Executive Summary
The pharmaceutical industry faces persistent challenges characterized by escalating costs, protracted development timelines, and low success rates for new drug candidates. This report explores “permissionless R&D” as a potentially transformative paradigm to address these systemic inefficiencies, contrasting it with the current highly regulated landscape. Permissionless innovation, defined by open participation and the elimination of gatekeepers, offers significant promise for accelerating drug discovery, reducing exorbitant development costs, and enhancing global drug accessibility. However, its implementation in the life sciences necessitates a meticulous consideration of profound challenges related to patient safety, product quality, ethical conduct, intellectual property rights, and liability. The analysis presented herein argues for a balanced, hybrid approach that strategically integrates elements of permissionless innovation within a robust, modernized regulatory framework to foster innovation while rigorously upholding public health safeguards.
1. Introduction: The Imperative for Innovation in Pharmaceutical R&D
The pharmaceutical sector is at a critical juncture, grappling with fundamental inefficiencies that impede the timely and affordable delivery of new therapies. Developing a novel drug is an extraordinarily capital-intensive and time-consuming endeavor, with costs often exceeding $800 million.1 Furthermore, the success rate for drug candidates entering clinical trials is remarkably low, with only about 10% ultimately achieving regulatory approval. This attrition is frequently driven by safety concerns or a lack of efficacy observed during development.3 This escalating inefficiency, where the cost of developing and approving a new drug roughly doubles every nine years, is often referred to as “Eroom’s Law”.5 This persistent trend of increasing inefficiency creates an inherent and pressing need for the industry to explore and adopt radically new R&D models. The current permissioned status quo, despite its critical safeguards, is becoming economically unsustainable, compelling the industry to consider disruptive approaches to maintain its long-term viability and meet the ever-growing global health demands.
In response to these systemic pressures, the concept of “permissionless innovation” has emerged as a potential pathway forward.6 This principle, rooted in the freedom to experiment and build without requiring prior approval, champions an environment where creativity and progress can accelerate by reducing centralized control and fostering broad participation.6 However, the application of such a paradigm within the highly sensitive domain of pharmaceutical R&D presents a fundamental philosophical divergence. Policy debates often center on whether to permit new developments until harm is proven, or to require proof of safety before any new innovation is allowed.8 The pharmaceutical industry, by its very nature, deals with human health and potentially irreversible outcomes, leading it to historically lean heavily on the latter, the “precautionary principle.” Introducing permissionless R&D directly challenges this deeply ingrained mindset, suggesting a societal and policy re-evaluation of risk tolerance. Embracing permissionless R&D in pharma would necessitate a significant cultural and legal paradigm shift, moving from a “prove no harm” stance to one that allows innovation until harm is demonstrated. This shift carries profound consequences for public trust, regulatory adaptation, and the very definition of responsible innovation in healthcare.
2. Defining Permissionless R&D in the Pharmaceutical Context
Core Principles of Permissionless Innovation
At its essence, permissionless innovation signifies an environment where anyone can participate and build without needing to meet predefined conditions or seek prior approval from a central authority.6 This model aims to eliminate gatekeepers, thereby fostering ecosystems where innovation can flourish unhindered.6 In contrast to “permissioned” systems, where access is tightly controlled by sovereigns, licenses, or curated memberships, a permissionless environment emphasizes that opportunity is not granted but rather seized and built upon by those willing to act.7
Contrast with Traditional “Permissioned” Systems in Pharma
The pharmaceutical industry stands as a quintessential example of a “permissioned” system. Drug development is governed by a highly structured, multi-year approval cycle meticulously overseen by regulatory bodies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA).10 This process mandates extensive preclinical research, followed by multi-phase clinical trials, and culminates in rigorous review processes. Each stage requires explicit regulatory authorization, exemplified by the necessity of an Investigational New Drug (IND) application before any human trials can commence.11 This stringent oversight is designed to ensure the safety, efficacy, and quality of pharmaceutical products before they reach the public.
