The pharmaceutical industry stands at a historic inflection point. For decades, it has operated on a simple, wildly profitable playbook: develop a “blockbuster” drug for a common condition, secure ironclad patent protection, and deploy a massive sales force to drive prescriptions toward multi-billion-dollar revenues. This model was the economic engine of modern medicine, a seemingly perpetual motion machine where the profits from one generation of blockbusters funded the research and development (R&D) for the next. But that engine is sputtering, and the entire industry is bracing for the impact.
The blockbuster model is not just aging; it is fundamentally broken. The low-hanging fruit of drug discovery for mass-market conditions like hypertension and high cholesterol has been picked. Payers, from governments to private insurers, are balking at premium prices for incrementally better drugs, and the very definition of success is being questioned. The once-vaunted $1 billion annual sales benchmark, which defined the blockbuster era, has been so devalued by market inflation and soaring development costs that it no longer signifies elite performance. According to analysis from IQVIA, a “true blockbuster” in today’s market needs to generate over $3 billion in annual sales, a threshold met by only 45 products in 2022, compared to the 188 that met the traditional definition.
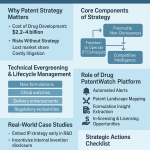
This creates a central paradox: pharmaceutical companies are more dependent than ever on the colossal cash flows from their top products to fund increasingly expensive R&D—now averaging $2.3 billion per new drug—yet the strategic path to creating those products has been all but obliterated.1 This pressure cooker environment has given rise to an “innovation paradox,” where the desperate need to replace outgoing revenue can stifle true, high-risk, high-reward breakthroughs. With an effective patent life often compressed to just 7-12 years after a grueling 12-13 year development cycle, the focus shifts to maximizing returns through safer, “me-too” drugs or defensive “evergreening” strategies rather than pursuing revolutionary science.4
Now, this strained model is about to be shattered by an external force of unprecedented scale: the 2025-2030 patent cliff. This is not just another wave of expirations; it is a seismic event that threatens to wipe out over $200 billion in annual revenue, forcing a painful and existential reckoning.5 The question is no longer
if the industry will change, but how. As the fizzle of the blockbuster era grows louder, the industry is looking warily—and with a mix of hope and trepidation—to the next big thing. This report will dissect the anatomy of this crisis and provide an exhaustive analysis of the new arsenal of technologies—from artificial intelligence and personalized medicine to antibody-drug conjugates and “living drugs”—that will not just replace lost revenue, but fundamentally redefine the future of medicine.
Part 1: The $200 Billion Precipice – Anatomy of the Looming Patent Cliff
Decoding the 2025-2030 Patent Cliff: A Storm of Unprecedented Scale
The term “patent cliff” is an industry colloquialism, but one that aptly captures the phenomenon: a sharp, sudden, and often catastrophic decline in revenue that a company experiences when a blockbuster drug loses its shield of exclusivity. As patents expire, the floodgates open for generic and biosimilar competitors, which can capture the market with breathtaking speed. It is not uncommon for a blockbuster’s revenue to plummet by 80-90% within the first year of generic entry, turning a reliable stream of billions into a mere trickle.5
What makes the coming cliff so perilous is its sheer financial magnitude. Analyst firm William Blair estimates that from 2023 through the end of 2025 alone, nearly 50 products will lose patent protection, eroding their aggregate sales from $162.8 billion in 2025 to just $67 billion by 2029. Widening the lens, the picture becomes even more stark. According to data and analytics firm GlobalData, the U.S. market is set to lose over $230 billion between 2025 and 2030. Other industry projections place the total annual revenue at risk from patent expirations between 2025 and 2030 at a colossal $236 billion. This is, by any measure, one of the most financially significant patent cliffs the industry has faced in over a decade, forcing companies to aggressively rethink their entire corporate strategy.6
This is not a generalized, industry-wide problem that affects all players equally. The pain will be concentrated among a handful of pharmaceutical giants whose fortunes have been built on the success of a few key products. According to one report, the impending losses will affect assets that accounted for more than 30% of the collective 2024 revenues from Bristol Myers Squibb, Pfizer, AstraZeneca, Novartis, and Regeneron. Another analysis suggests that for companies like BMS, Pfizer, and Novartis, the revenue generated by their top five drugs is set to decrease by as much as 62% by 2030.
The “death row” of blockbusters facing this cliff reads like a who’s who of modern medicine:
- Merck’s Keytruda (pembrolizumab): Perhaps the most talked-about expiration on the horizon, Keytruda is one of the industry’s highest-earning assets, a revolutionary cancer immunotherapy that brought in over $29 billion in 2024. Its primary patent is set to expire in 2028, creating a massive revenue hole that the company is scrambling to fill. Merck also faces headwinds for its cancer drug Lenvima (2025), diabetes drugs Januvia and Janumet (2026), and another cancer therapy, Lynparza (2027).9
- Bristol Myers Squibb’s Eliquis (apixaban) and Opdivo (nivolumab): BMS is arguably the company in the hottest seat. It faces a double whammy with two of its biggest products. Eliquis, a blockbuster anticoagulant co-marketed with Pfizer that generated over $13 billion for BMS in 2024, faces loss of exclusivity around 2026-2028.5 At the same time, its flagship immunotherapy Opdivo faces its own cliff in 2028. To compound the pressure, another cancer therapy, Yervoy, which brought in $2.5 billion in 2024, faces generic competition this year.
- AstraZeneca’s Farxiga (dapagliflozin): A cornerstone of the company’s portfolio, this SGLT2 inhibitor for diabetes and heart failure pulled in $7.7 billion in 2024. It faces the loss of key patent protections this year, representing a significant threat to AstraZeneca’s ambitious goal of reaching $80 billion in annual revenue by 2030.9 Its rare disease drug Soliris, with nearly $2.6 billion in 2024 sales, is also expected to face biosimilar challenges this year.9
- Novartis’s Entresto (sacubitril/valsartan): This crucial heart failure medication, which earned $7.8 billion for Novartis last year, is set to lose market exclusivity in July 2025, escalating the company’s patent problems.9
- Johnson & Johnson’s Stelara (ustekinumab): A key immunology moneymaker with $6.72 billion in U.S. sales in 2024, Stelara is already grappling with the launch of its first biosimilar competitor, with more on the way. The company also faces the expiration of its cancer drug Darzalex by 2029.6
The table below provides a stark visualization of the financial precipice, moving the patent cliff from an abstract threat to a concrete, quantifiable risk for specific corporate balance sheets. It is this reality that is forcing the dramatic strategic pivots we are now witnessing across the industry.
| Drug Name (Brand) | Innovator Company | Primary Indication | 2024 Revenue (approx.) | Expected U.S. LOE | Sources |
| Keytruda (pembrolizumab) | Merck | Cancer (Immunotherapy) | >$29 Billion | 2028 | 6 |
| Eliquis (apixaban) | Bristol Myers Squibb / Pfizer | Anticoagulant | >$20 Billion (Combined) | 2026-2028 | 6 |
| Opdivo (nivolumab) | Bristol Myers Squibb | Cancer (Immunotherapy) | ~$9 Billion | 2028 | 6 |
| Entresto (sacubitril/valsartan) | Novartis | Heart Failure | $7.8 Billion | 2025 | 9 |
| Farxiga (dapagliflozin) | AstraZeneca | Diabetes / Heart Failure | $7.7 Billion | 2025 | 9 |
| Stelara (ustekinumab) | Johnson & Johnson | Immunology | $6.72 Billion (U.S.) | 2025 (ongoing) | |
| Eylea (aflibercept) | Regeneron | Eye Disease | ~$6 Billion | 2025 (ongoing) | |
| Yervoy (ipilimumab) | Bristol Myers Squibb | Cancer (Immunotherapy) | $2.5 Billion | 2025 | |
| Soliris (eculizumab) | AstraZeneca | Rare Disease | $2.6 Billion | 2025 (ongoing) | 9 |
Corporate War Rooms: Immediate Strategies for Survival
Faced with this existential threat, pharmaceutical boardrooms and strategy teams have transformed into veritable war rooms. The responses have been swift, decisive, and revealing of divergent corporate philosophies under extreme pressure. Broadly, the immediate defensive strategies fall into three main categories: buying new assets, building from the internal pipeline, or cutting costs to the bone.
The most common and aggressive response has been to buy growth. The urgent need to replenish pipelines and fill looming revenue gaps has become a primary driver for a surge in mergers and acquisitions (M&A) and in-licensing deals.10 Companies are strategically acquiring promising therapies from early-stage biotechs to plug the holes in their portfolios.5 A notable example of this strategy in action was AbbVie’s pre-emptive $63 billion acquisition of Allergan in 2019, a move explicitly designed to brace for the eventual patent cliff of its megablockbuster, Humira. However, the current economic climate has introduced a new dynamic. While dealmaking remains crucial, there has been a noticeable shift toward greater selectivity. Companies are now focusing on fewer, but higher-value, early-stage opportunities and are increasingly sourcing de-risked, later-stage assets that promise a more immediate and certain return on investment.
The second strategy is to build from within. Companies fortunate enough to have a robust and innovative internal R&D pipeline are leaning heavily on it to weather the storm. AbbVie, having made its big “buy” move, is now relying on its new immunology stars, Skyrizi and Rinvoq, to patch the multi-billion-dollar hole left by Humira’s decline. AstraZeneca is similarly banking on its clinical pipeline, with its CFO calling 2025 an “unprecedented catalyst-rich period” for the company. But perhaps the most striking success story of the “build” strategy is Eli Lilly. By strengthening its pipeline with game-changing drugs, the company is not just surviving the patent cliff era but thriving, with a projected revenue boost of an astonishing 165% through 2030.
When buying or building isn’t a viable short-term option, the third, and most painful, strategy is to cut costs. This is the path of retrenchment, a defensive maneuver to preserve capital and weather the storm. The prime example of this approach is Bristol Myers Squibb. Facing the impending loss of both Eliquis and Opdivo, the company has chosen to navigate the turbulence not by aggressively acquiring new assets, but through a sweeping corporate realignment. In April 2024, BMS kicked off a program to save up to $1.5 billion by 2025, which included laying off around 2,200 employees. It has since tacked another $2 billion onto that cost-cutting goal. This is a high-risk gambit. While it shores up the balance sheet in the short term, deep cuts can cripple R&D capacity, damage employee morale, and potentially hamstring the company’s ability to innovate its way out of the crisis in the long run.
