medicare-medicaid/physician-financial-transparency-reports-sunshine-act
- FDA Debarment List (Drug Product Applications), accessed July 23, 2025, https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/compliance-actions-and-activities/fda-debarment-list-drug-product-applications
- Pharmaceutical Marketing Regulations: A Comprehensive Overview …, accessed July 23, 2025, https://intuitionlabs.ai/articles/pharmaceutical-marketing-regulations-compliance-fda-ftc-sunshine-act
- PDUFA – PhRMA, accessed July 23, 2025, https://phrma.org/policy-issues/research-development/pdufa
- Preserving PDUFA Is Critical for U.S. Biopharmaceutical Innovation | ITIF, accessed July 23, 2025, https://itif.org/publications/2025/07/01/preserving-pdufa-is-critical-for-us-biopharmaceutical-innovation/
- Politics, Profits & Pharma | Dangerous Prescription | FRONTLINE – PBS, accessed July 23, 2025, https://www.pbs.org/wgbh/pages/frontline/shows/prescription/politics/
- PDUFA Lays the Foundation: Launching Into the Era of User Fee Acts | FDA, accessed July 23, 2025, https://www.fda.gov/files/about%20fda/published/PDUFA-Lays-the-Foundation–Launching-Into-the-Era-of-User-Fee-Acts.pdf
- Prescription Drug User Fee Act – Wikipedia, accessed July 23, 2025, https://en.wikipedia.org/wiki/Prescription_Drug_User_Fee_Act
- Why is the FDA Funded in Part by the Companies It Regulates? – UConn Today, accessed July 23, 2025, https://today.uconn.edu/2021/05/why-is-the-fda-funded-in-part-by-the-companies-it-regulates-2/
- It’s UFA Time Again: Reauthorization of the FDA User Fee Acts Takes Center Stage in Congress – Akin Gump, accessed July 23, 2025, https://www.akingump.com/en/insights/alerts/its-ufa-time-again-reauthorization-of-the-fda-user-fee-acts-takes-center-stage-in-congress
- Prescription Drug User Fee Act Reauthorization – Senate Committee on Health, Education, Labor and Pensions, accessed July 23, 2025, https://www.help.senate.gov/download/testimony/woodcocktestimony34
- “A Legal Challenge of the Prescription Drug User Fee Act” by Jimmy …, accessed July 23, 2025, https://engagedscholarship.csuohio.edu/jlh/vol29/iss1/7/
- A Legal Challenge of the Prescription Drug User Fee Act – PubMed, accessed July 23, 2025, https://pubmed.ncbi.nlm.nih.gov/30866592/
- Regulating Drugs for Effectiveness and Safety: A Public Health Perspective, accessed July 23, 2025, https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/18/09/17/regulating-drugs-for-effectiveness-and-safety-a-public-health-perspective
- Ethical Drug Pricing – The Hastings Center for Bioethics, accessed July 23, 2025, https://www.thehastingscenter.org/briefingbook/ethical-drug-pricing/
- Pharma Spent Record Amount on Lobbying in 2022; PBMs Are Now in Spotli – AIS Health, accessed July 23, 2025, https://aishealth.mmitnetwork.com/blogs/spotlight-on-market-access/pharma-spent-record-amount-on-lobbying-in-2022-pbms-are-now-in-spotlight
- The Influence of Big Pharma on Healthcare Policies in America: Unraveling the Complex Web, accessed July 23, 2025, https://www.pharmafocusamerica.com/articles/the-influence-of-big-pharma-on-healthcare-policies-in-america-unraveling-the-complex-web
- Study Debunks Pharmaceutical Industry’s Claims That Medicare Drug Price Negotiation Would Harm R&D – Retired Americans, accessed July 23, 2025, https://retiredamericans.org/study-debunks-pharmaceutical-industrys-claims-that-medicare-drug-price-negotiation-would-harm-rd/
- Medicare Drug Price Negotiation Is Having a Minimal Impact on Pharma R&D – FREOPP, accessed July 23, 2025, https://freopp.org/whitepapers/results-from-the-first-round-of-medicare-drug-price-negotiation/
- New Reports Show Massive Big Pharma Influence-Peddling to Stop President Biden’s Medicare Drug Price Negotiation – Accountable US, accessed July 23, 2025, https://accountable.us/new-reports-show-massive-big-pharma-influence-peddling-to-stop-president-bidens-medicare-drug-price-negotiation/