Historical Examples from Other Industries
Permissionless innovation has historically served as a powerful catalyst for progress across various sectors, long predating the advent of the internet and blockchain technologies.7
- Early Internet and Web3: The foundational architects of the early internet deliberately designed it to be open and decentralized. This allowed individuals to connect, create, and exchange information without requiring approval from a central authority, a principle that fueled the explosive growth of the web.7 Similarly, contemporary decentralized technologies like blockchain and Web3 embody permissionless participation, enabling users to interact and transact without reliance on traditional intermediaries such as banks or corporations.7 The rapid emergence of decentralized finance (DeFi) platforms, including Uniswap and Aave, further illustrates the transformative power of this model, establishing financial markets that are accessible to any user at any time.7
- Software Development (APIs): The remarkable explosion of innovation within the IT industry, which led to the creation of hundreds of thousands of iOS and Android applications, is a direct consequence of permissionless innovation. This was primarily facilitated by the publication of Application Programming Interfaces (APIs), which allowed external developers to access and build upon core technologies without prior permission.1 This approach enables parallel experimentation, where diverse actors can launch their own projects independently, significantly accelerating the pace of invention and allowing a broader ecosystem to generate ideas that the original system designers might never have conceived.1
- Mining Industry (Goldcorp): A compelling example from a non-digital sector is the Canadian mining firm Goldcorp. Faced with underperforming mines and a lack of new gold deposits identified by its in-house geologists, Goldcorp’s CEO, inspired by the Linux operating system, took the unprecedented step of publicly releasing decades of proprietary geological data. He then challenged the global community to identify new gold deposits. This crowdsourcing initiative successfully led to the discovery of 110 new sites, half of which were previously unknown to Goldcorp, demonstrating how permissionless external contributions can unlock substantial value while the company retains its core intellectual property.1
The conceptualization of pharmaceutical innovations as “information goods” is a crucial underlying tenet. As highlighted, pharmaceutical R&D fundamentally involves the production of knowledge, encompassing both the discovery of new chemical or biological compounds and the comprehensive understanding of their safety and efficacy.18 The traditional “permissioned” system treats this information as proprietary and strictly controlled, thereby limiting its flow and broader utilization. Permissionless R&D, by advocating for open access to data 1, fundamentally shifts the paradigm of how this “information good” is generated, validated, and disseminated. This perspective suggests that if pharmaceutical innovation is indeed an “information good,” then the principles of open-source software and data sharing, which thrive on permissionless access to information, become highly relevant. This implies a potential for a more distributed, collaborative knowledge creation model, which could accelerate discovery by allowing more diverse perspectives and computational power to analyze and build upon existing data, potentially leading to breakthroughs that siloed approaches might miss.
However, a significant challenge arises in translating “digital” permissionless models to “physical” drug development. Many successful applications of permissionless innovation originate in digital realms, such as the internet, Web3, and software APIs, where the cost of experimentation is relatively low, iteration cycles are rapid, and errors are often reversible.1 In contrast, pharmaceutical R&D involves the manipulation of physical compounds, complex biological systems, and human clinical trials. These processes are inherently high-cost, high-risk, and slow, with irreversible patient safety consequences.3 The core challenge is not merely whether permissionless principles can be applied, but precisely how they can be adapted to a domain with such significant physical constraints, substantial capital requirements, and critical human safety implications. A pure, unfettered “permissionless” model, as observed in software development, is unlikely to be directly transferable to pharmaceuticals. Instead, it will necessitate substantial adaptation, the adoption of hybrid approaches, and the development of new, possibly technology-driven, safeguards to effectively manage the inherent risks associated with physical and biological experimentation.
3. The Case for Permissionless R&D: Benefits and Opportunities
3.1 Accelerating Discovery and Development
Permissionless R&D offers compelling advantages in accelerating the pace of drug discovery and development.