The varied reactions to the same external threat reveal a fascinating divergence in corporate philosophies. This is not simply a matter of different tactics; it reflects fundamental differences in risk tolerance, strategic vision, and the specific circumstances of each company. The path a company chooses is dictated by the health of its existing pipeline and the strength of its balance sheet. Eli Lilly, with a pipeline rich in potential blockbusters, can afford to bet on internal innovation. AbbVie, which had years to see the Humira cliff approaching, used its massive cash flow to make a transformative acquisition. BMS, on the other hand, facing the daunting prospect of losing two megablockbusters in quick succession, appears to have found itself in a position where deep, defensive cuts are its most immediate and viable option.6
This divergence sets the stage for a compelling natural experiment within the pharmaceutical industry. Over the next five to seven years, the market will render its verdict on which of these macro-strategies—Build, Buy, or Cut—proves most effective in navigating the crisis. Will BMS’s leaner structure make it an agile target for a future merger, or will it be left behind by more innovative peers? Will Eli Lilly’s R&D-heavy bet continue to pay off, or will an unexpected pipeline setback expose its vulnerability? For investors, strategists, and smaller biotech companies, tracking these divergent paths offers a real-time, high-stakes case study in corporate crisis management and signals a wealth of opportunities, whether for acquisition, partnership, or out-maneuvering a distracted giant.
Part 2: The Dawn of a New Age – Charting the Course for Next-Generation Therapeutics
The New Arsenal: An Overview of Transformative Technologies
The patent cliff is more than a financial crisis; it is a powerful catalyst, forcing the pharmaceutical industry to abandon its comfortable, chemistry-based past and embrace a future defined by complex biology, data science, and unprecedented therapeutic innovation. The “next big thing” is not a single drug or technology but a diverse and powerful arsenal of new platforms poised to revolutionize how we treat disease. This is not an incremental evolution; it is a paradigm shift.
The scale of this transformation is reflected in the explosive growth of the global biotechnology market, which is projected to surge from an estimated $1.7 trillion in 2025 to a staggering $5.85 trillion by 2034, expanding at a compound annual growth rate (CAGR) of over 13%.17 This growth is being fueled by a convergence of scientific breakthroughs that are moving from the realm of science fiction to clinical reality.
The key pillars of this new era include:
- Artificial Intelligence (AI): Moving from a niche tool to a foundational infrastructure for discovering and developing drugs at a speed and precision previously unimaginable.
- Personalized Medicine: The definitive end of the “one-size-fits-all” approach, using genomics and biomarkers to tailor treatments to the individual patient.20
- Advanced Targeted Therapies: The rise of “smart chemotherapy” like Antibody-Drug Conjugates (ADCs), which deliver potent toxins directly to cancer cells.
- RNA Therapeutics: Harnessing the power of messenger RNA (mRNA) not just for vaccines, but as a versatile tool for protein replacement and treating genetic diseases.19
- Cell and Gene Therapy (CGT): The most disruptive frontier, involving the engineering of “living drugs” like CAR-T cells and the revolutionary potential of CRISPR gene editing to offer one-time cures.20
These are not siloed technologies; they are deeply interconnected, often relying on each other to function. AI powers the data analysis for personalized medicine; mRNA is a key tool for delivering gene editing machinery; and ADCs represent a bridge between traditional and next-generation approaches. Together, they form the new strategic landscape that every pharmaceutical company must now navigate.
The AI Revolution in R&D: From In Silico to In Vivo
For decades, drug discovery has been a process of painstaking, trial-and-error experimentation in the lab. Today, that paradigm is being inverted by artificial intelligence. AI is rapidly moving from a promising but peripheral technology to a core, foundational infrastructure for the entire R&D process. It is being deployed across the value chain to accelerate discovery, de-risk development, and optimize clinical trials with a speed and scale that would have been impossible just a few years ago.19 The market reflects this tectonic shift: the AI in drug discovery sector is projected to grow from $6.93 billion in 2025 to $16.52 billion by 2034, a clear signal of its strategic importance.26
AI’s impact is perhaps most profound in the earliest stages of R&D, where it is fundamentally transforming the discovery and design funnel. By 2025, it is estimated that an incredible 30% of all new drugs will be discovered using AI.28 This is made possible by platforms like DeepMind’s AlphaFold, which has effectively solved the 50-year-old grand challenge of protein folding, allowing scientists to predict a protein’s 3D structure from its amino acid sequence with remarkable accuracy.20 This breakthrough provides unprecedented insight into disease mechanisms and accelerates the design of drugs that can precisely target these proteins.
Beyond understanding existing biology, AI is now creating it. Companies like Insilico Medicine are using generative AI to design completely novel molecules from scratch, tailored to specific disease targets. This in silico (computer-based) approach can slash drug discovery timelines and preclinical costs by 25-50%, allowing researchers to identify successful therapies earlier and abandon failing candidates with far less wasted investment.28
The revolution continues into the clinical trial phase, a notoriously long, expensive, and failure-prone stage of development. AI is being used to design smarter, more patient-centric trials that are both faster and more likely to succeed.19 AI algorithms can analyze vast datasets of electronic health records (EHRs) to identify and recruit the right patients for a trial with incredible speed and accuracy, a process automated by tools like TrialGPT. This not only accelerates recruitment—a common bottleneck—but also helps ensure greater diversity in trial populations. AI can also be used to design more efficient, adaptive trial protocols that can be adjusted in real-time based on incoming data, and even predict patient dropouts to prevent disruptions. The financial impact is staggering: AI-powered improvements in clinical trials have the potential to shorten trial durations by up to 50% and save the industry an estimated $26 billion annually.
This is not a theoretical future; it is happening now. The industry is rife with success stories and key players who are proving AI’s value:
- Insilico Medicine took the first fully AI-discovered and AI-designed drug for idiopathic pulmonary fibrosis (IPF) into Phase 2 clinical trials, a landmark achievement.31
- Atomwise famously used its AtomNet AI platform to scan millions of compounds and identify two potential drug candidates for the Ebola virus in less than a day, a process that would traditionally take years.
- Exscientia developed an AI-designed cancer drug that progressed from discovery to the start of clinical trials in just one year.
- Big Pharma has moved aggressively into the space. Pfizer integrated AI into the accelerated development of its COVID-19 treatment, Paxlovid, and has active partnerships with AI firms like Tempus and CytoReason. AstraZeneca is collaborating with BenevolentAI on treatments for chronic kidney disease. And Roche has established itself as a leader in AI adoption through both in-house innovation and strategic acquisitions.
The rise of AI is creating a profound shift in the competitive dynamics of the pharmaceutical industry. The advantage is no longer just about owning a patent on a molecule; it’s increasingly about owning the proprietary data and the sophisticated algorithms that can turn that data into drugs. Companies are not merely adopting off-the-shelf AI tools; they are building their own powerful, integrated platforms, such as Moderna’s generative AI application “mChat” or Janssen’s “Trials360.ai”.29
This creates a new “winner-take-most” dynamic. The logic is simple and powerful. First, high-quality, proprietary data is the fuel for any AI model. Large pharmaceutical companies, with their decades of accumulated clinical trial data, real-world evidence, and genomic information, possess a massive, defensible asset that is difficult for smaller players to replicate. Second, a company that develops a superior, proprietary algorithm—for instance, one that can predict drug toxicity or select the ideal patient population for a trial with higher accuracy—creates a durable competitive moat. This is a fundamental shift from a monopoly based on a patent to one based on data and algorithms. Finally, these platforms benefit from powerful network effects: the more they are used, the more data they generate, which in turn makes the AI models smarter, creating a virtuous cycle of improvement.
The long-term implication of this trend will be a widening of the performance gap between the industry’s leaders and laggards. Companies that make the strategic decision to invest heavily in building integrated, enterprise-wide data and AI infrastructure will be able to accelerate their pipelines, reduce their costs, and make smarter decisions. Those that treat AI as a series of siloed, experimental pilot projects risk being left permanently behind. This also recalibrates the M&A landscape, where the acquisition of a smaller biotech may now be valued as much for its unique data assets and AI talent as for its drug pipeline.
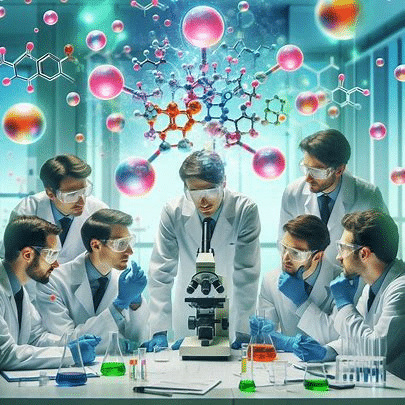
Personalized Medicine: The End of “One-Size-Fits-All”
For the better part of a century, the practice of medicine has been dominated by the “one-size-fits-all” blockbuster model: developing a single drug to treat millions of people with the same condition. While this approach has produced many life-saving treatments, it is inherently inefficient, as individual responses to a given drug can vary dramatically. We are now witnessing the definitive end of that era and the rise of its successor: personalized medicine.
This new paradigm represents a fundamental shift in philosophy, moving from treating diseases to treating individual patients. It leverages cutting-edge insights into a person’s unique genetic makeup, lifestyle, and environment to develop therapies that are more effective, carry fewer side effects, and are tailored to the specific biology of their disease.2 The market for this revolutionary approach is vast and growing rapidly. The global personalized medicine market, valued at over $614 billion in 2024, is projected to more than double to over $1.3 trillion by 2034, growing at a steady CAGR of 8.1%.
This transformation is being driven by a powerful convergence of enabling technologies:
- Multi-Omics: This is the integrated analysis of multiple layers of biological data. It goes beyond just genomics (the DNA blueprint) to include transcriptomics (which genes are active), proteomics (the proteins present in the body), and metabolomics (the chemical fingerprints of cellular processes).36 By combining these datasets, scientists can build a far richer, more dynamic picture of an individual’s health and disease state.
