Introduction
In the global landscape of medicine, a pharmaceutical drug’s nonproprietary name is far more than a simple identifier. It is a meticulously engineered instrument of public health, a universally understood word designed to transcend linguistic, commercial, and geographical barriers. This nomenclature functions as a codified language, a critical component of communication for every stakeholder in the healthcare continuum, from the research chemist synthesizing a new molecule to the physician prescribing a course of treatment, the pharmacist dispensing the medication, and the patient receiving it.1 The system is built upon a fundamental duality: the proprietary, or brand, name, which serves as a commercial asset for its manufacturer, and the nonproprietary, or generic, name, which exists as a public good, free for all to use.3 Navigating the inherent tension between these market-driven incentives and public health imperatives is the central challenge of pharmaceutical nomenclature.
The architecture and governance of this system are overseen by a triumvirate of key bodies. At the global level, the World Health Organization (WHO) manages the International Nonproprietary Name (INN) Programme, establishing a single, worldwide standard for each active substance.1 Within the United States, the United States Adopted Names (USAN) Council—a unique collaboration of professional medical and pharmaceutical organizations—operates in concert with the WHO to create harmonized names for the U.S. market.5 Finally, the U.S. Food and Drug Administration (FDA) wields ultimate regulatory authority, ensuring that all drug names, both proprietary and nonproprietary, meet stringent safety standards to prevent confusion and protect patients.6
This report provides an exhaustive analysis of this pharmaceutical alphabet. It begins by establishing the foundational principles that distinguish generic from brand-name drugs, exploring the regulatory and economic symbiosis that underpins the modern pharmaceutical market. It then delves into the procedural mechanics of the global (WHO INN) and national (USAN) naming authorities, revealing how a single, harmonized name is forged through international consensus. The subsequent section deconstructs the linguistic code of the drug stem system, presenting a comprehensive lexicon that translates these syllabic components into pharmacological meaning. The analysis then shifts to the clinical interface, where the profound impact of nomenclature on patient safety is examined, with a particular focus on the persistent challenge of Look-Alike, Sound-Alike (SALA) medication errors and the strategies developed to mitigate them. Finally, the report looks to the horizon, exploring the evolving naming conventions for advanced therapeutics such as biologics and gene therapies, and considering the future trajectory of a field continuously challenged by scientific innovation and the enduring quest for global harmonization.
Part I: The Architecture of Drug Nomenclature
Section 1: The Foundation – Generic vs. Brand-Name Pharmaceuticals
Defining the Core Concepts
The distinction between a brand-name drug and its generic equivalent is a cornerstone of modern pharmaceutical regulation and economics. A generic drug is a medication meticulously created to be the same as an already marketed brand-name drug in its most critical aspects. According to the U.S. Food and Drug Administration (FDA), this equivalence must be demonstrated across dosage form, safety, strength, route of administration, quality, performance characteristics, and intended use.7 The central component that unites a brand-name drug and its generic counterpart is the Active Pharmaceutical Ingredient (API)—the substance in the medicine that is pharmaceutically active against the illness or condition it is treating.7 For a generic drug to be approved, its manufacturer must provide scientific evidence proving that its API is identical to that of the innovator drug.7
However, while the API is identical, notable differences are permitted in the inactive ingredients, also known as excipients. These components, which include fillers, binders, colorings, flavorings, and preservatives, do not affect the performance, safety, or effectiveness of the medication.7 These permissible variations in inactive ingredients are the primary reason why a generic drug will often differ in color, shape, and size from its brand-name original.10 In fact, trademark laws explicitly require that generic versions look different from the brand-name drug to avoid confusion.9
The Principle of Bioequivalence
The fundamental scientific standard that allows a generic drug to be considered an equal substitute for a brand-name drug is bioequivalence. This principle demonstrates that the generic medicine works in the same way and provides the same clinical benefit as its brand-name counterpart.7 To establish bioequivalence, generic manufacturers must conduct studies that measure the rate and extent to which the API is absorbed into the bloodstream. The results must show that any differences in absorption between the generic and brand-name products are not statistically significant. A comprehensive study comparing generics to brand-name drugs found, on average, only a 3.5% difference in absorption into the body, a variation considered clinically insignificant.8 By meeting this standard, a generic drug is proven to have the same risks and benefits as the original, allowing patients and healthcare providers to substitute it with confidence.7
Regulatory Pathways and Cost Structures
The significant cost difference between brand-name and generic drugs is a direct result of their distinct regulatory approval pathways. An innovator company seeking to market a new drug must submit a New Drug Application (NDA) to the FDA. This is an exhaustive and monumentally expensive process, involving years of preclinical (animal) and clinical (human) trials to demonstrate the drug’s safety and effectiveness.
Conversely, a company seeking to market a generic version submits an Abbreviated New Drug Application (ANDA). The ANDA process is “abbreviated” because it does not require the applicant to repeat the costly and time-consuming clinical trials of the innovator drug. Instead, the generic manufacturer relies on the FDA’s previous finding that the brand-name product is safe and effective.7 The primary requirements for an ANDA are to demonstrate the generic’s bioequivalence to the brand-name drug and to prove that its manufacturing, packaging, and testing sites meet the same strict quality standards.7 By avoiding the need to duplicate extensive R&D and clinical testing, generic manufacturers can bring their products to market at a fraction of the cost. This regulatory framework is the direct cause of the substantial price reductions seen with generic drugs, which on average cost 80–85% less than their brand-name counterparts.8
The Role of Patents and Market Exclusivity
The entire pharmaceutical market operates on a delicate balance between incentivizing innovation and ensuring public access to affordable medications. This balance is primarily managed through the patent system. When a company develops a new drug, it is granted patent protection and periods of market exclusivity by the FDA. These protections give the innovator company a temporary monopoly, typically lasting for a number of years, during which no generic versions can be marketed.9 The standard patent term is 20 years from the date the patent was filed, though the effective market life is often shorter due to the lengthy development and approval process.9
This period of exclusivity is designed to allow the innovator company to recoup its substantial investment in research and development, which can often exceed a billion dollars.11 Once these patents and exclusivities expire, the market opens up to generic competition. Often, multiple generic manufacturers will enter the market simultaneously, creating intense price competition that further drives down the cost for consumers.9 This event, often referred to as the “patent cliff,” marks the point where the innovator’s revenue from a blockbuster drug can drop precipitously as its market share is rapidly captured by lower-priced generics.
This dynamic reveals that the generic drug industry is not merely a natural market phenomenon but a direct consequence of a deliberate and sophisticated regulatory framework. The system is designed to first reward innovation with a period of profitable monopoly and then, once that period has concluded, to aggressively promote public health and affordability through competition. The ANDA pathway is the central economic lever that makes this transition possible. Without a mechanism to bypass duplicative clinical trials, a competing version of an off-patent drug would be nearly as expensive to develop as the original, offering little cost advantage to the public. By allowing generic manufacturers to rely on the innovator’s established safety data, the ANDA process drastically lowers the barrier to market entry, thereby enabling the profound cost savings that define the generic drug market.7
Section 2: The Global Naming Authority – The WHO International Nonproprietary Name (INN) Programme
Historical Context and Mandate
The imperative for a standardized global system of drug nomenclature was recognized in the mid-20th century as the pharmaceutical landscape became increasingly international. In 1950, the World Health Assembly passed a resolution initiating what would become the International Nonproprietary Name (INN) Programme, which officially began its operations with the publication of the first list of INNs in 1953.1 The constitutional mandate of the World Health Organization (WHO) is to “develop, establish and promote international standards with respect to biological, pharmaceutical and similar products”.2 The INN system is the primary fulfillment of this mandate in the realm of drug naming.
From its inception, the program’s core objective has been to provide healthcare professionals worldwide with a single, unique, and universally available name for each active pharmaceutical substance.1 This universal language is critical for ensuring the “clear identification, safe prescription and dispensing of medicines to patients,” and it facilitates effective communication and information exchange among scientists, regulators, and clinicians across the globe.1
The INN Selection Process
The creation of an INN is a formal, multi-stage process involving rigorous review and international consultation.
- Application: The process typically begins when a pharmaceutical manufacturer submits a request for an INN directly to the WHO. This is usually done when a new drug is in the midst of clinical development, often around Phase II, to ensure a name is established by the time pivotal studies are published.17 The application must be accompanied by precise information on the substance’s chemistry, pharmacological action, and therapeutic use, along with several suggested names.17 As of recent updates, a user fee of US$12,000 is required to process each new INN request, reflecting the complexity of the review.16
- Review: The INN Expert Group, a panel of international specialists, collaborates closely with national nomenclature committees, such as the USAN Council, to examine the submitted information and proposed names.16 This collaborative review is a key mechanism for achieving global harmonization.
- Proposed INN (pINN): Once the Expert Group selects a suitable name, it is published as a “proposed INN” (pINN) in the WHO’s official journal, WHO Drug Information.2 This publication initiates a four-month period during which any interested party can submit comments or formal objections to the proposed name.20
- Recommended INN (rINN): If no substantive objections are raised during the comment period, the name is elevated to the status of a “recommended INN” (rINN).2 At this point, it becomes the official, globally recognized nonproprietary name for that substance. The WHO periodically updates and publishes a cumulative list of all rINNs, which now numbers over 8,000 distinct names.19
Principles of INN Creation and Linguistics
The construction of an INN is guided by several core principles designed to maximize safety and utility.