- Parallel Experimentation and Speed: By enabling multiple actors to initiate their own research endeavors without waiting for the outcomes of others, permissionless innovation fosters parallel experimentation, significantly increasing the speed of invention.1 This stands in stark contrast to the linear, sequential nature characteristic of traditional drug development.11 The removal of gatekeepers creates environments conducive to rapid innovation, thereby accelerating overall progress.6
- Leveraging External Expertise and “Abandoned Compounds”: Pharmaceutical companies frequently discard compounds that show limited promise for their initial intended use, often representing “Type 2 errors” where potential value is overlooked.1 Permissionless models advocate for opening these “tapped-out mines” or abandoned compounds to external parties.1 Third parties possessing specialized knowledge can identify new indications or applications that large pharmaceutical companies might miss.1 Notable examples include Viagra, initially investigated as a hypertension drug but later found effective for erectile dysfunction, and Cubicin, an antibiotic abandoned by Eli Lilly due to toxicity, which was subsequently developed by a smaller firm into a successful treatment for antibiotic-resistant staphylococcus.1 This approach effectively taps into a broader ecosystem of ideas that the original developers might not have conceived.1 This “Viagra Effect” illustrates a fundamental inefficiency in traditional R&D: the “false negative” problem. Companies, operating within a permissioned, target-driven framework, often discard compounds that do not meet initial criteria, even if they possess latent therapeutic value for other conditions. Permissionless R&D, by opening up data and compounds to a broader community, creates a mechanism for external, diverse perspectives to re-evaluate these discarded assets. This suggests a significant untapped resource within the pharmaceutical industry’s existing archives of “failed” or abandoned compounds. Permissionless models are uniquely positioned to exploit this, potentially leading to new revenue streams for companies and new treatment options for patients from previously “lost” investments, effectively transforming R&D failures into future successes.
- Open Access to Data, APIs, and Computational Models: Drawing lessons from the IT industry, the pharmaceutical sector can modularize complex technologies and utilize open APIs to facilitate external access to data and compounds.1 Providing open access to preclinical and clinical data on specific compounds, sharing assays that approximate therapeutic benefit, and making computational models widely available can invite third parties to explore new applications and variations.1 This “part open, part closed” governance structure allows companies to retain their patents while benefiting from external innovation.1
3.2 Cost Reduction and Efficiency Gains
Permissionless R&D offers avenues for significant cost reduction and efficiency improvements.
- Decentralized Clinical Trials (DCTs): DCTs are revolutionizing clinical research by shifting activities away from traditional clinical sites. They leverage digital tools such as telehealth consultations, wearable health monitoring devices, mobile applications for data collection, and direct-to-patient drug delivery.20 These trials enhance patient accessibility and diversity while improving data collection methodologies.20 Crucially, DCTs streamline patient recruitment, reduce site overhead costs, and minimize administrative burdens associated with conventional trials. This leads to faster trial timelines, with reported reductions of up to 30%, and substantial cost savings, potentially yielding financial benefits up to five times greater than the upfront investment for Phase 2 studies, and up to 14 times for Phase 3 studies.20 The adoption of DCTs can be viewed as a “Trojan Horse” for permissionless principles. While DCTs are implemented within the existing regulatory framework, their core mechanisms—remote participation, digital tools, reduced physical site visits, and patient-centricity—inherently embody elements of permissionlessness by reducing physical gatekeepers and central control points for patient interaction and data collection. This demonstrates that the industry and regulatory bodies are already, perhaps implicitly, adopting permissionless principles in areas where efficiency gains and patient convenience are undeniable. This controlled decentralization in trials could pave the way for broader acceptance and integration of similar concepts across the entire R&D pipeline, demonstrating that permissionless elements can be integrated without sacrificing oversight.
- Model-Informed Drug Development (MIDD): MIDD involves integrating data to quantify benefit/risk, thereby informing objective drug discovery and development decisions and enhancing trial and program efficiencies.22 The systematic application of MIDD can result in annualized average savings of approximately 10 months of cycle time and $5 million per program.22
- Prize-Based Systems and Open Innovation: Moving beyond sole reliance on patent monopolies, prize-based systems for drug development could incentivize innovation while simultaneously allowing for competitive generic production, potentially reducing costs and increasing affordability.23 This aligns with the “part open, part closed” model, where prizes could be awarded for external contributions.1 This approach encourages broader participation in the open aspects of technology, allowing for a proliferation of innovative ideas.1 The economic incentive for openness extends beyond altruism. While open-source drug discovery (OSDD) is often framed around “affordable healthcare for all” 24, and adaptive R&D addresses the needs of low- and middle-income countries (LMICs) 25, examples like Goldcorp 1 and the “part open, part closed” model 1 reveal a strong economic rationale for permissionless approaches. Companies can retain patents and control over monetization while leveraging external innovation to reduce their own R&D burden, discover new indications, and uncover new market opportunities. This highlights that the argument for permissionless R&D is not solely ethical or access-driven but also a pragmatic business case for openness. Profit-driven pharmaceutical companies can significantly benefit from strategically embracing permissionless elements, as it allows them to externalize certain R&D risks and costs, access a wider pool of talent, and potentially unlock new revenue streams from existing assets.