- AI and Advanced Data Analytics: The sheer volume and complexity of multi-omics data would be impossible for humans to analyze alone. AI and machine learning are the engines that make personalized medicine possible, sifting through these massive datasets to identify the subtle patterns, biomarkers, and genetic signatures that can predict disease risk and treatment response. The market for AI specifically within precision medicine is forecast to grow at an astonishing 35.8% CAGR, a testament to its critical role.
- Advanced Diagnostics: The practical application of personalized medicine relies on new diagnostic tools that can quickly and affordably capture this biological data. Technologies like next-generation sequencing (NGS) and “liquid biopsies”—simple blood tests that can detect circulating tumor DNA (ctDNA)—are moving from the research lab to the clinic. They are making it possible to diagnose diseases like cancer at their earliest stages, monitor treatment response in real-time, and match patients to the most effective therapies.36
Nowhere is the impact of personalized medicine more evident than in oncology, which currently represents the largest segment of the market, accounting for over 40% of its value. By 2025, a cancer patient’s journey may look radically different. An oncologist might routinely order comprehensive tumor profiling, providing a complete molecular fingerprint of the cancer, rather than just a general diagnosis based on its location in the body. For patients in remission, minimal residual disease (MRD) testing via liquid biopsy could detect a potential recurrence months earlier than traditional imaging scans, allowing for intervention when the cancer is most treatable.
This scientific revolution necessitates a corresponding revolution in business models. The blockbuster playbook of deploying vast sales armies to promote a single drug to a broad population is becoming obsolete. The new commercial model for personalized medicine is far more complex and data-driven. Success no longer depends on volume, but on value. The strategy involves:
- Companion Diagnostics: Developing a specific diagnostic test alongside a drug to identify the precise patient population that will benefit from it.
- Biomarker-Driven Targeting: Focusing R&D and commercial efforts on smaller, well-defined patient subgroups identified by specific genetic or molecular biomarkers.
- Value-Based Pricing: Justifying premium prices by demonstrating superior efficacy and safety in a targeted population, often supported by real-world evidence and health economic outcomes data.
This transition from a high-volume, low-information model to a high-value, high-information model is challenging. It requires a complete overhaul of R&D priorities, clinical trial design, regulatory strategy, and commercial infrastructure. However, it also holds the promise of a more rational and effective drug development process, one that delivers truly transformative treatments to the patients who need them most.
Antibody-Drug Conjugates (ADCs): The Rise of “Smart Chemotherapy”
As pharmaceutical companies search for the “next big thing,” one technology has emerged as a particularly powerful and strategically attractive option: the Antibody-Drug Conjugate, or ADC. Often described as “smart chemotherapy” or a biological “magic bullet,” ADCs represent a sophisticated fusion of targeted antibody therapy and potent cytotoxic drugs, designed to deliver a killer blow directly to cancer cells while minimizing collateral damage to healthy tissue.38 The market for these advanced therapies is exploding, projected to grow from approximately $7 billion in 2025 to between $17 billion and $34 billion by 2032, with a blistering CAGR of 14-17.5%.22
The elegance of an ADC lies in its three-part structure:
- The Antibody: A monoclonal antibody (mAb) that acts as a highly specific targeting system. It is engineered to recognize and bind to a specific antigen that is overexpressed on the surface of cancer cells.
- The Payload: A highly potent cytotoxic drug, often a form of chemotherapy that would be too toxic to administer systemically on its own.
- The Linker: A chemical bridge that covalently binds the payload to the antibody. The linker is the unsung hero of the ADC, designed to be stable in the bloodstream to prevent premature drug release, but to cleave and release its toxic payload once the ADC has been internalized by the target cancer cell.22
The development of ADCs has been a story of iterative improvement, evolving through distinct generations as scientists refined each of the three components to enhance efficacy and reduce toxicity.42
- First-Generation ADCs: Early attempts, like Pfizer’s Mylotarg® (gemtuzumab ozogamicin), were pioneering but flawed. They often used mouse-derived antibodies, which could trigger an immune response in patients, and were built with unstable linkers (like acid-sensitive hydrazone linkers) that could release the payload prematurely in the bloodstream, leading to severe off-target toxicity.42
- Second-Generation ADCs: This wave brought significant improvements. Companies switched to less immunogenic humanized or fully human antibodies and developed more stable linkers. However, these ADCs, such as Adcetris (brentuximab vedotin) and Kadcyla (trastuzumab emtansine), were typically produced using a random, stochastic conjugation method. This process attached the payload to available lysine or cysteine residues on the antibody, resulting in a heterogeneous mixture of molecules with a variable drug-to-antibody ratio (DAR) ranging from 0 to 8. This heterogeneity made the drug’s behavior unpredictable and could compromise its therapeutic window.
- Third-Generation and Beyond: The current state-of-the-art in ADC technology represents a major leap forward. The key innovations include site-specific conjugation, which uses advanced bioengineering techniques to attach a precise number of payload molecules to a specific location on the antibody. This creates a homogeneous product with a consistent DAR (typically 2 or 4), leading to more predictable pharmacokinetics and an improved safety profile.42 This generation is also defined by a new class of payloads. Instead of the ultra-potent tubulin inhibitors used in earlier ADCs, a new wave of highly successful drugs like AstraZeneca and Daiichi Sankyo’s Enhertu® (trastuzumab deruxtecan) and Gilead’s Trodelvy® (sacituzumab govitecan) utilize moderately potent topoisomerase I inhibitors as their payload. This seemingly counterintuitive move has been a game-changer.
The shift to moderately potent payloads unlocked a critical mechanism: the bystander effect. Because the payload is less toxic, more of it can be loaded onto each antibody, resulting in a high DAR of 8. When this ADC reaches a tumor, the released payload is not only potent enough to kill the target cell but is also membrane-permeable, allowing it to diffuse out and kill adjacent tumor cells, even if those cells don’t express the target antigen. This is a crucial advantage in treating solid tumors, which are often heterogeneous, meaning not all cells within the tumor express the same surface proteins. The bystander effect allows the ADC to overcome this heterogeneity, leading to a more profound and durable anti-tumor response.
This combination of sophisticated engineering and clever biology makes ADCs a perfect strategic fit for large pharmaceutical companies navigating the post-patent-cliff world. They represent an evolutionary, rather than a completely revolutionary, step. They leverage existing, well-understood expertise in monoclonal antibody development and manufacturing while delivering a step-change in therapeutic efficacy. This makes them a less risky and more accessible innovation compared to the immense complexities of cell and gene therapy. For companies like AstraZeneca, Daiichi Sankyo, Pfizer, Gilead, and Roche, ADCs serve as a powerful bridge between the old world of small molecules and the new world of complex biologics, offering a clear and promising path to replenishing their pipelines and securing future growth.
mRNA and RNA Therapeutics: The Messenger’s New Mission
The unprecedented speed and success of the mRNA COVID-19 vaccines was more than just a triumph of public health; it was a global, real-world proof-of-concept for one of the most versatile and promising platforms in modern biotechnology. While the pandemic thrust mRNA into the spotlight as a vaccine technology, its true therapeutic potential extends far beyond infectious diseases. The industry is now pivoting to harness this technology for a new mission: treating a vast range of conditions from rare genetic disorders to cancer.19
The underlying science of therapeutic mRNA is both elegant and powerful. For a business audience, it can be understood as a biological software update. Scientists design and synthesize a strand of messenger RNA that contains the instructions for a specific, functional protein. This mRNA is then packaged into a delivery vehicle—most commonly a lipid nanoparticle (LNP)—and administered to the patient.46 Once inside the body’s cells, the cellular machinery reads these instructions and begins producing the therapeutic protein. This approach has several key advantages over other methods. First, it is
transient; the mRNA degrades naturally after a few days, so the protein production is not permanent, avoiding the long-term risks associated with permanent gene modification.48 Second, it avoids the risk of
genomic integration, a major safety concern with some viral vector-based gene therapies.
This versatile platform is being explored across several key therapeutic applications:
- Protein Replacement Therapy: This is arguably the most promising near-term application. Many rare genetic diseases, such as cystic fibrosis or methylmalonic acidaemia, are caused by a single faulty gene that results in a missing or non-functional protein. mRNA therapy offers a way to restore this function by providing the cells with the correct instructions.46 A key advantage here is that mRNA can be used to produce intracellular and transmembrane proteins, a feat that is difficult or impossible with traditional protein replacement therapies, which are typically limited to secreted proteins.
- Cancer Vaccines and Therapeutics: The next frontier is personalized cancer vaccines. In this approach, a patient’s tumor is sequenced to identify unique mutations, or “neoantigens.” An mRNA vaccine is then custom-designed to teach the patient’s own immune system to recognize and attack cancer cells bearing these specific markers.23 Moderna’s individualized neoantigen therapy, mRNA-4157 (partnered with Merck), is one of the most closely watched assets in this space and a cornerstone of its post-COVID pipeline.
- Gene Editing Delivery: mRNA can also serve as a delivery tool for other advanced therapies. Instead of a therapeutic protein, the mRNA can carry the instructions for the components of a gene editing system, such as the Cas9 nuclease and guide RNA used in CRISPR, providing a transient and potentially safer way to perform gene editing in vivo.
Despite its immense promise, the widespread application of mRNA therapeutics is constrained by one major obstacle: the delivery problem. Naked mRNA is an incredibly fragile molecule. It is quickly degraded by enzymes in the bloodstream and, due to its size and negative charge, cannot easily cross the cell membrane.49 Solving this challenge is the key to unlocking mRNA’s full potential.
The current state-of-the-art solution is the Lipid Nanoparticle (LNP), a microscopic sphere of specialized lipids that encapsulates and protects the mRNA on its journey through the body.52 However, LNPs come with their own set of challenges. Scientists are working to improve their stability to avoid the need for ultra-cold storage, a major logistical hurdle. A more significant challenge is targeting. Current LNP formulations have a natural tendency to accumulate in the liver, which is useful for treating liver diseases but makes it difficult to deliver mRNA to other organs like the lungs, brain, or muscle tissue. Finally, even after the LNP is taken up by a target cell, it must be able to escape from an internal compartment called the endosome to release its mRNA cargo into the cytoplasm where it can be translated. Ensuring this “endosomal escape” is efficient is a critical area of ongoing research.