- Uniqueness and Safety: First and foremost, an INN must be distinctive in both sound and spelling to prevent confusion with other drug names or common words, an issue that could “jeopardize the safety of patients”.1
- Public Domain: INNs are formally placed in the public domain, designating them as “nonproprietary”.16 They are public property and can be used without restriction to identify a pharmaceutical substance. A critical corollary to this principle is that commercial trademarks must not be derived from INNs, nor should they incorporate the common stems used in INNs, as this would hinder the creation of future names within a pharmacological class and create a risk of confusion.1
- Translingual Communication: The system is inherently international. To ensure universal applicability, INNs are published in multiple official languages, including English, Latin, French, Spanish, Russian, Chinese, and Arabic, and are often designed to be cognates across these languages.2 Furthermore, the WHO employs a system of spelling regularization to facilitate consistent pronunciation and avoid ambiguity. This includes using “f” instead of “ph,” “t” instead of “th,” and “e” instead of “ae” or “oe,” while avoiding letters like “h” and “k” where possible.2
Global Harmonization and Collaboration
The success of the INN system hinges on its widespread adoption, which is achieved through deep and ongoing collaboration with national nomenclature authorities. As a result of this close partnership, national names such as British Approved Names (BAN), Japanese Adopted Names (JAN), and United States Adopted Names (USAN) are, with very rare exceptions, identical to the INN.1 This harmonization ensures that when a new drug is approved, it carries the same nonproprietary name in virtually every market around the world, fulfilling the program’s primary mission.
The INN system, therefore, functions as more than just a naming convention; it is a piece of critical global public health infrastructure. Its role is analogous to that of standardized units of measurement or universal communication protocols. The primary value of the INN lies not just in assigning a name but in creating a standardized, interoperable data layer that underpins global pharmacovigilance, scientific research, and clinical practice. Without a common identifier, aggregating safety data from different countries would be an insurmountable challenge, as the same active substance could be known by dozens of disparate local names—the classic example being paracetamol (the INN) and acetaminophen (the USAN, which is now a rare exception to the harmonization rule).3 The INN provides the unique, globally recognized key that allows a researcher in Tokyo, a clinician in São Paulo, and a regulator in Brussels to communicate about the exact same pharmaceutical ingredient with absolute clarity.1 This standardization is the foundation for scientific literature, international drug regulation, and the creation of global health databases, such as the World Intellectual Property Organization’s (WIPO) Pat-INFORMED database, which is searchable by INN.24 Consequently, the INN system is a foundational tool that enables global cooperation in medicine and prevents the fragmentation of critical health information, making a direct and indispensable contribution to patient safety worldwide.
Section 3: The United States Naming System – The USAN Council
Genesis and Governance
While the WHO’s INN Programme provides the global framework for nonproprietary drug naming, the United States operates a parallel, harmonized system managed by the United States Adopted Names (USAN) Council. The council was established in June 1961 as a cooperative venture between the American Medical Association (AMA) and the United States Pharmacopeial Convention (USP) to address concerns about the lack of a centralized, mandatory naming system in the U.S..3 The American Pharmacists Association (APhA) joined as the third sponsoring organization in 1964, solidifying the council’s unique governance structure.3
The USAN Council is composed of five members: one volunteer expert nominated by each of the three sponsoring organizations (AMA, USP, APhA), one member-at-large selected by the sponsors, and a non-voting liaison member from the FDA.3 This structure embodies a collaboration between key professional bodies in medicine, pharmacy, and pharmacopeial standards, working in concert with the federal regulator.
The USAN Negotiation Process
The assignment of a USAN is a formal procedure referred to as a “negotiation,” reflecting the collaborative dialogue between the drug sponsor, the council, and international bodies.5
- Application: A pharmaceutical firm typically initiates the process by filing an application with the USAN Program after the drug has entered clinical trials and has been assigned an Investigational New Drug (IND) number by the FDA.3 The application includes several proposed names, detailed chemical and pharmacological data, and a rationale for the suggested stem assignment, which indicates the drug’s class.5
- Review and Negotiation: Upon receipt, the application is assigned to a USAN staff member, or “negotiator,” who serves as the primary point of contact.5 The staff reviews the submission for completeness, checks the proposed names for conflicts with existing generic or proprietary names, and assesses whether the names appropriately reflect the drug’s action according to established nomenclature schemes.5 A ballot is then prepared for the USAN Council, containing the firm’s proposals and any alternatives suggested by the staff. The Council evaluates the names based on several key criteria, including whether the name reflects the drug’s action, how easily it can be pronounced and remembered, and how well it translates into other languages.5
- Harmonization with INN: A pivotal step in the process is achieving global harmonization. The USAN Council works in close conjunction with the WHO INN Expert Committee to ensure that a single, globally acceptable name is selected.3 This collaboration is so ingrained that consensus among the sponsoring firm, the USAN Council, and the INN experts is a prerequisite for the formal adoption of a USAN.5 To prevent divergence, applicants are required to notify the USAN Program if they receive any correspondence from the INN indicating comments or objections to a proposed name, ensuring that two different nonproprietary names are not established for the same compound.28
- Adoption and Publication: Once a consensus name is agreed upon by all parties, the USAN is formally adopted. The adopted name is then published online and forwarded to key scientific bodies like the Chemical Abstracts Service and the USP.5
The FDA’s Overarching Authority
The relationship between the USAN Council and the FDA illustrates the interplay between professional self-regulation and statutory government oversight. The Federal Food, Drug, and Cosmetic Act grants the FDA the ultimate authority to designate the official “established name” for any drug marketed in the United States.6 However, in a significant policy decision in 1984, the FDA announced that it would defer to the USAN as the established name for new single-entity drugs, rather than creating its own list.3
This deference streamlines the process, but the FDA retains its statutory power. The agency has a representative on the USAN Council and has the final authority to accept or reject any name proposed as an established name, including a USAN.3 This legal hierarchy ensures that while the naming process is driven by a consensus of professional experts and industry stakeholders, the final name must always meet the FDA’s stringent safety and regulatory standards.
Scope of Naming
The USAN Council’s mandate has expanded over time to keep pace with therapeutic innovation. In addition to traditional small-molecule drugs, the council is responsible for assigning nonproprietary names to a wide range of other medical products, including agents for gene therapy and cell therapy, contact lens polymers, surgical materials, and diagnostic agents.3 This broad scope underscores the council’s central role in establishing clear and consistent nomenclature across the spectrum of modern healthcare technologies.
The structure and operation of the USAN Council can be seen as a reflection of the broader U.S. healthcare system’s unique model. It is not a purely governmental body but rather a collaborative entity composed of private, professional organizations (AMA, USP, APhA) that set standards through consensus.3 This mirrors how professional standards in medicine are often developed by specialty boards and medical associations rather than by direct government decree. The process is explicitly defined as a “negotiation” that directly involves the commercial interests of the pharmaceutical firm, acknowledging the private industry’s central role in drug development.5 Meanwhile, the federal regulator—the FDA—maintains ultimate legal authority but chooses to defer to the expertise and consensus of this multi-stakeholder group, intervening primarily to enforce safety and legal standards.6 This framework represents a distinctly American approach, balancing professional expertise, commercial interests, and public safety through a structured, cooperative, yet legally hierarchical system.
Part II: The Language of Pharmacology – The Stem System
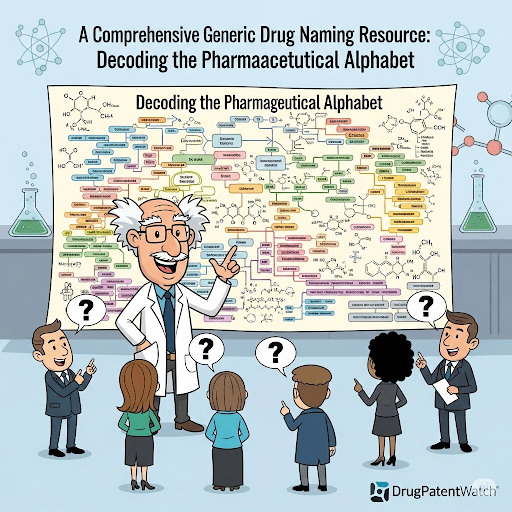
Section 4: Deconstructing the “Pharmaceutical Alphabet”
The Logic of Stems
The modern system of nonproprietary drug nomenclature is built upon a logical and informative foundation known as the stem system. A stem is a standardized syllable or group of syllables embedded within a drug’s generic name that serves as a “family name,” immediately identifying the drug’s relationship to a class of substances with similar pharmacological actions, chemical structures, or both.2 This systematic approach is a powerful tool for healthcare professionals, as it provides instant recognition of a drug’s therapeutic category, mechanism of action, and potential effects, thereby enhancing prescribing safety and efficiency.31
Anatomy of a Generic Name
A typical generic name is constructed from two main components, each with a distinct function:
- Stem: This is the core informational component of the name. The stem conveys the drug’s pharmacological classification. While most commonly used as a suffix at the end of the name (e.g., -olol for beta-blockers, -statin for HMG-CoA reductase inhibitors), a stem can also appear as a prefix at the beginning (e.g., cef- for cephalosporin antibiotics) or as an infix within the name (e.g., -grel- for platelet aggregation inhibitors).3
- Prefix: This component is a unique and often “fantasy” syllable or syllables that precedes the stem. The prefix has no intrinsic pharmacological meaning; its primary purpose is to create a distinctive, euphonious, and memorable name that differentiates the drug from other members of the same class.20 For example, in the names
atenolol and metoprolol, the -olol stem identifies both as beta-blockers, while the prefixes aten- and meto- serve as unique identifiers.