3.3 Enhancing Drug Accessibility and Addressing Unmet Needs
Permissionless R&D models hold significant potential for enhancing drug accessibility and addressing critical unmet medical needs.
- Addressing Global Health Disparities: The current R&D system frequently falls short in adequately addressing the health needs of the majority of the global population, particularly in low- and middle-income countries (LMICs), where challenges related to affordability and sustainable R&D financing are pronounced.23 Permissionless and open-source approaches can foster drug discovery for neglected tropical diseases, such as leishmaniasis, which often receive limited attention from traditional research-based pharmaceutical companies.24
- Adaptive R&D: Pharmaceutical companies are increasingly engaging in adaptive R&D, which involves modifying existing medicines—for instance, developing new formulations, fixed-dose combinations, repurposing for new indications, or creating versions for specific age groups like pediatric populations—to better suit the unique needs of LMICs.25 This strategy has the potential to bridge significant R&D gaps by producing more appropriate and accessible medicines for these populations.25 However, while access plans for these projects exist, they often lack comprehensive strategies for ensuring affordability and widespread availability post-launch, frequently focusing predominantly on registration plans with limited geographical reach.25
- Open-Source Drug Discovery (OSDD): Initiatives such as India’s Council of Scientific and Industrial Research (CSIR)-led OSDD consortium exemplify collaborative drug discovery for neglected diseases, driven by the motto “Affordable healthcare for all”.24 OSDD leverages open-source philosophy, crowdsourcing, and web-based tools, including a Wiki-based portal for peer review, to stimulate innovation and discover novel therapies without traditional Intellectual Property (IP) restrictions, thereby making new drugs available as generics.24 This model effectively blends patenting with open-source research principles, aiming to ensure both affordability and accessibility.24
- Citizen Science: Engaging citizen scientists can significantly democratize science, expand medical knowledge, and contribute to the development of new treatments.27 Individuals can actively participate in defining research questions, collecting data (e.g., through smartphone applications for environmental health monitoring), and interpreting findings, particularly for population health issues.27 This approach empowers marginalized groups and can accelerate the matching of patients with researchers by providing easily accessible technology platforms for collaboration.28
4. Navigating the Complexities: Risks and Challenges of a Permissionless Model
While the potential benefits of permissionless R&D in pharmaceuticals are considerable, its implementation introduces significant complexities and risks that necessitate careful consideration and robust mitigation strategies.
4.1 Patient Safety and Efficacy Concerns
The paramount concern in pharmaceutical development is patient safety and ensuring the efficacy of new treatments.