- 21st Century Citizen Pharma: The FDA & Patient-Focused Product Development – American University, accessed July 23, 2025, https://www.american.edu/wcl/impact/initiatives-programs/health/events/fdaconf18/conference-papers/upload/paradise.pdf
- Drug and Medical Device Companies Have Outsized Influence on FDA, accessed July 23, 2025, https://www.ucs.org/resources/drug-and-medical-device-companies-have-outsized-influence-fda
- The effects of lobbying on the FDA’s recall classification – PubMed, accessed July 23, 2025, https://pubmed.ncbi.nlm.nih.gov/37340417/
- FDA’s Revolving Door: Reckoning and Reform – Journal Article – Stanford Law School, accessed July 23, 2025, https://law.stanford.edu/publications/fdas-revolving-door-reckoning-and-reform/
- Gauging the Likelihood of Trump Administration FDA Reforms | Insights – Skadden, accessed July 23, 2025, https://www.skadden.com/insights/publications/2025/01/gauging-the-likelihood-of-trump-administration-fda-reforms
- Learn About FDA Advisory Committees, accessed July 23, 2025, https://www.fda.gov/patients/learn-about-fda-advisory-committees
- The Future Of FDA Advisory Committees: Protecting Public Health And Preserving Public Trust | Health Affairs Forefront, accessed July 23, 2025, https://www.healthaffairs.org/do/10.1377/forefront.20240628.510062/
- Advisory Committees – FDA, accessed July 23, 2025, https://www.fda.gov/advisory-committees
- CBER Advisory Committees – FDA, accessed July 23, 2025, https://www.fda.gov/media/133832/download
- Advisory Committee Membership Types – FDA, accessed July 23, 2025, https://www.fda.gov/advisory-committees/advisory-committee-membership/advisory-committee-membership-types
- 21 CFR Part 14 Subpart E — Members of Advisory Committees – eCFR, accessed July 23, 2025, https://www.ecfr.gov/current/title-21/chapter-I/subchapter-A/part-14/subpart-E
- NBER WORKING PAPER SERIES WHAT’S THE “INTEREST” IN FDA DRUG ADVISORY COMMITTEE CONFLICTS OF INTEREST? Joseph Golec Joh, accessed July 23, 2025, https://www.nber.org/system/files/working_papers/w14932/w14932.pdf
- FDA Commissioner Makary Announces New Policy on Individuals Serving on FDA Advisory Committees, accessed July 23, 2025, https://www.fda.gov/news-events/press-announcements/fda-commissioner-makary-announces-new-policy-individuals-serving-fda-advisory-committees
- Five Steps to Writing an Effective Presentation for an FDA Advisory Committee Meeting, accessed July 23, 2025, https://3dcommunications.us/latest-thinking/posts/five-steps-to-writing-an-effective-presentation-for-an-fda-advisory-committee-meeting/
- Characteristics and conflicts of interests of public speakers at the Psychopharmacologic Drug and Advisory Committee meetings regarding psychiatric drugs – PubMed, accessed July 23, 2025, https://pubmed.ncbi.nlm.nih.gov/32019896/
- Pitfalls and Safeguards in Industry-Funded Research – PMC – PubMed Central, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7122252/
- The Influence of the Pharmaceutical Industry – Parliament UK, accessed July 23, 2025, https://publications.parliament.uk/pa/cm200405/cmselect/cmhealth/42/42.pdf
- Does industry funding deserve a bad rap? – American Psychological Association, accessed July 23, 2025, https://www.apa.org/monitor/julaug03/industry
- FDA’s Role in Clinical Trials – Acenth, accessed July 23, 2025, https://acenth.com/blog/the-fdas-influence-on-clinical-trial-design-approval-and-oversight/
- FDA Regulatory Review – Assuring Data Quality and Validity in Clinical Trials for Regulatory Decision Making – NCBI, accessed July 23, 2025, https://www.ncbi.nlm.nih.gov/books/NBK224583/