The competitive landscape for mRNA is dominated by the pioneers of the COVID-19 vaccines, Moderna and BioNTech. However, the post-pandemic reality has been challenging. With vaccine revenues declining, both companies are facing significant economic pressure and have been forced to recalibrate their strategies. In 2025, both Moderna and BioNTech announced significant layoffs and pipeline restructurings to conserve cash and focus on their most promising near-term therapeutic programs.33 Other players, like
Arcturus Therapeutics, are following a similar path, discontinuing more speculative early-stage vaccine programs to double down on their core mRNA therapeutic assets for conditions like cystic fibrosis. This period of consolidation and strategic refocusing underscores the immense potential of therapeutic mRNA, but also the significant scientific and financial hurdles that must be overcome to turn that potential into a broad clinical reality.
Cell & Gene Therapy (CGT): Engineering the “Living Drugs” of Tomorrow
While AI, personalized medicine, and ADCs represent profound advances, the most disruptive and potentially transformative frontier in biotechnology is the field of Cell and Gene Therapy (CGT). These are not conventional drugs that are manufactured in a chemical plant; they are complex, often personalized treatments that involve the fundamental manipulation of human biology. The CGT market is projected to experience explosive growth, with some forecasts predicting a stunning 44% CAGR through 2030, surging from $8.7 billion in 2024 to over $76 billion.36
This revolution stands on two main pillars:
- Cell Therapy: This involves extracting a patient’s own cells, modifying them outside the body to enhance their therapeutic properties, and then re-infusing them. The most prominent example is CAR-T therapy.
- Gene Therapy: This aims to treat or cure diseases by directly correcting the underlying genetic fault, often using revolutionary gene editing tools like CRISPR.
Together, these approaches are moving medicine from an era of chronic treatment to one of potential one-time cures, a shift that carries both unprecedented promise and unparalleled challenges.
CAR-T Therapy: Weaponizing the Immune System
Chimeric Antigen Receptor T-cell (CAR-T) therapy is a remarkable form of immunotherapy that turns a patient’s own immune cells into a highly targeted, “living drug” to fight cancer. The process, while scientifically complex, can be understood as a series of sophisticated steps:
- Collection (Leukapheresis): The process begins at the patient’s bedside, where blood is drawn and passed through an apheresis machine that separates out the T-cells, the primary soldiers of the immune system.59
- Engineering: These T-cells are then cryopreserved and shipped to a specialized, highly controlled manufacturing facility. There, they are genetically engineered, typically using a disarmed viral vector, to express a new protein on their surface: the Chimeric Antigen Receptor, or CAR. This receptor is a synthetic protein, part antibody and part signaling molecule, designed to recognize and latch onto a specific antigen found on the surface of the patient’s cancer cells.
- Expansion: The newly engineered CAR-T cells are then cultured and expanded in the lab, multiplying until there are hundreds of millions of them.
- Infusion: This final CAR-T cell product is frozen and shipped back to the hospital. After the patient undergoes a brief course of chemotherapy to deplete their existing lymphocytes (making room for the new cells), the CAR-T cells are infused back into the patient’s bloodstream in a single session.58
- Attack: If all goes according to plan, these “supercharged” T-cells will circulate throughout the patient’s body, seek out any cells bearing the target antigen, and launch a powerful and precise attack, killing the cancer cells.
The clinical results for CAR-T have been nothing short of revolutionary, particularly in patients with advanced blood cancers who have failed all other treatments. Therapies like Kymriah (Novartis), Yescarta (Gilead/Kite), Breyanzi (BMS/Juno), and Abecma (BMS/bluebird bio) have produced deep and durable remissions, with many patients remaining cancer-free for years after a single infusion.58
However, this incredible therapeutic potential comes with a set of equally incredible hurdles that represent major barriers to its widespread use:
- Manufacturing and Supply Chain Complexity: The “vein-to-vein” time—from cell collection to infusion—is a logistical nightmare. It is a highly personalized, time-sensitive process that requires cryogenic shipping, flawless coordination between the hospital and the manufacturing site, and an unbreakable “chain of identity” to ensure the right patient gets their own cells back.59 Unlike producing a pill, this process cannot be easily scaled, and any error can have fatal consequences. This is the single greatest bottleneck in the field.
- Astronomical Cost and Reimbursement Challenges: The bespoke, labor-intensive manufacturing process leads to staggering costs. The list price for the therapy alone is often between $400,000 and $500,000, and when hospitalization, supportive care, and management of side effects are included, the total cost of care can easily exceed $1 million per patient.67 This creates a crisis for reimbursement systems. Payers in the U.S. are not structured to handle such massive, one-time payments for curative therapies, especially given the high rate of patient churn in commercial insurance plans, which means a payer might foot the bill for a cure only for the patient to switch to a competitor’s plan the following year.69
- Significant Safety Risks: The powerful immune activation triggered by CAR-T cells can lead to severe and potentially life-threatening side effects. The two most common are Cytokine Release Syndrome (CRS), a systemic inflammatory response that can cause high fevers and dangerous drops in blood pressure, and Immune Effector Cell-Associated Neurotoxicity Syndrome (ICANS), which can cause confusion, seizures, and cerebral edema. Managing these toxicities requires highly specialized care in an experienced academic medical center.60
CRISPR Gene Editing: Rewriting the Code of Life
If CAR-T therapy is about weaponizing existing cells, CRISPR gene editing is about rewriting the fundamental source code of life itself. Adapted from a natural defense system found in bacteria, the CRISPR-Cas9 system has been repurposed into a revolutionary gene editing tool of unprecedented precision and ease of use.72
For a business audience, the technology is best understood through the “molecular scissors” analogy. The system consists of two key components:
- The Cas9 Enzyme: This is the “scissor” molecule, a nuclease that is capable of cutting both strands of a DNA helix.
- The Guide RNA (gRNA): This is a small, programmable piece of RNA that acts as the “GPS,” directing the Cas9 scissors to a precise, specific sequence in the genome.72
The process is remarkably straightforward. Scientists design a gRNA that is complementary to the faulty gene they wish to edit. When the CRISPR-Cas9 system is introduced into a cell, the gRNA guides the Cas9 enzyme to the target location. Cas9 then makes a clean, double-stranded break in the DNA.72 At this point, scientists can leverage the cell’s own natural DNA repair machinery to make a change. The cell can either try to patch the break together through a process called non-homologous end joining (NHEJ), which is error-prone and typically results in the deactivation or
“knockout” of the target gene. Alternatively, if scientists provide a correct DNA template, the cell can use a more precise pathway called homology-directed repair (HDR) to patch the break, effectively replacing the faulty gene with the correct version in a process known as “knock-in”.72
The therapeutic promise of this technology is almost boundless. It holds the potential to provide a one-time, permanent cure for thousands of monogenic diseases—disorders caused by a mutation in a single gene—such as sickle cell disease, beta-thalassemia, cystic fibrosis, and Huntington’s disease.25 The field has already reached a major milestone with the regulatory approval of
Casgevy (exagamglogene autotemcel), a CRISPR-based therapy developed by CRISPR Therapeutics and Vertex Pharmaceuticals, for the treatment of sickle cell disease and transfusion-dependent beta-thalassemia.
The clinical landscape is advancing at a breathtaking pace. As of early 2025, there were approximately 250 clinical trials underway involving various gene-editing technologies, with over 150 actively recruiting patients. These trials are targeting a wide range of diseases, including blood disorders, various cancers, viral diseases like HIV, cardiovascular conditions, and autoimmune diseases. Key corporate players leading this charge include CRISPR Therapeutics, Vertex Pharmaceuticals, Intellia Therapeutics, and Editas Medicine.
However, the power to rewrite the code of life comes with profound responsibilities and significant risks. The single greatest scientific and safety concern is the potential for “off-target effects.” This occurs when the CRISPR system mistakenly cuts the DNA at an unintended location in the genome. While the system is highly precise, it is not perfect, and an off-target cut could have disastrous consequences, such as disrupting a healthy gene or, in the worst-case scenario, activating an oncogene and causing cancer. A tremendous amount of research is focused on improving the specificity of the system and developing methods to detect and eliminate any off-target edits.74 Because these are permanent genetic changes, long-term safety monitoring is paramount, but by its nature, this data takes many years to collect.78
Beyond the scientific challenges lie deep ethical concerns. While the use of CRISPR to edit somatic cells (non-reproductive cells) to treat disease in an individual is widely supported, the prospect of editing germline cells (eggs, sperm, or embryos) raises a host of ethical dilemmas. Germline editing would create changes that are heritable, passed down to all future generations. This opens the door to the possibility of “designer babies” and the enhancement of normal human traits like intelligence or height, a prospect that has led to a broad international consensus against its use in humans. Germline editing is currently illegal in the United States and many other countries due to these profound ethical and safety concerns.77
Part 3: Navigating the New Ecosystem – Strategy, Investment, and the Path Forward
The tectonic shift from the blockbuster model to a future dominated by complex, data-driven biotechnologies is creating a new and challenging ecosystem for the pharmaceutical industry. Success is no longer guaranteed by scale or legacy. It now depends on a company’s ability to navigate a turbulent investment landscape, adopt entirely new business models, and overcome unprecedented hurdles in regulation, manufacturing, and market access. Strategic agility, powered by sophisticated intelligence, has become the ultimate currency.
The Shifting Tides of Capital: Following the Money in Biotech
The flow of capital into the biotech sector provides a clear barometer of industry sentiment and strategic priorities. After the frenzied, record-breaking investment peak during the COVID-19 pandemic in 2021, the market has undergone a significant correction. Venture capital (VC) funding, the lifeblood of early-stage innovation, has tightened considerably.
However, the story of 2025 is one of nuanced recovery and strategic realignment. While the total volume of deals remains below pre-pandemic averages, the size of those deals is increasing for companies that can demonstrate compelling, de-risked science. Investors are becoming more selective, pivoting away from high-risk, early-stage platform technologies and toward companies with assets in mid-stage validation that show a clearer path to clinical success and commercialization. This “flight to quality” means that while it is harder for a new biotech to secure its initial seed funding, those that do and can deliver on their milestones are able to raise substantial amounts of capital in later rounds.
The allocation of this capital clearly follows the technological trends reshaping the industry. The areas attracting the most significant investment are:
- AI-Driven Drug Discovery: Companies that are successfully leveraging AI are commanding enormous valuations and attracting massive investment rounds. A prime example is Xaira Therapeutics, which raised a staggering $1 billion in its Series A financing, a clear testament to investor confidence in the power of AI to revolutionize R&D.