The Evolution of the Stem System
The development of the stem-based system represents a significant evolution in pharmaceutical nomenclature. Early drug names were often based on their complex chemical structures.3 As medicinal chemistry advanced and new drugs became more numerous and structurally intricate, these chemically derived names grew increasingly long, unwieldy, and difficult for non-chemists to pronounce or remember.3 More importantly, they provided little practical information to the physicians, pharmacists, and nurses who prescribed and administered them. Recognizing this limitation, nomenclature bodies shifted toward the current system, which prioritizes clinical utility. The stem system was designed to meet the needs of healthcare professionals by embedding clear, concise pharmacological relationships directly into the drug names themselves.3
The Process for Establishing New Stems
The stem system is a living language that must evolve to accommodate novel classes of drugs with new mechanisms of action. However, the creation of a new stem is a deliberate and rigorous process designed to preserve the integrity and usefulness of the existing nomenclature. The USAN Council, for instance, actively discourages excessive stem creation, believing it diminishes the system’s value.31
When a pharmaceutical company develops a truly novel substance that does not fit within any existing stem class, it can petition for the creation of a new one. The burden of proof falls on the applicant to provide substantial data demonstrating that the substance is unique in its chemical structure or pharmacological action.31 Before a new stem is formally adopted, the WHO often publishes it as a “pre-stem” for a period of public consultation.19 This transparent and consultative approach allows experts and stakeholders worldwide to provide feedback, ensuring that any new addition to the pharmaceutical alphabet is logical, necessary, and globally accepted. This careful stewardship maintains the system’s coherence and ensures that each stem remains a meaningful and reliable indicator of a drug’s properties.
This systematic approach to naming is more than a simple classification scheme; it functions as a powerful cognitive heuristic designed to enhance clinical decision-making. The sheer number of available medications is vast and continually expanding, making it impossible for any single clinician to memorize the detailed pharmacology of every agent.15 The stem system addresses this challenge by reducing the cognitive load on practitioners. By grouping drugs into families with a shared stem, the system leverages the power of pattern recognition. When a clinician encounters a new drug name, such as “rosuvastatin,” the
-statin stem immediately activates a mental schema associated with HMG-CoA reductase inhibitors.32 This schema includes the drug class’s mechanism of action (cholesterol synthesis inhibition), primary indications (hyperlipidemia), and key side effect profile (myopathy, liver enzyme elevation). This instant recognition is a cognitive shortcut that bypasses the need to consult a reference from scratch, thereby speeding up the prescribing and safety-checking process. In this way, the stem system is a deliberately engineered cognitive tool that improves clinical efficiency and patient safety by making critical pharmacological information immediately and intuitively accessible.
Section 5: A Lexicon of Common Pharmaceutical Stems
The stem system provides a structured language for understanding the relationships between different drugs. For clinicians, pharmacists, and students, a well-organized lexicon of these stems is an invaluable tool for learning and practice. The following table presents a comprehensive list of the most clinically relevant drug stems, organized by therapeutic category. This structure, unlike a simple alphabetical list, is designed to be clinically intuitive, allowing users to explore the nomenclature within a specific field of practice. It should be noted that this list is not exhaustive, as the nomenclature process is dynamic, with new stems being created and older definitions modified as scientific understanding evolves.31
| Therapeutic Category | Stem | Definition/Drug Class | Examples (Generic Name, Brand Name) |
| Cardiovascular System | -pril | Antihypertensives (ACE inhibitors) | Lisinopril (Zestril), Captopril (Capoten) 33 |
| -sartan | Angiotensin II receptor antagonists | Losartan (Cozaar), Valsartan (Diovan) 33 | |
| -olol | Beta-blockers (β-adrenergic receptor antagonists) | Metoprolol (Lopressor), Atenolol (Tenormin) 33 | |
| -dipine | Calcium channel blockers (dihydropyridine type) | Amlodipine (Norvasc), Nifedipine (Procardia) 40 | |
| -statin | Antihyperlipidemics (HMG-CoA reductase inhibitors) | Atorvastatin (Lipitor), Simvastatin (Zocor) 42 | |
| -thiazide | Diuretics (thiazide type) | Hydrochlorothiazide (Microzide) 33 | |
| -semide | Diuretics (loop type) | Furosemide (Lasix), Torsemide (Demadex) 42 | |
| -parin | Anticoagulants (heparin derivatives/LMWH) | Enoxaparin (Lovenox), Dalteparin (Fragmin) 33 | |
| -arol | Anticoagulants (dicumarol derivatives) | Warfarin (Coumadin) 40 | |
| -grel- | Platelet aggregation inhibitors | Clopidogrel (Plavix), Ticagrelor (Brilinta) 33 | |
| -teplase | Thrombolytics (tissue plasminogen activators) | Alteplase (Activase), Reteplase (Retavase) 40 | |
| Anti-Infectives | -cillin | Antibiotics (penicillin derivatives) | Amoxicillin (Amoxil), Penicillin G 33 |
| cef- | Antibiotics (cephalosporin derivatives) | Cefazolin (Ancef), Ceftriaxone (Rocephin) 40 | |
| -penem | Antibiotics (carbapenem derivatives) | Imipenem/cilastatin (Primaxin), Meropenem (Merrem) 40 | |
| -cycline | Antibiotics (tetracycline derivatives) | Doxycycline (Vibramycin), Tetracycline 40 | |
| -mycin | Antibiotics (macrolide or other origins) | Azithromycin (Zithromax), Erythromycin 33 | |
| -floxacin | Antibiotics (fluoroquinolone derivatives) | Ciprofloxacin (Cipro), Levofloxacin (Levaquin) 32 | |
| sulfa- | Antibiotics (sulfonamides) | Sulfamethoxazole (component of Bactrim) 40 | |
| -conazole | Antifungals (systemic, miconazole type) | Fluconazole (Diflucan), Ketoconazole (Nizoral) 40 | |
| -fungin | Antifungals (echinocandin type) | Caspofungin (Cancidas), Micafungin (Mycamine) 32 | |
| -vir | Antivirals (general) | Acyclovir (Zovirax), Oseltamivir (Tamiflu) 2 | |
| -ciclovir | Antivirals (acyclovir type) | Acyclovir (Zovirax), Ganciclovir (Cytovene) 45 | |
| -navir | Antivirals (HIV protease inhibitors) | Ritonavir (Norvir), Lopinavir (component of Kaletra) | |
| Central Nervous System | -azepam | Anxiolytics (benzodiazepine type) | Diazepam (Valium), Lorazepam (Ativan) 33 |
| -zolam | Anxiolytics (benzodiazepine type) | Alprazolam (Xanax), Midazolam (Versed) 32 | |
| -barb- | Sedatives/Hypnotics (barbituric acid derivatives) | Phenobarbital (Luminal), Secobarbital (Seconal) 33 | |
| -oxetine | Antidepressants (fluoxetine type/SSRI) | Fluoxetine (Prozac), Paroxetine (Paxil) 33 | |
| -triptyline | Antidepressants (tricyclic type) | Amitriptyline (Elavil), Nortriptyline (Pamelor) 33 | |
| -pramine | Antidepressants (imipramine type) | Imipramine (Tofranil), Clomipramine (Anafranil) 33 | |
| -peridol | Antipsychotics (haloperidol type) | Haloperidol (Haldol) 33 | |
| -apine | Antipsychotics (atypical) | Olanzapine (Zyprexa), Quetiapine (Seroquel) 42 | |
| -idone | Antipsychotics (risperidone type) | Risperidone (Risperdal), Paliperidone (Invega) 33 | |
| -triptan | Antimigraine agents (5-HT receptor agonists) | Sumatriptan (Imitrex), Rizatriptan (Maxalt) 44 | |
| Pain and Inflammation | -caine | Local anesthetics | Lidocaine (Xylocaine), Bupivacaine (Marcaine) 40 |
| -profen | Anti-inflammatory/analgesic agents (NSAIDs) | Ibuprofen (Advil, Motrin), Ketoprofen 33 | |
| -ac | Anti-inflammatory agents (NSAIDs, acetic acid type) | Diclofenac (Voltaren), Ketorolac (Toradol) 39 | |
| -coxib | Anti-inflammatory agents (COX-2 inhibitors) | Celecoxib (Celebrex) 45 | |
| -codone | Opioid analgesics | Hydrocodone (Vicodin), Oxycodone (OxyContin) | |
| -morphone | Opioid analgesics | Hydromorphone (Dilaudid), Oxymorphone (Opana) | |
| Endocrine and Metabolic | gli- | Antihyperglycemics (sulfonylureas) | Glipizide (Glucotrol), Glyburide (DiaBeta) 40 |
| -glitazone | Antihyperglycemics (thiazolidinedione type) | Pioglitazone (Actos), Rosiglitazone (Avandia) 33 | |
| -gliptin | Antihyperglycemics (DPP-4 inhibitors) | Sitagliptin (Januvia), Saxagliptin (Onglyza) 45 | |
| -tide | Peptides and glycopeptides (e.g., GLP-1 agonists) | Liraglutide (Victoza), Semaglutide (Ozempic) 33 | |
| pred- | Corticosteroids (prednisone derivatives) | Prednisone, Prednisolone 33 | |
| -sone | Corticosteroids | Betamethasone, Dexamethasone 42 | |
| -dronate | Bone resorption inhibitors (bisphosphonates) | Alendronate (Fosamax), Risedronate (Actonel) 39 | |
| Oncology | -rubicin | Antineoplastic antibiotics (anthracyclines) | Doxorubicin (Adriamycin), Epirubicin (Ellence) 33 |
| -mustine | Antineoplastics (alkylating agents) | Carmustine (BiCNU), Lomustine (CeeNU) 40 | |
| -tinib | Antineoplastics (tyrosine kinase inhibitors) | Imatinib (Gleevec), Erlotinib (Tarceva) 44 | |
| -mab | Monoclonal antibodies (pre-2021 nomenclature) | Trastuzumab (Herceptin), Rituximab (Rituxan) 47 | |
| -taxel | Antineoplastics (taxane derivatives) | Paclitaxel (Taxol), Docetaxel (Taxotere) | |