- Office of Scientific Investigations – FDA, accessed July 23, 2025, https://www.fda.gov/about-fda/cder-offices-and-divisions/office-scientific-investigations
- Institutional Review Boards Frequently Asked Questions – FDA, accessed July 23, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions
- Real-World Evidence – FDA, accessed July 23, 2025, https://www.fda.gov/science-research/science-and-research-special-topics/real-world-evidence
- FDA Is Not the Problem – Center for American Progress, accessed July 23, 2025, https://www.americanprogress.org/article/fda-is-not-the-problem/
- The hazards of rapid approval of new drugs – PMC, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4816872/
- The illusion of safety: A report to the FDA on AI healthcare product approvals – PMC, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12140231/
- FDA Shares New Priorities and ‘Proactive’ Approach to Working with Developers – Cure, accessed July 23, 2025, https://wewillcure.com/insights/therapeutics/fda-shares-new-priorities-and-proactive-approach-to-working-with-developers
- Priority Therapeutic Areas for Development – FDA, accessed July 23, 2025, https://www.fda.gov/drugs/electronic-regulatory-submission-and-review/priority-therapeutic-areas-development
- Recent FDA Actions Foreshadow a New, Complicated Regulatory Picture – AAF, accessed July 23, 2025, https://www.americanactionforum.org/insight/recent-fda-actions-foreshadow-a-new-complicated-regulatory-picture/
- Who Deserves a Cure? The FDA’s New Gatekeeping Game | Cato at Liberty Blog, accessed July 23, 2025, https://www.cato.org/blog/who-deserves-cure-fdas-new-gatekeeping-game
- The Role of Patents and Regulatory Exclusivities in Drug Pricing | Congress.gov, accessed July 23, 2025, https://www.congress.gov/crs-product/R46679
- Patents and Drug Pricing: Why Weakening Patent Protection Is Not in the Public’s Best Interest – American Bar Association, accessed July 23, 2025, https://www.americanbar.org/groups/intellectual_property_law/resources/landslide/2025-spring/drug-pricing-weakening-patent-protection-not-best-interest/
- How Drug Life-Cycle Management Patent Strategies May Impact Formulary Management, accessed July 23, 2025, https://www.ajmc.com/view/a636-article
- Filing Strategies for Maximizing Pharma Patents: A Comprehensive Guide for Business Professionals – DrugPatentWatch, accessed July 23, 2025, https://www.drugpatentwatch.com/blog/filing-strategies-for-maximizing-pharma-patents/
- The Dark Reality of Drug Patent Thickets: Innovation or Exploitation? – DrugPatentWatch, accessed July 23, 2025, https://www.drugpatentwatch.com/blog/the-dark-reality-of-drug-patent-thickets-innovation-or-exploitation/
- Addressing Patent Thickets To Improve Competition and Lower Prescription Drug Prices – I-MAK, accessed July 23, 2025, https://www.i-mak.org/wp-content/uploads/2023/12/Addressing-Patent-Thickets-Blueprint_2023.pdf
- Strategic Patenting by Pharmaceutical Companies – Should Competition Law Intervene? – PMC, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7592140/
- Pricing of pharmaceuticals is becoming a major challenge for health systems – The BMJ, accessed July 23, 2025, https://www.bmj.com/content/368/bmj.l4627
- 5 Famous Drug Recalls in US History & Why They Happened, accessed July 23, 2025, https://www.hhrlaw.com/blog/2022/march/5-famous-drug-recalls-in-us-history-why-they-hap/
- FDA Approvals and Regulations: Overview | EBSCO Research Starters, accessed July 23, 2025, https://www.ebsco.com/research-starters/law/fda-approvals-and-regulations-overview
- Criticism of the Food and Drug Administration – Wikipedia, accessed July 23, 2025, https://en.wikipedia.org/wiki/Criticism_of_the_Food_and_Drug_Administration
- List of withdrawn drugs – Wikipedia, accessed July 23, 2025, https://en.wikipedia.org/wiki/List_of_withdrawn_drugs