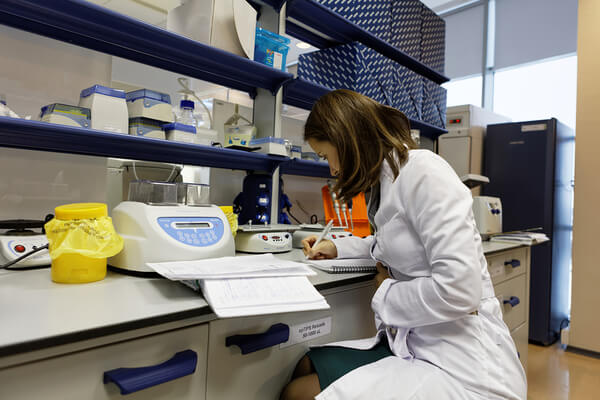
- Critical Role of Regulatory Oversight: Current regulatory bodies, such as the FDA and EMA, are specifically designed to safeguard the rights and well-being of human subjects and to ensure the scientific rigor and quality of drug evaluations.16 The established drug development process mandates rigorous preclinical and multi-phase clinical research (Phase 1, 2, 3) to meticulously test for safety and efficacy, supported by strict monitoring and comprehensive data review.11 Institutional Review Boards (IRBs) play a crucial role, being legally empowered to approve, require modifications in, or disapprove research protocols to ensure that study participants are not exposed to unnecessary risks and that the potential benefits of a study outweigh any potential harms.29 This oversight extends to the review of unanticipated problems and adverse events that may arise during trials.31
- Risks of Inadequate Testing and Monitoring: A less regulated environment, by potentially lowering the “bar for new treatments,” could lead to a higher incidence of drug safety issues.3 Without stringent oversight, there is an increased risk of insufficient target validation, a lack of predictive preclinical models, and the absence of appropriate biomarkers, all of which contribute to higher clinical trial failure rates or, more critically, the approval of ineffective or unsafe drugs.3 The World Health Organization’s (WHO) “Medication Without Harm” initiative underscores the substantial global cost—estimated at $42 billion annually—and the severe patient harm associated with unsafe medication practices and errors, often stemming from weak medication systems or human factors.32
- Lack of Reproducibility: The current R&D landscape already contends with a significant “lack of reproducibility of published information,” with an estimated annual economic impact of $28 billion in the USA alone attributed to preclinical research that cannot be replicated.3 A less regulated model, characterized by reduced oversight or diminished pressure for transparency and rigorous methodology, could exacerbate this problem. This would lead to an even greater waste of resources on flawed research and a severe erosion of confidence in scientific findings.3 This situation highlights a regulatory “catch-22” between speed and safety. While the slow, costly, and constrained nature of current approval cycles is often criticized 8, the necessity of rigorous regulation for patient safety, preventing “unanticipated problems” and “avoidable harm,” is paramount.3 This presents a fundamental dilemma: accelerating R&D by reducing “permission” inherently risks compromising safety. Therefore, any shift towards permissionless models must involve innovative solutions that can achieve both speed and safety, rather than sacrificing one for the other, potentially through novel forms of real-time monitoring and adaptive oversight.
4.2 Quality Control and Manufacturing Integrity
Maintaining stringent quality control and manufacturing integrity is a significant challenge, potentially exacerbated by a permissionless model.
- Challenges in Maintaining Standards: Traditional pharmaceutical manufacturing relies on tightly managed Quality Assurance (QA) and Quality Control (QC) processes within single, centralized facilities.34 In a decentralized or permissionless model, quality oversight could become fragmented, with responsibilities distributed among geographically dispersed personnel or even downstream users.34 This risks creating “bottom-heavy” systems that are overloaded with final checks but lack sufficient upstream process control.34 Such a shift also introduces variability in execution due to the diverse backgrounds and expertise of personnel operating in mobile or point-of-care units.34
- Risks of Poor Practices: Common factors contributing to low pharmaceutical quality include poor manufacturing practices (e.g., inadequate facility maintenance, lack of adherence to Standard Operating Procedures (SOPs), unqualified personnel, and inadequate or uncalibrated equipment), the use of substandard raw materials, incorrect formulation, and insufficient testing at all stages of production.35 Failures in quality control, often due to rushed processes, poor sampling, or unqualified personnel, can allow substandard products to enter the market.35
- Counterfeit Drugs: The proliferation of counterfeit drugs, which may contain incorrect or harmful ingredients, improper dosages, or lack efficacy, poses a significant public health threat, particularly in under-regulated markets.35 A permissionless model, without robust traceability, serialization, and real-time monitoring systems, could exacerbate this risk and hinder the effective detection and removal of such products.35 This concern points to a potential “tragedy of the commons” in unregulated quality. The numerous quality control challenges detailed—poor manufacturing practices, inadequate testing, unqualified personnel, supply chain issues, and counterfeit drugs 35—could worsen significantly. Without centralized “permission” and enforcement, there is a high risk that individual actors, driven by cost-cutting or the desire for speed, might compromise quality. This could lead to a systemic degradation of drug integrity, an increase in substandard or counterfeit products, and a severe erosion of patient and public trust in pharmaceutical products. This is not merely about isolated failures but a potential collapse of collective quality standards in the absence of a strong regulatory hand.