| Gastrointestinal | -prazole | Proton-pump inhibitors (anti-ulcer) | Omeprazole (Prilosec), Pantoprazole (Protonix) 33 |
| -tidine | H2-receptor antagonists (anti-ulcer) | Ranitidine (Zantac), Cimetidine (Tagamet) 40 | |
| -setron | Antiemetics (5-HT3 receptor antagonists) | Ondansetron (Zofran), Granisetron (Kytril) 40 | |
| Respiratory | -terol | Bronchodilators (β-agonist type) | Albuterol (ProAir), Salmeterol (Serevent) 33 |
| -lukast | Antiasthmatics (leukotriene receptor antagonists) | Montelukast (Singulair), Zafirlukast (Accolate) 40 | |
| -adine | Antihistamines (H1 receptor antagonists) | Loratadine (Claritin), Fexofenadine (Allegra) 33 |
Part III: Nomenclature at the Clinical Interface – Patient Safety and Medication Errors
Section 6: When Names Collide – The Challenge of Look-Alike, Sound-Alike (SALA) Drugs
The Scope of the Problem
While the systematic nature of drug nomenclature is designed to enhance clarity and safety, it paradoxically creates vulnerabilities. The sheer volume of pharmaceuticals, combined with the linguistic constraints of creating unique names, inevitably leads to products with names that look or sound similar. These Look-Alike, Sound-Alike (SALA) drugs represent a significant and persistent threat to patient safety.48 The potential for confusion is not a minor issue; it is a leading cause of medication errors. Data from national error reporting programs indicate that confusion arising from similar drug names accounts for approximately 25% of all reported medication errors.50 In the United States, it is estimated that roughly one in every thousand prescriptions filled results in the wrong drug being dispensed due to name confusion.51 These are not mere clerical mistakes; they can lead to severe patient harm, including underdosing, overdosing, exposure to unintended side effects, and failure to treat the underlying condition, sometimes with fatal consequences.49
Causal Factors
SALA errors are rarely caused by a single point of failure. Instead, they typically arise from a confluence of human factors and systemic weaknesses that create an environment where a latent vulnerability—the similarity between two names—can manifest as an active error. Key contributing factors include:
- Illegible Handwriting: Poorly written prescriptions are a classic source of ambiguity, making it easy to misinterpret one drug name for another.48
- Verbal and Telephone Orders: Spoken communication, especially over the phone, can lead to phonetic confusion, where a sound-alike name is heard incorrectly.53
- Similar Packaging and Labeling: Manufacturers sometimes use similar color schemes, logos, or label designs for different products, which can lead to “look-alike” errors during selection from a shelf or cabinet.49
- Computerized Prescriber Order Entry (CPOE) and Pharmacy Systems: Drop-down menus and search functions that list drug names alphabetically can place SALA pairs directly next to each other, increasing the risk of an incorrect selection, particularly in a fast-paced environment.50
- Confirmation Bias: Healthcare professionals, under pressure, may see what they expect to see. When presented with an unfamiliar name, they may unconsciously substitute a more familiar, similar-sounding name, a cognitive shortcut known as confirmation bias.53
Case Studies in Confusion
The real-world consequences of SALA errors are best illustrated through specific cases where name confusion led to patient harm:
- FORADIL vs. TORADOL: A handwritten prescription for the long-acting bronchodilator formoterol (Foradil) was misinterpreted by a pharmacist as the potent nonsteroidal anti-inflammatory drug (NSAID) ketorolac (Toradol). The error highlights the danger of confusing drugs from entirely different therapeutic classes.50
- PLAVIX vs. PAXIL: A hospitalized patient reported taking “Plaxil” at home, a mispronunciation of the antiplatelet agent clopidogrel (Plavix). The admitting physician misinterpreted this as the antidepressant paroxetine (Paxil) and prescribed it, leading to several days of severe disorientation for the patient.50
- Morphine vs. Hydromorphone: This pair of potent opioids is one of the most frequently confused and dangerous SALA combinations, implicated in 32% of opiate-related SALA error reports. A common contributing factor is the mistaken belief that hydromorphone is the generic name for morphine. As hydromorphone is several times more potent than morphine on a milligram-for-milligram basis, such a mix-up can easily lead to a fatal overdose.50
- Clopidogrel vs. Clozapine: In a documented hospital case, a patient was prescribed the antiplatelet drug clopidogrel. Due to name similarity, a nurse dispensed the potent atypical antipsychotic clozapine instead. Shortly after administration, the patient was found unconscious, requiring emergency intervention and transfer to the intensive care unit. The investigation revealed the nurse, working under time pressure in a noisy environment, had “skimmed” the prescription rather than reading it thoroughly.57
The Role of the Institute for Safe Medication Practices (ISMP)
In response to the ongoing threat of SALA errors, the Institute for Safe Medication Practices (ISMP), a non-profit patient safety organization, has become a leading authority. The ISMP operates the National Medication Errors Reporting Program (ISMP MERP), a voluntary system that collects and analyzes error reports from healthcare professionals across the country.58 Based on this data, the ISMP publishes its widely recognized “List of Confused Drug Names,” a critical resource that alerts clinicians, pharmacists, and healthcare systems to high-risk SALA pairs.59 This list serves as the foundation for many of the risk-reduction strategies implemented in hospitals and pharmacies nationwide.
The analysis of these errors reveals a crucial pattern: the similar drug name itself is a latent system vulnerability. This vulnerability, however, is most often activated by active failures and systemic pressures within the clinical environment. The case of the clopidogrel/clozapine mix-up, for example, was not caused solely by the similar names but was triggered by a high-pressure work environment that led to a cognitive shortcut.57 Similarly, errors originating from CPOE systems are a product of software design that fails to account for the known risk of placing SALA pairs in close proximity.56 This understanding reframes the problem of SALA errors. It is not an issue of individual carelessness but a systemic failure that requires a multi-layered, system-based approach to prevention, addressing not only the names themselves but the processes, technologies, and human factors that surround their use.
Section 7: Proactive Strategies for Mitigating Risk
Addressing the complex challenge of SALA errors requires a multifaceted approach involving regulatory oversight, visual differentiation strategies, robust clinical practices, and systemic safeguards within healthcare organizations. The goal is to build multiple layers of defense to intercept potential errors before they can reach the patient.
Regulatory Interventions: The FDA’s Role in Prevention
The FDA plays a critical gatekeeping role in preventing potentially confusing drug names from entering the market in the first place. This proactive review is a cornerstone of the agency’s medication safety efforts.
- Proprietary Name Review: Before a new drug is approved, its proposed proprietary (brand) name undergoes a rigorous evaluation by the FDA’s Division of Medication Error Prevention and Analysis (DMEPA).63 DMEPA’s primary focus is safety. Its multidisciplinary team of safety analysts scrutinizes proposed names for any potential similarities to existing drug names—both brand and generic. This involves a detailed assessment of orthographic (look-alike) and phonetic (sound-alike) characteristics.64 To aid this analysis, the FDA developed and uses the Phonetic and Orthographic Computer Analysis (POCA) program, a software tool that employs an advanced algorithm to score the similarity between two names.65 If a proposed name is deemed to have an unacceptable risk of being confused with another product, the FDA will reject it, requiring the manufacturer to submit a new proposal.65
- Promotional Review: In parallel, the FDA’s Office of Prescription Drug Promotion (OPDP) reviews proposed names to ensure they are not “fanciful” or promotional in a way that could be misleading.64 The OPDP assesses whether a name might overstate the drug’s efficacy, imply minimized risk, or make unsubstantiated claims of superiority, all of which could contribute to inappropriate prescribing or use.64
Visual Differentiation: The “Tall Man Lettering” (TML) Initiative
For SALA pairs that already exist in the market, one of the most widely adopted risk-reduction strategies is “Tall Man Lettering” (TML).
- Concept and Application: TML is the practice of using a mix of lowercase and uppercase letters within a drug name to visually emphasize the differences between two look-alike names. For example, the commonly confused pair hydralazine and hydroxyzine are rendered as hydrALAZINE and hydrOXYzine.53 This simple visual cue is designed to interrupt the automatic processing of the name by the reader, forcing them to pay closer attention to the differing parts of the words.