- Cell and Gene Therapy: Despite the immense manufacturing and cost challenges, the curative potential of CGT makes it an irresistible area for investment. Both large and small companies in the space continue to attract significant funding to advance their pipelines.24
- Core Therapeutic Areas: Oncology, immunology, and rare diseases remain the top priorities for investors, reflecting the high unmet medical need and the potential for premium pricing in these areas.21
For early-stage biotechs, this tighter funding environment makes strategic partnerships, licensing deals, and M&A with Big Pharma more critical than ever. Large pharmaceutical companies, flush with cash but facing the patent cliff, are actively seeking to in-license or acquire promising assets to replenish their pipelines.15 This creates a symbiotic relationship where small innovators gain access to much-needed capital and development expertise, while large companies gain access to the next generation of therapeutic technologies. A notable trend in this area is the increasing prominence of China-based biotechs, which are becoming major players in the global licensing and partnership landscape, cementing the country’s role as a rising power in biopharmaceutical innovation.84
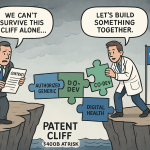
Rewriting the Playbook: New Business Models and the Power of Competitive Intelligence
The transition from the blockbuster era to the age of personalized medicine necessitates a complete rewriting of the pharmaceutical business playbook. The commercial model for a $30 cholesterol pill prescribed to millions is fundamentally incompatible with the model required for a $500,000 gene therapy administered once to a few thousand patients. The strategic focus must shift from achieving high volume through mass-market promotion to demonstrating profound value in well-defined, niche patient populations.1
In this new, complex, and rapidly evolving environment, competitive intelligence (CI) has transformed from a useful ancillary function into a core strategic imperative. Companies can no longer afford to operate with an incomplete picture of the competitive landscape. They must systematically and continuously monitor their rivals’ R&D activities, clinical trial designs and results, regulatory strategies, and patent portfolios to make informed, high-stakes decisions about their own pipelines and corporate strategy.87
This is where specialized, data-driven platforms like DrugPatentWatch become indispensable. In an era defined by data, these tools provide the granular, real-time intelligence that is essential for survival and success. They aggregate and analyze vast amounts of information from disparate sources—including patent filings, FDA databases like the Orange Book, clinical trial registries, and litigation records—to provide actionable insights that support critical business functions 87:
- Anticipating Competition and Managing Portfolios: For branded manufacturers, these tools provide a clear line of sight into when their key products will face generic or biosimilar competition. By tracking patent expiration dates, ongoing litigation, and Paragraph IV challenges (the process by which generic companies challenge innovator patents), companies can build precise financial models to forecast revenue declines and manage investor expectations.89 For generic and API manufacturers, this same data helps identify market entry opportunities and inform portfolio management decisions.
- Deconstructing Competitor Strategy: A competitor’s patent portfolio is more than just a legal document; it is a strategic roadmap. By meticulously analyzing the claims, examples, and descriptions within a competitor’s patents, a company can reverse-engineer their formulation strategies, understand the technical challenges they faced, and identify their R&D direction. This allows for the identification of “white space” for a company’s own innovation or the development of “design-around” strategies to avoid infringement.
- Informing R&D and Business Development: Comprehensive CI helps R&D leaders make smarter portfolio prioritization decisions. By understanding the competitive intensity in a given therapeutic area—how many rivals are pursuing similar mechanisms or targeting the same patient populations—companies can avoid crowded fields and instead allocate resources to areas with higher unmet needs and greater commercial potential.
This highlights a crucial evolution in the role of competitive intelligence. Historically, CI related to patents was primarily a defensive activity, focused on protecting one’s own blockbuster fortress from legal challenges and generic entrants. The goal was risk mitigation. In the new ecosystem, however, CI has become a powerful offensive weapon.
The strategic calculus has changed. In the old model, the primary question was, “How do we defend our patent?” In the new model, the question is, “What does the entire patent landscape tell us about where the opportunities are?” A sophisticated analysis of patent data can become a treasure map. A generic company can use the detailed information in the FDA’s Orange Book, as aggregated by platforms like DrugPatentWatch, to proactively design a non-infringing product or craft a “skinny label” strategy that carves out patented uses, accelerating their path to market. A small biotech can analyze the landscape to find a less-crowded biological pathway to target, increasing its chances of success. An innovator can even use this intelligence to identify the next logical improvement for its own product line before a competitor does. The value of these intelligence platforms is no longer just about managing legal risk; it is a fundamental tool for strategic R&D planning, business development, and market domination. Companies that master this offensive use of CI will be able to navigate the complex terrain more nimbly, make smarter bets, and move faster than their rivals.
The Final Hurdles: Overcoming Regulatory, Manufacturing, and Reimbursement Barriers
While the scientific promise of the new biotech frontier is immense, the path from the lab to the patient is littered with formidable non-scientific hurdles. Successfully commercializing these novel therapies requires navigating a gauntlet of complex and often archaic systems in regulation, manufacturing, and reimbursement.
The regulatory landscape is struggling to keep pace with the speed of innovation. For cell and gene therapies in particular, the traditional regulatory pathways designed for small molecules and conventional biologics are often a poor fit. Recognizing this, the U.S. Food and Drug Administration (FDA) has made efforts to adapt, creating new specialized offices like the Office of Therapeutic Products (OTP) and new programs like the INitial Targeted Engagement for Regulatory Advice on CBER producTs (INTERACT) to provide earlier and more frequent guidance to developers. However, significant challenges remain in establishing clear, consistent, and predictable regulatory requirements for the chemistry, manufacturing, and controls (CMC) and clinical development of these highly complex products.93
For many advanced therapies, especially CGTs, manufacturing is the single greatest bottleneck. The industry lacks the scalable, automated, and cost-effective production methods needed to meet potential demand. Autologous therapies like CAR-T, which are created on a patient-by-patient basis, are particularly challenging to scale out. This reliance on manual, labor-intensive processes in highly specialized, sterile facilities leads to several critical problems: limited manufacturing capacity and “slot” availability, which creates long and often life-threatening wait times for patients; high variability between batches; and an extremely high cost of goods, which is the primary driver of the therapies’ astronomical prices.66
This high cost feeds directly into the final and perhaps most intractable hurdle: the reimbursement crisis. The U.S. healthcare system, with its fragmented payer landscape and focus on annual budgets, is fundamentally ill-equipped to handle the financial shock of multi-million-dollar, one-time curative therapies. Payers face several dilemmas. The first is the sheer “sticker shock” of the upfront cost, which can strain budgets and reinsurance policies.69 The second is the problem of
patient churn. A commercial insurer may be hesitant to pay $2 million for a gene therapy that cures a patient’s condition, only to have that patient switch to a different insurance plan the following year. In this scenario, the initial payer bears the full cost while the long-term cost savings (from avoiding a lifetime of chronic care) accrue to a competitor. To address this misalignment, the industry and payers are exploring innovative value-based arrangements, where payment is tied to clinical outcomes. However, these agreements are logistically complex to implement and track, and their adoption has been slow. Until these systemic barriers are overcome, the most revolutionary medicines may remain out of reach for the vast majority of patients who could benefit from them.
Conclusion: The Future is Complex, Collaborative, and Data-Driven
The pharmaceutical industry is in the midst of a profound and irreversible transformation. The patent cliff of 2025-2030 is not merely a cyclical financial challenge; it is the definitive end of the blockbuster era and the powerful catalyst forcing a fundamental reinvention of the industry’s scientific, strategic, and commercial models. The comfortable, chemistry-based playbook that generated decades of predictable growth has been replaced by a new reality that is complex, uncertain, and defined by the convergence of advanced biology and data science.
The path forward is no longer about finding the next billion-dollar pill for a mass market. It is about mastering a diverse and challenging arsenal of new therapeutic modalities. It requires a deep understanding of the intricate mechanisms of Antibody-Drug Conjugates, the delicate delivery challenges of mRNA therapeutics, and the revolutionary but logistically demanding world of cell and gene therapies like CAR-T and CRISPR. The science is more complex, the manufacturing more difficult, and the commercial models more nuanced than ever before.
In this new ecosystem, the profile of a successful pharmaceutical company is being redrawn. The winners will not necessarily be the largest or the ones with the biggest sales forces. Instead, they will be the organizations that demonstrate excellence in three critical domains:
- Mastery of Complex Science: The future of medicine lies in a deep and integrated understanding of genomics, proteomics, immunology, and cell biology. Companies must cultivate or acquire the scientific talent capable of navigating these complex fields to develop truly differentiated therapies.
- Harnessing the Power of Data: Data has become as valuable as intellectual property. The ability to build and deploy enterprise-wide AI and data analytics capabilities is no longer a competitive advantage but a prerequisite for survival. This is the key to accelerating discovery, de-risking development, and delivering the promise of personalized medicine.
- Unwavering Strategic Agility: The landscape is shifting too quickly for rigid, long-term plans. Success will demand a culture of agility, powered by sophisticated, real-time competitive intelligence. Companies must be able to expertly navigate the turbulent investment climate, forge strategic partnerships, and proactively adapt to evolving regulatory and reimbursement environments.
The road ahead is undeniably fraught with scientific, financial, and systemic challenges. Yet, for the first time in history, the industry possesses the tools to not just treat, but to potentially cure, diseases that were once considered intractable. The companies that can successfully bridge the gap between this incredible scientific promise and the harsh realities of the market will not only survive the patent cliff—they will define the future of human health.
Industry Insight:
“We believe the biggest headwind to large pharma revenue growth over the next five years is loss of exclusivity…. The pharmaceutical industry is bracing for one of its most financially significant patent cliffs in over a decade, with multiple blockbuster drugs set to lose exclusivity by 2030. As biosimilars and generics flood the market, pricing pressures will intensify—particularly in oncology—challenging pharma companies to rethink revenue strategies, pipeline investments, and lifecycle management to safeguard long-term growth.”
Citation: William Blair analysts, as reported by BioSpace , and a GlobalData report.
Key Takeaways
- The End of the Blockbuster Era: The traditional pharmaceutical model of developing mass-market “blockbuster” drugs is broken, strained by rising R&D costs and payer resistance. This is being accelerated by an unprecedented patent cliff between 2025-2030, which puts over $200 billion in annual revenue at risk from drugs like Keytruda, Eliquis, and Opdivo.