- What Happens When Drugs Fail Post-Approval? – News-Medical.net, accessed July 23, 2025, https://www.news-medical.net/life-sciences/What-Happens-When-Drugs-Fail-Post-Approval.aspx
- How FDA Failures Contributed to the Opioid Crisis – AMA Journal of Ethics, accessed July 23, 2025, https://journalofethics.ama-assn.org/article/how-fda-failures-contributed-opioid-crisis/2020-08
- Slowing Down Accelerated Approval: Examining the Role of Industry Influence, Patient Advocacy Organizations, and Political Pressure, accessed July 23, 2025, https://ir.lawnet.fordham.edu/cgi/viewcontent.cgi?article=5932&context=flr
- What influences healthcare providers’ prescribing decisions? Results from a national survey – FDA, accessed July 23, 2025, https://www.fda.gov/media/151256/download
- Bad Pharma Quotes by Ben Goldacre – Goodreads, accessed July 23, 2025, https://www.goodreads.com/work/quotes/19171192-bad-pharma-how-drug-companies-mislead-doctors-and-harm-patients
- Shine Lecturer Sidney Wolfe: FDA’s Drug Review Process is Broken | SPH, accessed July 23, 2025, https://www.bu.edu/sph/news/articles/2014/shine-lecturer-sidney-wolfe-fdas-drug-review-process-is-broken/
- Procedure for Submitting the HHS-521 Request for Approval of Outside Activity – FDA, accessed July 23, 2025, https://www.fda.gov/media/104760/download
- PROTECTING THE INTEGRITY OF GOVERNMENT SCIENCE – Department of Transportation, accessed July 23, 2025, https://www.transportation.gov/sites/dot.gov/files/2024-10/01-22-Protecting_the_Integrity_of_Government_Science.pdf
- Scientific Integrity at HHS, accessed July 23, 2025, https://www.hhs.gov/programs/research/scientificintegrity/index.html
- Office of Scientific Integrity – FDA, accessed July 23, 2025, https://www.fda.gov/about-fda/office-chief-scientist/office-scientific-integrity
- Master Internal Audits for FDA Compliance: Ultimate Checklist – OurRecords, accessed July 23, 2025, https://ourrecords.com/internal-audits-fda-compliance-guide/
- Notifications on Data Integrity – Medical Devices – FDA, accessed July 23, 2025, https://www.fda.gov/medical-devices/industry-medical-devices/notifications-data-integrity-medical-devices
- Filing Whistleblower Complaints under the FDA Food Safety Modernization Act – OSHA, accessed July 23, 2025, https://www.osha.gov/sites/default/files/publications/OSHA3714.pdf
- FDA Food Safety Modernization Act (FSMA) | Whistleblower Protection Program, accessed July 23, 2025, https://www.whistleblowers.gov/statutes/fda_402
- FDA Food Safety Modernization Act Whistleblower Protection (21 U.S.C. § 399d), accessed July 23, 2025, https://leppardlaw.com/federal/whistleblower/fda-food-safety-modernization-act-whistleblower-protection-21-u-s-c-%C2%A7-399d/
- Whistleblower Protection – Federal Trade Commission OIG, accessed July 23, 2025, https://oig.ftc.gov/whistleblower-protection
- Whistleblower Rights & Protections | Office of Personnel Management – OPM-OIG, accessed July 23, 2025, https://oig.opm.gov/report-oig/whistleblower-rights-protections
- CDER Formal Dispute Resolution – FDA, accessed July 23, 2025, https://www.fda.gov/about-fda/cder-contact-information/cder-formal-dispute-resolution
- Formal Dispute Resolution: Sponsor Appeals Above the Division Level Guidance for Industry and Review Staff – FDA, accessed July 23, 2025, https://www.fda.gov/media/85613/download
- SOPP 8005: Formal Dispute Resolution Process – FDA, accessed July 23, 2025, https://www.fda.gov/media/108908/download
- June 4, 2024 Meeting of the Psychopharmacologic Drugs Advisory Committee – FDA, accessed July 23, 2025, https://www.fda.gov/media/180463/download
- The Relative Contributions of NIH and Private Sector Funding to the Approval of New Biopharmaceuticals – PMC, accessed July 23, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9440766/