- Adoption and Standardization: The use of TML is strongly promoted by the FDA, the ISMP, and The Joint Commission.59 Both the FDA and ISMP publish official lists of drug pairs with recommended TML formatting to encourage standardization across healthcare settings, from pharmacy labels and computer screens to automated dispensing cabinets.61
- Efficacy: While TML is a widely implemented and low-cost intervention, evidence regarding its effectiveness is mixed. Some laboratory-based studies have shown that it can reduce selection errors, but real-world analyses have yielded less conclusive results.67 The expert consensus, however, is that TML is a valuable component of a comprehensive medication safety program, serving as one of many necessary layers of defense.70
The Pharmacist’s Critical Role in Error Interception
Pharmacists are positioned at a critical juncture in the medication-use process and serve as the final safety net for intercepting prescribing errors, including those related to SALA drugs. Their role extends far beyond dispensing and involves several key safety functions:
- Order Clarification: Pharmacists are responsible for clarifying any prescription that is ambiguous, illegible, or incomplete. This includes contacting the prescriber to verify the drug name, strength, and indication when a potential SALA confusion is suspected.53
- Use of Technology: Modern pharmacy information systems can be configured with alerts that warn the pharmacist when a prescription is entered for a drug on the ISMP’s high-alert or SALA lists, prompting a second look.73
- Safe Dispensing Practices: Pharmacists can implement physical safeguards, such as storing SALA medications on different shelves or in separate, clearly marked bins to prevent selection errors. The use of barcode scanning technology during the dispensing process provides a crucial technological verification step, ensuring the product being dispensed matches the one entered in the system.74
- Patient Education: Counseling patients on their medications is a vital safety function. By confirming the medication’s name (both brand and generic) and its purpose with the patient, the pharmacist empowers the patient to become an active participant in their own safety and to question any discrepancies they may notice later.74
Best Practices for Healthcare Systems
Ultimately, preventing SALA errors requires a system-wide commitment to safety, integrating technology, standardizing processes, and fostering a culture of vigilance. Key best practices for hospitals and health systems include:
- Technological Safeguards: Implementing barcode medication administration (BCMA) ensures that the right patient receives the right drug at the right time. CPOE systems should be configured to minimize risk by, for example, requiring prescribers to enter at least the first five letters of a drug name during a search, which reduces the number of SALA pairs appearing together on a selection screen.68
- Standardization of Orders: Institutions should create and enforce policies that discourage the use of error-prone abbreviations and unofficial “stemmed” names (e.g., ordering “a statin”). For high-risk SALA pairs, policies may require the use of both brand and generic names on all orders. Critically, including the drug’s indication on the prescription provides essential clinical context that can help a pharmacist or nurse catch a potential error (e.g., an order for the anticonvulsant Keppra to treat a bacterial infection would immediately raise a red flag, preventing confusion with the antibiotic Keflex).68
- Safe Storage Practices: In patient care areas, SALA medications should be physically separated in automated dispensing cabinets (ADCs) and medication carts. The use of auxiliary labels, highlighting, or TML on storage bins can provide additional visual cues to prevent mix-ups.74
Part IV: Advanced Topics and Future Horizons
Section 8: Naming Biologics, Biosimilars, and Advanced Therapies
The established nomenclature systems, designed primarily for chemically synthesized small-molecule drugs, face significant challenges when applied to the new frontier of advanced therapeutics. Biologics, biosimilars, and cell and gene therapies possess a level of complexity that demands a more nuanced and descriptive approach to naming.
The Complexity of Biologics
The fundamental difference between a traditional generic drug and a biosimilar lies in their molecular nature. A small-molecule drug like atorvastatin is a relatively simple chemical compound that can be synthesized and replicated with perfect fidelity. Consequently, its generic version is identical to the brand-name original.81 Biologics, in contrast, are large, highly complex molecules—such as monoclonal antibodies or therapeutic proteins—that are produced by living organisms (e.g., bacteria, yeast, or mammalian cells).37 Due to the inherent variability of biological processes, it is impossible to create an exact copy of a biologic. Instead, a follow-on product, known as a “biosimilar,” is engineered to be “highly similar” to the original reference product, with no clinically meaningful differences in terms of safety, purity, and potency.81 This intrinsic lack of identicality is the central reason why the traditional naming system has been deemed insufficient for this class of medicines.
The Biosimilar Naming Debate: The Four-Letter Suffix
The question of how to name biosimilars has sparked a significant international debate, revealing differing regulatory philosophies and priorities.
- The FDA’s Suffix-Based Approach: In the United States, the FDA has implemented a naming convention that requires a unique, four-letter, meaningless suffix to be attached with a hyphen to the nonproprietary name of all new biologics, including reference products and their biosimilars.82 For example, a biosimilar to a reference product named
replicamab-hjxf might be named replicamab-cznm.85 The FDA’s stated rationale for this policy is twofold: to enhance pharmacovigilance by making it easier to trace adverse events to a specific manufacturer’s product, and to prevent the inadvertent substitution of products that have not been deemed “interchangeable” by the agency.83 - Global Divergence and Stakeholder Opinions: This U.S.-centric approach stands in contrast to the conventions in Europe and those followed by the WHO. The European Medicines Agency (EMA) has not required suffixes, arguing that existing product identifiers, such as the brand name and batch number, are sufficient for effective pharmacovigilance.87 This divergence highlights a major fault line in the quest for global regulatory harmonization. The debate has drawn strong opinions from various stakeholders. Proponents of the suffix system, often innovator biologic companies, argue that unique names are essential for patient safety and accurate tracking.86 Conversely, opponents, including the U.S. Federal Trade Commission (FTC), biosimilar manufacturers, and various pharmacy and payer groups, contend that the suffixes create unnecessary confusion, may falsely imply that biosimilars are clinically different or inferior to their reference products, and could ultimately hinder market uptake and undermine the cost-saving potential of biosimilars.81
Emerging Frameworks for Cell and Gene Therapies
The nomenclature challenge becomes even more acute with the advent of cell and gene therapies, which are not single molecules but complex therapeutic systems. In response, the USAN Council and the WHO’s INN Programme have collaborated to develop novel, more descriptive naming schemes.
For genetically modified cell-based therapies, a harmonized two-word naming convention has been established.91 This system is designed to convey information about both the genetic modification and the cellular component:
- First Word (Gene Component): This word describes the genetic material being delivered. It is constructed with a random, unique prefix; an infix that denotes the gene’s function or target (e.g., -kin- for an interleukin gene); and the stem -gene.
- Second Word (Cell/Vector Component): This word identifies the cellular vehicle. It is composed of an infix that specifies the cell type (e.g., -leu- for lymphocytes or -tem- for stem cells) and the stem -cel. For gene therapies that use a viral vector instead of cells, this second word describes the vector, using an infix for the virus type (e.g., -parvo- for an adeno-associated virus) and a stem like -vec to indicate it is a vector.
An example is tisagenlecleucel, the nonproprietary name for the CAR-T therapy Kymriah. This name deconstructs to tisa-gen-lec-leucel, indicating a therapy involving a gene modification (-gen-) delivered via leucocytes (-leu-) that is a cellular therapy (-cel). This modular, descriptive approach represents a necessary evolution of nomenclature to keep pace with the increasing complexity of modern therapeutics.
This evolution in naming conventions is a direct reflection of advancing science and reveals differing regulatory philosophies. The progression from a single, shared name for identical small molecules (fluoxetine), to a suffixed name for “highly similar” biologics (infliximab-abda), to a descriptive two-word name for multi-component cell therapies (tisagenlecleucel) mirrors the escalating complexity of the medicines themselves. Furthermore, the global disagreement over biosimilar suffixes exposes a fundamental philosophical divide. The FDA’s approach prioritizes the precise identification of each unique product for pharmacovigilance, potentially at the cost of creating market friction and a perception of difference that could slow biosimilar adoption.86 The EMA’s approach, in contrast, prioritizes the concept of biosimilarity by using a shared nonproprietary name, relying on existing systems like brand names and lot numbers for traceability. This may foster greater clinical confidence in interchangeability and accelerate market competition.87 Thus, the seemingly simple question of how to name a drug becomes a proxy for a much larger debate about how regulators should balance the promotion of competition with the management of uncertainty for new and complex classes of medicine.
Section 9: Case Studies in Naming, Patents, and Market Strategy
The nonproprietary name of a drug exists at the intersection of science, regulation, and commerce. An examination of some of the most significant drugs in pharmaceutical history reveals how their nomenclature, patent lifecycle, and market strategy are deeply intertwined.
Atorvastatin (Lipitor): The Blockbuster and the Patent Cliff
- Nomenclature and Development: The generic name atorvastatin clearly identifies the drug’s class through the -vastatin stem, which designates HMG-CoA reductase inhibitors used to lower cholesterol.42 The brand name,
Lipitor, was chosen to be evocative of the drug’s effect on lipids.94 Synthesized by Parke-Davis (later acquired by Pfizer) in 1985 and approved by the FDA in 1996, atorvastatin quickly became the world’s best-selling drug, generating over $125 billion in sales during its patent-protected life.96 - Patent Expiration and Market Strategy: The primary U.S. patent for Lipitor expired on November 30, 2011, a highly anticipated event known as a “patent cliff” that exposed the brand to generic competition.96 In the years leading up to and following this date, Pfizer executed a multi-pronged strategy to mitigate the inevitable revenue loss. This included aggressive direct-to-consumer advertising campaigns featuring slogans like “Only Lipitor is Lipitor,” which were designed to instill brand loyalty and create a perception of uniqueness that might make patients hesitant to switch to a generic version.99 Despite these efforts, the entry of generic atorvastatin led to a dramatic and rapid erosion of Lipitor’s market share, demonstrating the powerful economic impact of patent expiration on even the most successful blockbuster drugs.
Sildenafil (Viagra): Strategic Patenting and Controlled Generic Entry
- Nomenclature and Discovery: The generic name sildenafil uses the -afil stem, which signifies a phosphodiesterase-5 (PDE5) inhibitor with vasodilator action.20 The iconic brand name
Viagra was crafted to suggest vigor and vitality. The drug’s development is a classic case of serendipity in pharmacology; originally investigated by Pfizer in the early 1990s as a treatment for angina, its notable side effect of inducing erections led to its repositioning as a groundbreaking treatment for erectile dysfunction (ED).101 - Strategic Patenting and Lifecycle Management: Pfizer employed a sophisticated intellectual property strategy to maximize Viagra’s market life. The company secured two distinct U.S. patents for the same compound: one covering its cardiovascular use (marketed as Revatio), which expired in 2012, and a second, more critical patent covering its use for ED, which was extended to April 2020 through pediatric testing provisions.101 This layering of patents is a form of “evergreening” designed to prolong market exclusivity.