- Divergent Survival Strategies: In response, Big Pharma is pursuing divergent paths. Some, like Eli Lilly, are betting on internal innovation (“Build”). Others, like AbbVie, have historically relied on massive M&A (“Buy”). And some, like BMS, are resorting to deep cost-cutting and layoffs (“Cut”). The success of these strategies will reshape the competitive landscape.
- AI is the New R&D Infrastructure: Artificial Intelligence is no longer a niche tool but a foundational element of drug discovery and development. It is accelerating timelines, reducing costs, and optimizing clinical trials. The competitive edge is shifting from owning a molecule to owning the proprietary data and algorithms that create them.
- The Rise of High-Value, Niche Therapeutics: The future of medicine is personalized, targeted, and complex. The industry is pivoting to advanced platforms like:
- Personalized Medicine: Using genomics and biomarkers to tailor treatments to individuals, especially in oncology.
- Antibody-Drug Conjugates (ADCs): “Smart chemotherapy” that offers a powerful and strategically attractive bridge between traditional pharma and next-generation biotech.
- mRNA Therapeutics: Moving beyond vaccines to treat rare genetic diseases and create personalized cancer therapies, though delivery remains a key challenge.
- Cell & Gene Therapy (CGT): The most disruptive frontier, with “living drugs” like CAR-T and curative-intent gene editing tools like CRISPR, which face immense manufacturing, cost, and reimbursement hurdles.
- Competitive Intelligence as a Core Function: In this complex and fast-moving environment, systematically gathering and analyzing competitive intelligence is essential. Platforms like DrugPatentWatch are critical for anticipating patent expirations, deconstructing competitor strategies, and making smarter R&D portfolio decisions.
- Systemic Hurdles Remain: The full potential of these new technologies is constrained by significant non-scientific barriers. The industry must overcome complex regulatory pathways, manufacturing bottlenecks (especially for CGTs), and a reimbursement system not designed for high-cost, one-time curative therapies.
Frequently Asked Questions (FAQ)
1. What makes the 2025-2030 patent cliff different from previous ones?
This patent cliff is distinguished by both its sheer financial scale and the nature of the drugs involved. With over $200 billion in annual revenue at risk, it is one of the largest in history.5 Furthermore, it heavily impacts not just traditional small-molecule drugs but also a host of complex biologics and first-in-class therapies, particularly in oncology and immunology (e.g., Keytruda, Opdivo, Eliquis).6 This means the competitive landscape will be shaped by the entry of both generics and more complex, costly-to-develop biosimilars, creating a more unpredictable and challenging environment for innovator companies than in past cliffs that were dominated by small-molecule expirations.
2. Why are Antibody-Drug Conjugates (ADCs) considered such a strategic “sweet spot” for Big Pharma right now?
ADCs occupy a unique strategic position that makes them highly attractive for large pharmaceutical companies looking to replenish their pipelines. They represent an evolutionary, rather than a completely revolutionary, step. They leverage existing, well-established corporate expertise in monoclonal antibody development and manufacturing, which reduces the technical and logistical risk compared to building capabilities in cell and gene therapy from scratch. At the same time, they offer a significant leap in efficacy over traditional chemotherapy by targeting cancer cells directly. The latest generation of ADCs, with their stable linkers and novel payloads that enable a “bystander effect,” have proven to be highly effective in treating heterogeneous solid tumors, addressing a major unmet need. This combination of manageable risk and high reward makes them a perfect “bridge” technology for companies seeking to innovate without completely abandoning their core competencies.
3. Beyond the hype, what is the single biggest practical barrier holding back widespread use of CAR-T and CRISPR therapies?
While cost and safety are significant issues, the single biggest practical barrier is manufacturing and logistics.66 For autologous therapies like CAR-T and the currently approved CRISPR therapy Casgevy, the process is bespoke for every single patient. It involves a complex, time-sensitive “vein-to-vein” supply chain that requires extracting a patient’s cells, shipping them under cryogenic conditions to a centralized facility, performing complex genetic engineering in a sterile environment, and shipping the final “living drug” back for infusion. This process is incredibly difficult to scale, creates major capacity bottlenecks (leading to long patient wait times), and is the primary driver of the therapies’ multi-hundred-thousand-dollar price tags. Until the industry can develop more automated, decentralized, or “off-the-shelf” (allogeneic) manufacturing solutions, these revolutionary therapies will remain accessible to only a small fraction of eligible patients.
4. How is AI changing the nature of competition in the pharmaceutical industry?
AI is shifting the basis of competition from owning a patented molecule to owning a proprietary data and analytics platform. The competitive moat is no longer just the patent, but the algorithm. A company with a superior AI model for predicting drug toxicity, identifying novel targets, or selecting the right patients for a clinical trial has a durable advantage that is difficult to replicate. This creates a “winner-take-most” dynamic where companies with large, high-quality proprietary datasets (often the incumbent Big Pharma players) can create a virtuous cycle: more data leads to better AI, which leads to better drugs and trial outcomes, which in turn generates more data. This forces all players to treat data and AI not as a support function, but as a core strategic asset.
5. If personalized medicine targets smaller patient populations, how can it be as profitable as the old blockbuster model?
The business model for personalized medicine replaces the blockbuster’s focus on volume with a focus on value. While the target patient population for a personalized therapy may be much smaller, the drug’s price can be significantly higher for several reasons. First, the therapy’s efficacy is typically much greater in a well-defined, biomarker-selected population, which can justify a premium price to payers. Second, the development process can be more efficient; clinical trials may be smaller and shorter, and the probability of success is higher, reducing overall R&D risk and cost. Finally, many personalized medicines, particularly in oncology and rare diseases, come with orphan drug designations and other regulatory incentives that provide extended periods of market exclusivity, further enhancing their long-term value. The model is not about selling to everyone, but about delivering transformative outcomes to a specific group of patients and being compensated for that high level of value.
References
- The Meteoric Rise of CAR-T Cell Therapies: List of CAR-T Companies – BioInformant, accessed August 2, 2025, https://bioinformant.com/car-t-companies-the-meteoric-rise-of-cellular-immunotherapies/
- The New Pharma Playbook: From Data Overload to Market Domination – DrugPatentWatch, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/new-business-models-for-pharmaceutical-marketing-transforming-data-into-market-domination/
- Bye, bye blockbusters, hello niche busters – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3153529/
- Pharma’s Rx for R&D | McKinsey & Company, accessed August 2, 2025, https://www.mckinsey.com/featured-insights/sustainable-inclusive-growth/charts/pharmas-rx-for-r-and-d
- Patent cliff and strategic switch: exploring strategic design possibilities in the pharmaceutical industry – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4899342/
- The End of Exclusivity: Navigating the Drug Patent Cliff for …, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/the-impact-of-drug-patent-expiration-financial-implications-lifecycle-strategies-and-market-transformations/
- Big Pharma prepare for next patent cliff as blockbuster drugs revenue losses loom, says GlobalData, accessed August 2, 2025, https://www.globaldata.com/media/pharma/big-pharma-prepare-next-patent-cliff-blockbuster-drugs-revenue-losses-loom-says-globaldata/
- Top Strategies for Pharma Profitability after Drug Patents Expire – DrugPatentWatch, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/top-strategies-for-pharma-profitability-after-drug-patents-expire/
- Drug Patent Expirations: Potential Effects on Pharmaceutical Innovation – UM Carey Law, accessed August 2, 2025, https://www2.law.umaryland.edu/marshall/crsreports/crsdocuments/R42399_03022012.pdf
- 5 Pharma Powerhouses Facing Massive Patent Cliffs—And What They’re Doing About It, accessed August 2, 2025, https://www.biospace.com/business/5-pharma-powerhouses-facing-massive-patent-cliffs-and-what-theyre-doing-about-it
- Blockbuster Drugs on Patent Cliffs Research Report 2025 | – GlobeNewswire, accessed August 2, 2025, https://www.globenewswire.com/news-release/2025/07/28/3122199/0/en/Blockbuster-Drugs-on-Patent-Cliffs-Research-Report-2025-2030-Patent-Cliff-to-Be-Largest-Since-2010-Hitting-Blockbusters-Like-Keytruda-Eliquis-and-Darzalex.html
- The top 15 blockbuster patent expirations coming this decade – Fierce Pharma, accessed August 2, 2025, https://www.fiercepharma.com/special-report/top-15-blockbuster-patent-expirations-coming-decade
- Key drugs losing patent protection in 2025 | Pharma Manufacturing, accessed August 2, 2025, https://www.pharmamanufacturing.com/home/article/55249347/key-drugs-losing-patent-protection-in-2025
- The top 10 drugs losing US exclusivity in 2025 – Fierce Pharma, accessed August 2, 2025, https://www.fiercepharma.com/special-reports/top-10-drugs-losing-us-exclusivity-2025
- A 2025 Update on Expiring Marketing Patents, New Generics – U.S. Pharmacist, accessed August 2, 2025, https://www.uspharmacist.com/article/a-2025-update-on-expiring-marketing-patents-new-generics