- Managed Generic Entry: Rather than facing an abrupt patent cliff, Pfizer orchestrated a controlled descent. Through strategic litigation and subsequent settlement agreements with generic manufacturers Teva and Mylan, Pfizer allowed for a managed entry of generic sildenafil in December 2017, more than two years before the patent’s final expiration. The terms of the settlement required the generic companies to pay Pfizer a royalty for a license to market their products.101 In a concurrent and decisive move, Pfizer launched its own “authorized generic” through its subsidiary, Greenstone. This allowed Pfizer to compete directly with the new generics on price, capture a significant portion of the generic market for itself, and effectively dilute the 180-day market exclusivity period granted to the first generic filer. This case study is a masterclass in how proactive legal and commercial strategies can transform a patent cliff into a managed and more profitable transition.
Fluoxetine (Prozac): The Birth of Modern Pharmaceutical Branding
- Nomenclature and Cultural Impact: The generic name fluoxetine contains the -oxetine stem, used for a class of antidepressants structurally related to it.33 However, it was the brand name,
Prozac, that revolutionized pharmaceutical marketing. Developed by Eli Lilly in 1972 and approved in 1987, fluoxetine was the first major selective serotonin reuptake inhibitor (SSRI).103 In a departure from tradition, Lilly hired a branding agency to create the name. The name
Prozac was chosen to sound “positive and professional and zappy,” deliberately avoiding any direct reference to the drug’s chemical nature or the condition it treated.104 This, combined with an unprecedented direct-to-consumer marketing campaign, transformed Prozac from a mere medication into a cultural icon and the first blockbuster antidepressant. - Patent Litigation and Generic Entry: Eli Lilly’s market dominance was cut short by a surprise court ruling in 2000 that invalidated a key patent, abruptly moving the U.S. patent expiration date from 2003 to August 2001.107 This decision triggered a rapid influx of generic competition from multiple manufacturers, including Barr Laboratories, which was granted 180-day exclusivity for the most common 20 mg dosage form.108 Within the first three weeks of generic availability, Prozac’s share of new prescriptions plummeted from nearly 22% to under 8%.108 The case of Prozac starkly illustrates the immense financial stakes of patent litigation and the swift and dramatic impact that generic entry can have on a brand-name drug’s market share and revenue.
Section 10: The Future of Pharmaceutical Nomenclature
The landscape of pharmaceutical development is undergoing a profound transformation, driven by advances in genomics, biotechnology, and data science. As therapeutics become more complex and personalized, the established systems of drug nomenclature face unprecedented challenges and will require continuous evolution to remain fit for purpose.
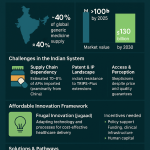
Persistent Challenges in Global Harmonization
Despite decades of effort, achieving complete global harmonization of drug nomenclature remains an elusive goal. The ongoing international debate over the naming of biosimilars is the most salient example of this challenge.87 The divergence between the U.S. FDA’s suffix-based system and the approach favored by the EMA and WHO highlights fundamental differences in regulatory philosophy and priorities.88 Beyond this high-profile issue, numerous other hurdles persist, including differing national regulatory frameworks, varying public health needs, and the practical difficulties of updating legacy healthcare IT systems and clinical practices to accommodate new naming conventions.109 The globalization of the pharmaceutical supply chain, where nearly 40% of U.S. drug products and 80% of active ingredients originate from over 150 countries, makes the need for robust, harmonized standards more critical than ever.112
The Impact of Personalized Medicine and Pharmacogenomics
The rise of personalized medicine and pharmacogenomics—the study of how an individual’s genes affect their response to drugs—presents a conceptual challenge to the very idea of a single nonproprietary name.113 The traditional model is based on a single active ingredient intended for a broad population. However, personalized medicine aims to tailor treatments to individuals or small subgroups based on their specific genetic makeup or disease biomarkers.114
As this field matures, we may see the development of therapies that are effective only in patients with a specific genetic variant. This raises complex questions for nomenclature. Should the nonproprietary name itself incorporate information about the relevant biomarker or genetic target? Will a single stem be sufficient to classify a drug that may have different effects in different genetic populations? The future of nomenclature may need to move beyond a single identifier for an active ingredient and toward more complex, multi-component names that capture the relationship between a drug and its specific biological target, a trend already visible in the two-word names for cell and gene therapies.117
Emerging Trends and Increasing Complexity
The future of drug naming will be shaped by several intersecting trends that increase its complexity and importance.
- The Crowded Lexicon: The number of approved drugs continues to grow each year. This expansion means that the available “white space” for creating new names that are unique, memorable, non-confusing, and marketable is rapidly shrinking.119 The process of naming a new drug is already a multi-year endeavor that can involve generating hundreds of candidates to find one that can successfully navigate the gauntlet of regulatory, trademark, and linguistic checks.20 This increasing difficulty will likely lead to greater reliance on computational linguistics, algorithms, and artificial intelligence to generate and screen potential names.119
- Evolving Brand Strategies: Branding strategies are also evolving. A notable trend is the move toward “Pharma 2.0” names—brand names that sound more scientific and are often derived from the drug’s generic name or mechanism of action (e.g., Tykerb, from its classification as a tyrosine kinase inhibitor).124 This represents a shift away from purely aspirational or abstract names and toward names that seek to inspire confidence by embracing the underlying science.
- A Living Language: Ultimately, the pharmaceutical alphabet is not a static set of rules but a living language that must adapt to reflect the progress of science.46 The creation of new stems, such as
-tinib for the class of tyrosine kinase inhibitors, and the development of entirely new naming schemes for cell and gene therapies, are testaments to the system’s capacity for evolution. As our understanding of disease becomes more granular and our therapeutic tools more sophisticated, the nomenclature used to describe them will need to become equally nuanced and precise.
Conclusion
The system of nonproprietary drug nomenclature, though often overlooked, is a critical pillar of global health. This report has demonstrated that a generic name is not an arbitrary label but a carefully constructed piece of a universal language, forged through a complex, multi-stakeholder process designed to balance the imperatives of pharmaceutical innovation, public access to affordable medicine, and, above all, patient safety. The collaborative efforts of the WHO’s INN Programme and the USAN Council have created a remarkably harmonized global system, providing a foundation for clear communication among clinicians, researchers, and regulators worldwide. The stem system, the linguistic core of this nomenclature, functions as an elegant and powerful cognitive tool, embedding essential pharmacological information directly into a drug’s name to facilitate safer and more efficient clinical decision-making.
Despite the system’s successes, patient safety remains the central and most pressing challenge. The persistence of Look-Alike, Sound-Alike (SALA) medication errors underscores that nomenclature exists within a complex clinical ecosystem. Preventing these errors requires more than just careful name selection; it demands a multi-layered, systemic approach that integrates technological safeguards like barcode scanning, standardized clinical practices, and the vigilant oversight of healthcare professionals, particularly pharmacists, who serve as the final line of defense.
Looking forward, the pharmaceutical alphabet is at an inflection point. The advent of biologics, biosimilars, and personalized medicine is pushing the boundaries of traditional naming conventions, forcing an evolution toward more descriptive and complex nomenclature. The ongoing international debate over biosimilar naming highlights the challenges of achieving global consensus in the face of differing regulatory philosophies. As medicine advances into an era of therapies tailored to an individual’s genetic code, the very concept of a single “generic” name will be tested. The future of drug naming will demand unprecedented levels of international collaboration, regulatory agility, and linguistic innovation to ensure that this vital public health infrastructure continues to serve its ultimate purpose: to clearly, accurately, and safely identify every medicine for the benefit of every patient.
Works cited
- Guidance on INN – Health products policy and standards, accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn/guidance-on-inn
- International nonproprietary name – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/International_nonproprietary_name
- United States Adopted Name – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/United_States_Adopted_Name
- Overview of Generic Drugs and Drug Naming – Drugs – Merck Manual Consumer Version, accessed August 1, 2025, https://www.merckmanuals.com/home/drugs/brand-name-and-generic-drugs/overview-of-generic-drugs-and-drug-naming
- Procedure for USAN name selection – American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/procedure-usan-name-selection
- Established Names – FDA, accessed August 1, 2025, https://www.fda.gov/media/70119/download
- Generic Drugs: Questions & Answers – FDA, accessed August 1, 2025, https://www.fda.gov/drugs/frequently-asked-questions-popular-topics/generic-drugs-questions-answers
- Generic vs. Brand-Name Drugs: What’s the Difference? – Humana, accessed August 1, 2025, https://www.humana.com/pharmacy/medication-information/difference-between-generic-and-brand-drug
- Generic vs. Brand-Name Drugs: Is There a Difference? | University Hospitals, accessed August 1, 2025, https://www.uhhospitals.org/blog/articles/2022/07/generic-vs-brand-name-drugs-is-there-a-difference
- www.uhhospitals.org, accessed August 1, 2025, https://www.uhhospitals.org/blog/articles/2022/07/generic-vs-brand-name-drugs-is-there-a-difference#:~:text=They%20look%20different.,%2C%20colors%2C%20flavors%20and%20preservatives.
- Generic Versus Brand Medications | Brown University Health, accessed August 1, 2025, https://www.brownhealth.org/be-well/generic-versus-brand-medications
- Generic Drug Facts | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/generic-drugs/generic-drug-facts
- Expanding the Use of Generic Drugs – HHS ASPE, accessed August 1, 2025, https://aspe.hhs.gov/reports/expanding-use-generic-drugs-0
- International Nonproprietary Names (INN) for novel vaccine substances: A matter of safety, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8625196/
- International Nonproprietary Names (INN) – Drugs.com, accessed August 1, 2025, https://www.drugs.com/inn.html
- INN Online Application, accessed August 1, 2025, https://extranet.who.int/tools/inn_online_application/
- INN selection process – Health products policy and standards, accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn/selection
- Know the Pharma Basics: INN and USAN – Red Sneakers Blog, accessed August 1, 2025, https://redsneakersblog.com/2017/04/22/know-pharma-basics-inn/
- INN Schemes – Health products policy and standards, accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn/inn-schemas
- Ever Wonder How Drugs Are Named? Read On – Pfizer, accessed August 1, 2025, https://www.pfizer.com/news/articles/ever_wonder_how_drugs_are_named_read_on
- International Nonproprietary Names for Pharmaceutical Substances (INN) – Fimea, accessed August 1, 2025, https://fimea.fi/en/supervision/legislation/european_pharmacopoeia/international-non-proprietary-names-for-pharmaceutical-substances-inn-
- Protection of USAN & INN Stems – American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/protection-usan-inn-stems
- International Nonproprietary Names Programme and Classification of Medical Products – World Health Organization (WHO), accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn
- International Nonproprietary Names from WHO Added to the Global Brand Database – WIPO, accessed August 1, 2025, https://www.wipo.int/en/web/global-brand-database/w/news/2019/news_0001
- Pat-INFORMED – The Gateway to Medicine Patent Information – WIPO, accessed August 1, 2025, https://www.wipo.int/pat-informed/en/
- How Do Drugs Get Named? | Journal of Ethics | American Medical Association, accessed August 1, 2025, https://journalofethics.ama-assn.org/article/how-do-drugs-get-named/2019-08
- United States Adopted Names (USAN), accessed August 1, 2025, https://www.oit.va.gov/Services/TRM/StandardPage.aspx?tid=5231
- USAN Council | American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/usan-council
- Drug Product Nomenclature – FDA, accessed August 1, 2025, https://www.fda.gov/media/134015/download
- United States adopted name (USAN) – PMLiVE, accessed August 1, 2025, https://pmlive.com/healthcare_glossary/terms/u/united_states_adopted_name_usan/
- United States Adopted Names approved stems – American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/united-states-adopted-names-approved-stems
- Common Drug Stems, accessed August 1, 2025, https://learning.medicine.wsu.edu/wp-content/uploads/sites/4/2024/01/Common-Drug-Stems.pdf
- Pharmacology Cheat Sheet: Generic Drug Stems – Nurseslabs, accessed August 1, 2025, https://nurseslabs.com/common-generic-drug-stem-cheat-sheet/
- 29.5. International Non-Proprietary Names (generic names for pharmaceutical substances) and INN stems | IPA Manuals, accessed August 1, 2025, http://manuals.ipaustralia.gov.au/trademark/international-non-proprietary-names-generic-names-for-pharmaceutical-substances-and-inn-stems
- Guidelines released on USAN naming, accessed August 1, 2025, https://gabionline.net/guidelines/Guidelines-released-on-USAN-naming
- A Morphological Study of Drug Brand Names – The UNH Scholars Repository, accessed August 1, 2025, https://scholars.unh.edu/cgi/viewcontent.cgi?article=1103&context=honors
- Drug nomenclature – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Drug_nomenclature
- INN stems – World Health Organization (WHO), accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn/stembook
- USAN STEM LIST, accessed August 1, 2025, https://farmamol.web.uah.es/drug-naming_stem-list-cumulative.pdf
- Common Stems for International Nonproprietary Names (INNs …, accessed August 1, 2025, https://www.drugs.com/inn-stems.html
- Common Drug Name Stems Cheat Sheet – ADL Data Systems, accessed August 1, 2025, https://www.adldata.org/wp-content/uploads/2015/07/CommonDrugStemsCheatSheet.pdf
- Table 1.8, [Common Classes of Medications, Examples, Suffixes, and Roots]. – Nursing Pharmacology – NCBI Bookshelf, accessed August 1, 2025, https://www.ncbi.nlm.nih.gov/books/NBK595006/table/ch1pharma.T.common_classes_of_medication/
- Usan Stem List | PDF – Scribd, accessed August 1, 2025, https://www.scribd.com/doc/236650700/Usan-Stem-List
- Drug Prefix, Root, and Suffix – Denali Rx, accessed August 1, 2025, https://denalirx.com/drug-prefix-root-and-suffix/
- 29. Annex A1 – Table of INN stems – IPA Manuals, accessed August 1, 2025, http://manuals.ipaustralia.gov.au/trademark/annex-a1—table-of-inn-stems
- What’s in a Name? Drug Nomenclature and Medicinal Chemistry Trends using INN Publications – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8154580/
- What is INN a Name? – The Antibody Society, accessed August 1, 2025, https://www.antibodysociety.org/antibody-engineering-therapeutics/what-is-inn-a-name/
- LASA Medications: a vulnerability for the patient safety – Cirrus, accessed August 1, 2025, https://www.getcirrus.com/en-blog/lasa-medications-a-vulnerability-for-the-patient-safety
- Medication safety for look-alike, sound-alike medicines – IRIS, accessed August 1, 2025, https://iris.who.int/bitstream/handle/10665/373495/9789240058897-eng.pdf?sequence=1
- Medication Errors Linked to Drug Name Confusion Advisory, accessed August 1, 2025, https://patientsafety.pa.gov/ADVISORIES/Pages/200412_07.aspx
- Cognitive tests predict real-world errors: the relationship between drug name confusion rates in laboratory-based memory and perception tests and corresponding error rates in large pharmacy chains – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC5530327/
- Automated detection of wrong-drug prescribing errors | BMJ Quality & Safety, accessed August 1, 2025, https://qualitysafety.bmj.com/content/28/11/908
- Chapter 6. The Role of Drug Names in Medication Errors – PharmacyLibrary, accessed August 1, 2025, https://pharmacylibrary.com/doi/10.21019/9781582120928.ch6
- Medication Errors | AMCP.org, accessed August 1, 2025, https://www.amcp.org/concepts-managed-care-pharmacy/medication-errors
- Case report of a medication error by look-alike packaging: a classic surrogate marker of an unsafe system – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4357082/
- Look-alike, sound-alike medication errors: a novel case concerning a S | IMCRJ, accessed August 1, 2025, https://www.dovepress.com/look-alike-sound-alike-medication-errors-a-novel-case-concerning-a-slo-peer-reviewed-fulltext-article-IMCRJ
- Look‐alikes, sound‐alikes: Three cases of insidious medication errors – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7752431/
- ISMP’s List of Confused Drug Names, accessed August 1, 2025, https://www.ismp.org/sites/default/files/attachments/2017-11/confuseddrugnames%2802.2015%29.pdf
- ISMP’s List of Confused Drug Names. | PSNet, accessed August 1, 2025, https://psnet.ahrq.gov/issue/ismps-list-confused-drug-names
- ISMP Guidance and Tools – ECRI, accessed August 1, 2025, https://home.ecri.org/blogs/ismp-resources
- FDA and ISMP Lists of Look-Alike Drug Names with Recommended Tall Man (Mixed Case) Letters – ECRI, accessed August 1, 2025, https://online.ecri.org/hubfs/ISMP/Resources/ISMP_Look-Alike_Tallman_Letters.pdf
- List of Confused Drug Names – ECRI, accessed August 1, 2025, https://home.ecri.org/blogs/ismp-resources/list-of-confused-drug-names
- Medication Errors Related to CDER-Regulated Drug Products – FDA, accessed August 1, 2025, https://www.fda.gov/drugs/drug-safety-and-availability/medication-errors-related-cder-regulated-drug-products
- Drug Name Review | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/fda-drug-info-rounds-video/drug-name-review
- Characteristics That May Help in the Identification of Potentially Confusing Proprietary Drug Names, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7238771/
- FDA In Brief: FDA Provides Guidances On Proprietary Naming for Drugs, Changes to Naming Analysis Program, accessed August 1, 2025, https://www.fda.gov/news-events/fda-brief/fda-brief-fda-provides-guidances-proprietary-naming-drugs-changes-naming-analysis-program
- Tall Man lettering – Wikipedia, accessed August 1, 2025, https://en.wikipedia.org/wiki/Tall_Man_lettering
- Medication Errors Related to Look-Alike, Sound-Alike Drugs—How …, accessed August 1, 2025, https://www.apsf.org/article/medication-errors-related-to-look-alike-sound-alike-drugs-how-big-is-the-problem-and-what-progress-is-being-made/
- Tall Man Letters Are Gaining Wide Acceptance – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3351881/
- FDA and ISMP Lists of Look-Alike Drug Names with Recommended Tall Man Letters, accessed August 1, 2025, https://www.ismp.org/sites/default/files/attachments/2017-11/tallmanletters.pdf
- A systematic literature review of LASA error interventions – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC9328434/
- Drug Name Confusions – Pharmacy Times, accessed August 1, 2025, https://www.pharmacytimes.com/view/drug-name-confusions
- Preventing dispensing errors by alerting for drug confusions in the pharmacy information system—A survey of users | PLOS One – Research journals, accessed August 1, 2025, https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197469