- Life sciences: Primed for an increase – McKinsey, accessed August 2, 2025, https://www.mckinsey.com/capabilities/m-and-a/our-insights/life-sciences-primed-for-an-increase
- Pulse check: Key trends shaping biopharma dealmaking in 2025 – McKinsey, accessed August 2, 2025, https://www.mckinsey.com/industries/life-sciences/our-insights/the-synthesis/pulse-check-key-trends-shaping-biopharma-dealmaking-in-2025
- Biotechnology Industry Outlook 2025: Key Data & Innovations – StartUs Insights, accessed August 2, 2025, https://www.startus-insights.com/innovators-guide/biotechnology-industry-outlook/
- BioTech 2025: Key Trends, Innovations, and Challenges Shaping the Future, accessed August 2, 2025, https://biotechbreakthroughawards.com/biotech-2025-key-trends-innovations-and-challenges-shaping-the-future/
- What We’re Watching Ahead of BIO 2025: Trends Shaping the Future of Biotech | JD Supra, accessed August 2, 2025, https://www.jdsupra.com/legalnews/what-we-re-watching-ahead-of-bio-2025-1625448/
- 2025 predictions: Which trends are set to shape the biotech industry this year?, accessed August 2, 2025, https://www.labiotech.eu/in-depth/biotech-trends-2025/
- Five Key Trends Shaping Biopharma and Biotech in 2025 – PPD, accessed August 2, 2025, https://www.ppd.com/blog/2025-biopharma-biotech-trends/
- Antibody Drug Conjugates Market Share & Forecast, 2025-2032, accessed August 2, 2025, https://www.coherentmarketinsights.com/market-insight/antibody-drug-conjugates-market-181
- The future of mRNA vaccines beyond COVID-19 | CAS, accessed August 2, 2025, https://www.cas.org/resources/cas-insights/future-mrna-vaccines
- 2025 Biotech Economics: CROs, Advanced Therapies & Trends in Funding, accessed August 2, 2025, https://www.precisionformedicine.com/blog/2025-biotech-economics-cros-advanced-therapies-trends-in-funding
- The State of Biotechnology in 2025: Innovations and Trends | UF Medical Physiology Online, accessed August 2, 2025, https://distance.physiology.med.ufl.edu/the-state-of-biotechnology-in-2025-innovations-and-trends/
- AI in Drug Discovery Market Size to Worth USD 16.52 Bn by 2034 – BioSpace, accessed August 2, 2025, https://www.biospace.com/press-releases/ai-in-drug-discovery-market-size-to-worth-usd-16-52-bn-by-2034
- Artificial Intelligence (AI) In Drug Discovery Market Size, Share, and Trends 2025 to 2034, accessed August 2, 2025, https://www.precedenceresearch.com/artificial-intelligence-in-drug-discovery-market
- How 2025 can be a pivotal year of progress for Biopharma | World Economic Forum, accessed August 2, 2025, https://www.weforum.org/stories/2025/01/2025-can-be-a-pivotal-year-of-progress-for-pharma/
- AI in Pharma and Biotech: Market Trends 2025 and Beyond, accessed August 2, 2025, https://www.coherentsolutions.com/insights/artificial-intelligence-in-pharmaceuticals-and-biotechnology-current-trends-and-innovations
- AI in the Pharmaceutical Industry [5 Success Stories][2025] – DigitalDefynd, accessed August 2, 2025, https://digitaldefynd.com/IQ/ai-in-pharmaceutical-industry/
- In 2024, AI-Discovered Drugs Are Showing Remarkably High Success Rates in Early Clinical Trials – Pivotal AI, accessed August 2, 2025, https://pivot-al.ai/blog/articles/in-2024-ai-discovered-drugs-are-showing-remarkably-high-success-rates-in-early-clinical-trials
- 10 Case Studies of Successful Implementation of AI in Healthcare, accessed August 2, 2025, https://scimedian.in/10-case-studies-of-successful-implementation-of-ai-in-healthcare/
- Moderna trims digital team, lays off employees as chief information officer departs, accessed August 2, 2025, https://www.fiercepharma.com/pharma/moderna-trims-digital-team-lays-employees-chief-information-officer-departs
- From One-Size to Custom-Fit: The Transition from Blockbuster Drugs to Personalized Medicine in Rare Disease Care – TrialHub, accessed August 2, 2025, https://trialhub.com/resources/articles/from-one-size-to-custom-fit-the-transition-from-blockbuster-drugs-to-personalized-medicine-in-rare-disease-care
- Personalized Medicine Market Size to Increase USD 1,315.43 Billion by 2034 – BioSpace, accessed August 2, 2025, https://www.biospace.com/press-releases/personalized-medicine-market-size-to-increase-usd-1-315-43-billion-by-2034
- Precision Medicine Trends 2025: Top 6 Powerful Positive Shifts, accessed August 2, 2025, https://lifebit.ai/blog/precision-medicine-trends-2025/
- Discover the Top 10 Trends in Precision Medicine [2025] – StartUs Insights, accessed August 2, 2025, https://www.startus-insights.com/innovators-guide/trends-in-precision-medicine/
- Antibody Drug Conjugate Market Size, Key Players, Pipelines and Partnerships, accessed August 2, 2025, https://www.towardshealthcare.com/insights/antibody-drug-conjugate-market-sizing
- Introduction to Antibody-Drug Conjugates – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC8628511/
- A comprehensive overview on antibody-drug conjugates: from the conceptualization to cancer therapy – Frontiers, accessed August 2, 2025, https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1274088/full
- Antibody Drug Conjugates Market Reaching US$ 34.7 Billion By 2032, accessed August 2, 2025, https://media.market.us/antibody-drug-conjugates-market-news/
- Antibody–Drug Conjugates: The Dynamic Evolution from … – MDPI, accessed August 2, 2025, https://www.mdpi.com/2072-6694/16/2/447
- Antibody–Drug Conjugates: The Dynamic Evolution from Conventional to Next-Generation Constructs – PMC – PubMed Central, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10814585/
- Antibody–Drug Conjugates—Evolution and Perspectives – PMC – PubMed Central, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11241239/
- 10 Life Science and Biotech Trends to Watch in 2025 – Thermo Fisher Scientific, accessed August 2, 2025, https://www.thermofisher.com/blog/life-in-the-lab/10-life-science-trends-to-watch-in-2024/
- mRNA therapies: Pioneering a new era in rare genetic disease …, accessed August 2, 2025, https://pubmed.ncbi.nlm.nih.gov/38580137/
- Applications for mRNA – TriLink BioTechnologies, accessed August 2, 2025, https://www.trilinkbiotech.com/applications-for-mrna
- Unleashing the potential of mRNA therapeutics for inherited neurological diseases – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11969220/
- Opportunities and Challenges in the Delivery of mRNA-Based Vaccines – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC7076378/
- Unleashing the potential of mRNA therapeutics for inherited neurological diseases | Brain, accessed August 2, 2025, https://academic.oup.com/brain/article/147/9/2934/7658372
- Lipid nanoparticle-based mRNA vaccines: a new frontier in precision oncology – Oxford Academic, accessed August 2, 2025, https://academic.oup.com/pcm/article/7/3/pbae017/7725808
- Lipid Nanoparticle-Based Delivery System A Competing Place for mRNA Vaccines | ACS Omega, accessed August 2, 2025, https://pubs.acs.org/doi/10.1021/acsomega.3c08353
- Nonviral targeted mRNA delivery: principles, progresses, and challenges – PubMed, accessed August 2, 2025, https://pubmed.ncbi.nlm.nih.gov/39760110/
- Recent Advances in the Lipid Nanoparticle-Mediated Delivery of …, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC10059764/
- Fierce Biotech Layoff Tracker 2025, accessed August 2, 2025, https://www.fiercebiotech.com/biotech/fierce-biotech-layoff-tracker-2025
- Arcturus stops work on early-stage vaccine programs in effort to ‘streamline resources’ – Fierce Biotech, accessed August 2, 2025, https://www.fiercebiotech.com/biotech/arcturus-stops-work-early-stage-vaccine-programs-effort-streamline-resources
- Cell and gene therapy market set to grow at 44% CAGR through 2030 – PharmaLive, accessed August 2, 2025, https://www.pharmalive.com/cell-and-gene-therapy-market-set-to-grow-at-44-cagr-through-2030/
- CAR T Cells: Engineering Immune Cells to Treat Cancer – NCI, accessed August 2, 2025, https://www.cancer.gov/about-cancer/treatment/research/car-t-cells
- CAR-T ups challenges in pharma supply chain | BioPharma Dive, accessed August 2, 2025, https://www.biopharmadive.com/news/car-t-supply-chain-cell-therapy-challenges-pharma/521560/
- Mechanism, Challenges, and Progresses of Chimeric Antigen Receptors T-cell Cancer Therapy – Scientific Archives, accessed August 2, 2025, https://www.scientificarchives.com/article/mechanism-challenges-and-progresses-of-chimeric-antigen-receptors-t-cell-cancer-therapy
- Long-Term (≥5-Year) Remission and Survival After Treatment With Ciltacabtagene Autoleucel in CARTITUDE-1 Patients With Relapsed/Refractory Multiple Myeloma – ASCO Publications, accessed August 2, 2025, https://ascopubs.org/doi/10.1200/JCO-25-00760
- Generation of CAR-T Cells for Cancer Immunotherapy | Springer Nature Experiments, accessed August 2, 2025, https://experiments.springernature.com/articles/10.1007/978-1-4939-8885-3_24
- Press Release Service: CAR-T Cell Therapy Market Research 2024-2025: Size, Forecasts, Trials, and Trends, accessed August 2, 2025, https://crisprmedicinenews.com/press-release-service/card/car-t-cell-therapy-market-research-2024-2025-size-forecasts-trials-and-trends-approved-car-t-t/
- Promises and challenges of a decentralized CAR T-cell manufacturing model – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11235344/
- Challenges for the Commercialization of Cell & Gene Therapy …, accessed August 2, 2025, https://www.techsciresearch.com/blog/challenges-for-the-commercialization-of-cell-gene-therapy-products/1307.html
- 7 Common Cell and Gene Therapy Manufacturing Challenges (and How To Solve Them), accessed August 2, 2025, https://pharmasource.global/content/expert-insight/7-common-cell-and-gene-therapy-manufacturing-challenges-and-how-to-solve-them/
- High Cost of Chimeric Antigen Receptor T-Cells: Challenges and Solutions, accessed August 2, 2025, https://ascopubs.org/doi/10.1200/EDBK_397912
- The High Cost to Manufacture Cures | Eureka blog – Charles River Laboratories, accessed August 2, 2025, https://www.criver.com/eureka/high-cost-manufacture-cures