- Adopt Strategies to Manage Look-Alike and/or Sound-Alike Medication Name Mix-Ups, accessed August 1, 2025, https://home.ecri.org/blogs/ismp-alerts-and-articles-library/adopt-strategies-to-manage-look-alike-and-or-sound-alike-medication-name-mix-ups
- Perilous effct of sala drugs – rootcause assessment and intimidation, accessed August 1, 2025, https://www.wisdomlib.org/health-sciences/journal/world-journal-of-pharmaceutical-research/d/doc1365550.html
- Medication Dispensing Errors and Prevention – StatPearls – NCBI Bookshelf, accessed August 1, 2025, https://www.ncbi.nlm.nih.gov/books/NBK519065/
- Pharmacist’s Role in Medication Safety | PSNet, accessed August 1, 2025, https://psnet.ahrq.gov/primer/pharmacists-role-medication-safety
- ASHP Guidelines on Preventing Medication Errors in Hospitals, accessed August 1, 2025, https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/preventing-medication-errors-hospitals.ashx
- Reducing Errors from LASA Medication Names | FDB (First Databank), accessed August 1, 2025, https://www.fdbhealth.com/insights/articles/2018-10-04-reducing-errors-from-look-alike-sound-alike-medication-names-the-role-of-indications
- Safety Tips to Prevent Look- Alike Sound-Alike (LASA) Eye and Ear Drug Errors – New York Eye and Ear Infirmary, accessed August 1, 2025, https://www.nyee.edu/files/Patient%20Care/Patient%20Resources/Safety%20Tips%20to%20Prevent%20Look-Alike%20Sound-/safety-tips.pdf
- Biosimilar Naming Conventions: Pharmacist Perceptions and Impact on Confidence in Dispensing Biologics – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10398106/
- Naming Convention, Interchangeability, and Patient Interest in …, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7428664/
- It’s All in the Name: Updated FDA Guidance on Nonproprietary …, accessed August 1, 2025, https://www.haynesboone.com/news/alerts/its-all-in-the-name
- Nonproprietary Naming of Biological Products Guidance for Industry | FDA, accessed August 1, 2025, https://www.fda.gov/files/drugs/published/Nonproprietary-Naming-of-Biological-Products-Guidance-for-Industry.pdf
- Updated FDA Labeling Recommendations for Biosimilar and Interchangeable Biosimilar Products | FDA, accessed August 1, 2025, https://www.fda.gov/drugs/our-perspective/updated-fda-labeling-recommendations-biosimilar-and-interchangeable-biosimilar-products
- The Name Game – The FDA Issues Draft Guidance of Biologics Naming, accessed August 1, 2025, https://www.crowell.com/en/insights/client-alerts/the-name-game-the-fda-issues-draft-guidance-of-biologics-naming
- Global Harmonization Is Not All That Global: Divergent Approaches in Drug Safety, accessed August 1, 2025, https://www.insideeulifesciences.com/2008/08/01/global-harmonization-is-not-all-that-global-divergent-approaches-in-drug-safety/
- The Naming of Biosimilar Medicines Worldwide Should Promote Patient Safety and Prescriber Confidence, accessed August 1, 2025, https://biosimilarscouncil.org/resource/the-naming-of-biosimilar-medicines-worldwide-should-promote-patient-safety-and-prescriber-confidence/
- Debate Continues Around Biosimilar Naming Conventions – Pharmacy Times, accessed August 1, 2025, https://www.pharmacytimes.com/view/debate-continues-around-biosimilar-naming-conventions
- FTC Criticizes FDA’s Proposed Biosimilar Naming Rules | Insights & Resources – Goodwin, accessed August 1, 2025, https://www.goodwinlaw.com/en/insights/blogs/2015/10/ftc-criticizes-fdas-proposed-biosimilar-naming-rul
- Gene Therapy Naming Scheme | American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/gene-therapy-naming-scheme
- Genetically Modified Cell-based Therapy Naming Scheme | American Medical Association, accessed August 1, 2025, https://www.ama-assn.org/about/united-states-adopted-names-usan/genetically-modified-cell-based-therapy-naming-scheme
- Health products policy and standards, accessed August 1, 2025, https://www.who.int/teams/health-product-and-policy-standards/inn/inn-bio/inn-bio-ct
- Lipitor – Wiktionary, the free dictionary, accessed August 1, 2025, https://en.wiktionary.org/wiki/Lipitor
- atorvastatin – Wiktionary, the free dictionary, accessed August 1, 2025, https://en.wiktionary.org/wiki/atorvastatin
- When does the patent for Atorvastatin expire? – Patsnap Synapse, accessed August 1, 2025, https://synapse.patsnap.com/article/when-does-the-patent-for-atorvastatin-expire
- Lipitor History and Information – DrugClaim.com, accessed August 1, 2025, https://drugclaim.com/lipitor-history/
- Lipitor Patent Expires | The Scientist, accessed August 1, 2025, https://www.the-scientist.com/lipitor-patent-expires-41658
- “For Me There Is No Substitute”: Authenticity, Uniqueness, and the Lessons of Lipitor, accessed August 1, 2025, https://journalofethics.ama-assn.org/article/me-there-no-substitute-authenticity-uniqueness-and-lessons-lipitor/2010-10
- How are generic drugs named? – The Grammarphobia Blog, accessed August 1, 2025, https://www.grammarphobia.com/blog/2019/08/generic-drug-names.html
- Viagra’s Generic Cliff: Why It Wasn’t a Free-for-All – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/viagra-a-complicated-case-study-of-generic-drug-market-entry-in-the-united-states/
- Sildenafil: from angina to erectile dysfunction to pulmonary hypertension and beyond – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7097805/
- Generic Medications – MGH Center for Women’s Mental Health, accessed August 1, 2025, https://womensmentalhealth.org/posts/generic-medications/
- FDA Approves Prozac as an Antidepressant | EBSCO Research Starters, accessed August 1, 2025, https://www.ebsco.com/research-starters/health-and-medicine/fda-approves-prozac-antidepressant
- The creation of the Prozac myth | Mental health – The Guardian, accessed August 1, 2025, https://www.theguardian.com/society/2008/feb/27/mentalhealth.health1
- The Truth About Fluoxetine – Alternative to Meds Center, accessed August 1, 2025, https://www.alternativetomeds.com/blog/the-controversial-history-of-fluoxetine-the-active-ingredient-in-prozac/
- Prozac patent loss sends drug shares down | Business – The Guardian, accessed August 1, 2025, https://www.theguardian.com/business/2000/aug/11/mondaymediasection.media
- Prozac patent expires making room for generic – Houston – Chron, accessed August 1, 2025, https://www.chron.com/business/article/prozac-patent-expires-making-room-for-generic-2032943.php
- Current Challenges in Labelling for Generic Medicinal Products: Company Core Data Sheet (CCDS) Development and Maintenance – PMC – PubMed Central, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7744299/
- International Harmonization of Expedited Programs: Challenges and Opportunities for Increasing Patient Access to Innovative Therapies – Duke-Margolis Institute for Health Policy, accessed August 1, 2025, https://healthpolicy.duke.edu/events/international-harmonization-expedited-programs-challenges-and-opportunities-increasing
- Tactics and Strategies for a Way Forward – International Regulatory Harmonization Amid Globalization of Drug Development – NCBI, accessed August 1, 2025, https://www.ncbi.nlm.nih.gov/books/NBK174228/
- From Regulatory Convergence to Global Regulatory Harmonization – Pharma’s Almanac, accessed August 1, 2025, https://www.pharmasalmanac.com/articles/from-regulatory-convergence-to-global-regulatory-harmonization
- Personalized Medicine and the Future of Pharmacogenomics, accessed August 1, 2025, https://pharmacy.wsu.edu/2022/02/11/personalized-medicine-and-the-future-of-pharmacogenomics/
- Personalized Medicine Market: Trends, Insights, and Future Projections (2024-2035), accessed August 1, 2025, https://www.pharmiweb.com/press-release/2025-03-04/personalized-medicine-market-trends-insights-and-future-projections-2024-2035
- Personalized medicine is taking over. Here’s how companies can navigate the future, accessed August 1, 2025, https://business.gmu.edu/news/2023-05/personalized-medicine-taking-over-heres-how-companies-can-navigate-future
- Personalized Medicine – Future Impact, Pharma Industry Perspective – PMC, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC2918032/
- Current Status, Issues and Future Prospects of Personalized Medicine for Each Disease, accessed August 1, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8949099/
- The Future of Personalized Medicine: How AI and Pharmacogenomics Are Changing Drug Development – The Eleight, accessed August 1, 2025, https://lhseleight.wordpress.com/2025/04/02/the-future-of-personalized-medicine-how-ai-and-pharmacogenomics-are-changing-drug-development/
- Why Do Prescription Drugs Have Such Crazy Names? | Global …, accessed August 1, 2025, https://globalhealthnow.org/2024-07/why-do-prescription-drugs-have-such-crazy-names
- What’s in a name: Agencies struggle to keep up with new drug names, accessed August 1, 2025, https://pharma.nridigital.com/pharma_dec23/whats-in-a-name-agencies-struggle-to-keep-up-with-expanding-drug-space
- Press Room – Brand Institute, accessed August 1, 2025, https://brandinstitute.com/press-room/
- How Are New Drugs Named? The Process Explained!, accessed August 1, 2025, https://absoluteawakenings.com/how-are-new-drugs-named-the-process-explained/
- The Comprehensive Science and Art of Pharmaceutical Drug Naming – DrugPatentWatch, accessed August 1, 2025, https://www.drugpatentwatch.com/blog/the-comprehensive-science-and-art-of-pharmaceutical-drug-naming/
- IP for Business: The Fall and Rise of Pharma Brand Names – WIPO, accessed August 1, 2025, https://www.wipo.int/web/wipo-magazine/articles/ip-for-business-the-fall-and-rise-of-pharma-brand-names-36258
- What’s in a Name? Drug Nomenclature and Medicinal Chemistry Trends using INN Publications, accessed August 1, 2025, https://pubs.acs.org/doi/10.1021/acs.jmedchem.1c00181