- Exploring the Truth of Reimbursement Challenges for Cell and Gene Therapies – Trinity Life Sciences, accessed August 2, 2025, https://trinitylifesciences.com/wp-content/uploads/2021/05/Trinity_Reimbursement_Challenges-6.10.19-1.pdf
- CAR-T Reimbursement Updates Proposed for FY 2024 | Avalere Health Advisory, accessed August 2, 2025, https://advisory.avalerehealth.com/insights/car-t-reimbursement-updates
- Why is CAR-T therapy so expensive? – Cell Guidance Systems, accessed August 2, 2025, https://www.cellgs.com/blog/why-is-car-t-therapy-so-expensive.html
- What is CRISPR: Your Ultimate Guide | Synthego, accessed August 2, 2025, https://www.synthego.com/learn/crispr
- How does CRISPR work? – Live Science, accessed August 2, 2025, https://www.livescience.com/58790-crispr-explained.html
- What is CRISPR-Cas9? – Your Genome, accessed August 2, 2025, https://www.yourgenome.org/theme/what-is-crispr-cas9/
- Questions and Answers about CRISPR | Broad Institute, accessed August 2, 2025, https://www.broadinstitute.org/what-broad/areas-focus/project-spotlight/questions-and-answers-about-crispr
- CRISPR gene editing – Wikipedia, accessed August 2, 2025, https://en.wikipedia.org/wiki/CRISPR_gene_editing
- What are genome editing and CRISPR-Cas9?: MedlinePlus Genetics, accessed August 2, 2025, https://medlineplus.gov/genetics/understanding/genomicresearch/genomeediting/
- Advancing CRISPR genome editing into gene therapy clinical trials: progress and future prospects – PMC – PubMed Central, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/
- Overview CRISPR Clinical Trials 2025 – CRISPR Medicine News, accessed August 2, 2025, https://crisprmedicinenews.com/clinical-trials/
- Vertex and CRISPR Therapeutics Present New Data in 22 Patients With Greater Than 3 Months Follow-Up Post-Treatment With Investigational CRISPR/Cas9 Gene-Editing Therapy, CTX001™ at European Hematology Association Annual Meeting, accessed August 2, 2025, https://crisprtx.com/about-us/press-releases-and-presentations/vertex-and-crispr-therapeutics-present-new-data-in-22-patients-with-greater-than-3-months-follow-up-post-treatment-with-investigational-crispr-cas9-gene-editing-therapy-ctx001-at-european-hematology-association-an
- Stable growth continues in the life sciences VC market – Grant Thornton, accessed August 2, 2025, https://www.grantthornton.com/insights/articles/life-sciences/2025/life-sciences-vc-market
- Navigating biotech investment cycles — the true north: Guest Commentary – BioCentury, accessed August 2, 2025, https://www.biocentury.com/article/654643/navigating-biotech-investment-cycles-the-true-north-guest-commentary
- Biotech 2025 Funding Squeeze, How to Navigate – BioBridge Global, accessed August 2, 2025, https://biobridgeglobal.org/industry/navigating-the-2025-biotech-funding-squeeze/
- Resurging Funding Catapults APAC Biotech Startups – BioSpectrum Asia, accessed August 2, 2025, https://www.biospectrumasia.com/analysis/26/26425/resurging-funding-catapults-apac-biotech-startups.html
- Evaluate Issues Annual World Preview Report, accessed August 2, 2025, https://www.pharmaceuticalcommerce.com/view/evaluate-issues-annual-world-preview-report
- Understanding Pharmaceutical Competitor Analysis – DrugPatentWatch, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/the-importance-of-pharmaceutical-competitor-analysis/
- Role of Competitive Intelligence in Pharma and Healthcare Sector, accessed August 2, 2025, https://www.delveinsight.com/blog/competitive-intelligence-in-healthcare-sector
- Competitive Intelligence Case Studies – Aquest Consulting | Commercial Strategy for Global Biopharma, accessed August 2, 2025, https://www.aquestconsulting.com/case-studies/competitive-intelligence-case-studies/
- DrugPatentWatch | Software Reviews & Alternatives – Crozdesk, accessed August 2, 2025, https://crozdesk.com/software/drugpatentwatch
- The Strategic Value of Orange Book Data in Pharmaceutical Competitive Intelligence, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/the-strategic-value-of-orange-book-data-in-pharmaceutical-competitive-intelligence/
- Cracking the Code: Using Drug Patents to Reveal Competitor Formulation Strategies, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/cracking-the-code-using-drug-patents-to-reveal-competitor-formulation-strategies/
- Understanding FDA Cell and Gene Therapy Guidance – Synthego, accessed August 2, 2025, https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance
- Cellular & Gene Therapy Products – FDA, accessed August 2, 2025, https://www.fda.gov/vaccines-blood-biologics/cellular-gene-therapy-products
- Cellular & Gene Therapy Guidances – FDA, accessed August 2, 2025, https://www.fda.gov/vaccines-blood-biologics/biologics-guidances/cellular-gene-therapy-guidances
- Cell and Gene Therapies Face Manufacturing Challenges – BioPharm International, accessed August 2, 2025, https://www.biopharminternational.com/view/cell-and-gene-therapies-face-manufacturing-challenges
- www.pharmafocusamerica.com, accessed August 2, 2025, https://www.pharmafocusamerica.com/articles/challenges-opportunities-cell-gene-therapy-manufacturing#:~:text=The%20widespread%20use%20of%20cell,enhance%20capability%20and%20reduce%20expense.
- A Pharmacist’s Guide to Blockbuster Patent Expirations: 2025 and Beyond, accessed August 2, 2025, https://www.pharmacytimes.com/view/a-pharmacist-s-guide-to-blockbuster-patent-expirations-2025-and-beyond
- The Impact of Patent Expiry on Drug Prices: A Systematic Literature Review – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC6132437/
- List – 65 Drug Patents Expiring in 2025 – GreyB, accessed August 2, 2025, https://www.greyb.com/blog/drug-patents-expiring-2025/
- Drug Patent Expirations for the Week of July 27, 2025 – DrugPatentWatch, accessed August 2, 2025, https://www.drugpatentwatch.com/blog/drug-patent-expirations-for-the-week-of-july-27-2025/
- United States: These 37 Drugs Face Patent Expirations and Generic Entry From 2025 – 2026, accessed August 2, 2025, https://www.drugpatentwatch.com/p/expiring-drug-patents-generic-entry/
- The Future of Biotech – Office of the Director of National Intelligence – Global Trends, accessed August 2, 2025, https://www.dni.gov/index.php/gt2040-home/gt2040-deeper-looks/future-of-biotech
- What to expect in US healthcare in 2025 and beyond | McKinsey, accessed August 2, 2025, https://www.mckinsey.com/industries/healthcare/our-insights/what-to-expect-in-us-healthcare-in-2025-and-beyond
- Pharma industry to outdo India Inc in 2025 pay hike: Study, accessed August 2, 2025, https://economictimes.indiatimes.com/industry/healthcare/biotech/pharmaceuticals/pharma-industry-to-outdo-india-inc-in-2025-pay-hike-study/articleshow/123010749.cms
- Imfinzi granted Priority Review and Breakthrough Therapy Designation in the US for patients with resectable early-stage gastric and gastroesophageal junction cancers – AstraZeneca, accessed August 2, 2025, https://www.astrazeneca.com/media-centre/press-releases/2025/imfinzi-granted-priority-review-and-breakthrough-therapy-designation-us-patients-with-resectable-early-stage-gastric-gastroesophageal-junction-cancers.html
- Transforming Cancer Care: A Narrative Review on Leveraging …, accessed August 2, 2025, https://www.mdpi.com/2077-0383/14/15/5346
- CRISPR Clinical Trials to Follow – Synthego, accessed August 2, 2025, https://www.synthego.com/blog/crispr-clinical-trials
- New gene-editing therapy shows early success in fighting advanced GI cancers, accessed August 2, 2025, https://www.sciencedaily.com/releases/2025/05/250502133947.htm
- Finance Pipeline Business Appendices – Sanofi, accessed August 2, 2025, https://www.sanofi.com/assets/dotcom/content-app/events/quaterly-results/2025/2025-q2-2025-results/2025_07_31_Sanofi_Q2_2025_Results.pdf
- LIFE SCIENCES INDUSTRY REPORT 2025 – pharmaphorum, accessed August 2, 2025, https://pharmaphorum.com/sites/default/files/2025-01/Life%20Sciences%20Industry%20Report%202025%20pt1%20v10.pdf
- The Global Use of Medicines Outlook Through 2029 – IQVIA, accessed August 2, 2025, https://www.iqvia.com/insights/the-iqvia-institute/reports-and-publications/reports/the-global-use-of-medicines-outlook-through-2029
- Vision 2030: patient services and support in the healthcare market of the future – IQVIA, accessed August 2, 2025, https://www.iqvia.com/library/white-papers/vision-2030-patient-services-and-support-in-the-healthcare-market-of-the-future
- Pharma Industry Outlook: Where is the Growth? – DCAT Value Chain Insights, accessed August 2, 2025, https://www.dcatvci.org/features/pharma-industry-outlook-where-is-the-growth/
- Cell And Gene Therapy Manufacturing Market Report, 2030 – Grand View Research, accessed August 2, 2025, https://www.grandviewresearch.com/industry-analysis/cell-gene-therapy-manufacturing-market
- Cell and gene therapy market set to grow at 31.3% CAGR through 2030, forecasts GlobalData, accessed August 2, 2025, https://www.globaldata.com/media/pharma/cell-gene-therapy-market-set-grow-31-3-cagr-2030-forecasts-globaldata/
- Mechanism of action of CAR T-cell therapy. Patient’s T cells are …, accessed August 2, 2025, https://www.researchgate.net/figure/Mechanism-of-action-of-CAR-T-cell-therapy-Patients-T-cells-are-collected-by_fig1_318693671
- Overview of Multiple Myeloma – CancerNetwork, accessed August 2, 2025, https://www.cancernetwork.com/view/overview-of-multiple-myeloma
- IL-10-expressing CAR T cells resist dysfunction and mediate durable clearance of solid tumors and metastases – Nature Biotechnology : r/science – Reddit, accessed August 2, 2025, https://www.reddit.com/r/science/comments/18ynuf3/il10expressing_car_t_cells_resist_dysfunction_and/
- mRNA therapies: Pioneering a new era in rare genetic disease treatment – OUCI, accessed August 2, 2025, https://ouci.dntb.gov.ua/en/works/ldGG6rm4/
- AI in Pharma: Use Cases, Success Stories, and Challenges in 2025, accessed August 2, 2025, https://scw.ai/blog/ai-in-pharma/
- The AI advantage in discovering new medicines – Clinical Trials Arena, accessed August 2, 2025, https://www.clinicaltrialsarena.com/features/the-ai-advantage-in-discovering-new-medicines/
- AI In Action: Redefining Drug Discovery and Development – PMC, accessed August 2, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC11800368/