4.3 Ethical and Societal Implications
Ethical considerations are foundational to drug discovery and development, particularly concerning human subjects.
- Protection of Human Subjects and Informed Consent: Ethical principles, including autonomy, beneficence, nonmaleficence, and justice, serve as the guiding pillars for responsible research.38 Informed consent, which ensures that participants fully comprehend all potential risks and benefits and freely choose to participate or withdraw without repercussions, is a cornerstone of ethical research.38 Unregulated research could bypass these crucial protections, posing particular risks to vulnerable populations such as children, pregnant women, or individuals with cognitive impairments.38 Historical incidents, such as the U.S. Public Health Service Syphilis Study at Tuskegee, starkly illustrate the severe consequences of lacking informed consent and ethical oversight.30
- Data Privacy and Conflicts of Interest: Permissionless models that involve open data sharing raise substantial concerns regarding data security and privacy, especially for sensitive medical or genetic information.38 Mismanagement of such data could result in breaches or misuse.42 The commercial aspects inherent in drug development can create ethical dilemmas, particularly concerning conflicts of interest and the potential exploitation of research participants. In such scenarios, stakeholders must prioritize the welfare of patients over financial gains and ensure transparency in reporting research outcomes.38
- Societal Impact of Unregulated Products: The rapid development of “new psychoactive substances” (NPS), whose chemical structures are constantly modified to evade regulation, exemplifies the societal dangers of unregulated drug development. These untested products often lack recommended dosages and carry unknown risks, leading to potential harm.43 Similarly, the absence of adequate regulation in nascent fields like artificial intelligence (AI) in healthcare poses serious safety concerns if AI tools are misused.44 Public opinion and policy play a crucial role in shaping drug development norms, influencing aspects such as the call for greater diversity in clinical trials and increased concern for animal welfare.45 These concerns point to a potential “ethical vacuum” in unaccountable innovation. Ethical principles and mechanisms like informed consent and Institutional Review Board (IRB) review are foundational to human research in pharmaceuticals.38 Unregulated research risks bypassing these safeguards, potentially leading to the exploitation of vulnerable populations and severe harm, as evidenced by historical abuses.30 The danger is that permissionless R&D, if not carefully structured with explicit ethical frameworks and accountability mechanisms, could create an environment where the drive for rapid innovation outpaces the development of robust ethical oversight. This is particularly critical in pharmaceuticals, where human lives are directly at stake, and the potential for irreversible harm is high.
4.4 Intellectual Property and Liability Frameworks
The structure of intellectual property (IP) and liability is fundamental to pharmaceutical innovation.
- Balancing Innovation Incentives: The pharmaceutical industry relies more heavily on patent protection than virtually any other sector to incentivize the massive, long-term R&D investments required.18 Permissionless models, while promoting open access and collaboration, must carefully navigate how to ensure continued investment and appropriate reward for innovation.47 Debates persist regarding whether current IP models, particularly patent monopolies, hinder drug accessibility and affordability, especially in low- and middle-income countries (LMICs).23 For instance, recent legislative changes like the Inflation Reduction Act’s price controls are perceived by some as reducing incentives for small-molecule drug innovation.48
- AI and Inventorship: The increasing integration of Artificial Intelligence (AI) in drug discovery introduces novel intellectual property challenges. Recent legal decisions in the U.S. indicate that if AI is deemed the sole inventor of a drug, it might be ineligible for patenting, as the term “inventor” is legally defined as a natural person.49 This creates uncertainty regarding IP rights in AI-driven permissionless R&D, potentially impacting a pharmaceutical company’s ability to secure exclusive rights to a drug if AI significantly replaces human ingenuity in the discovery process.49
- Liability in Decentralized Models: Decentralized Autonomous Organizations (DAOs) and other permissionless structures challenge existing legal frameworks concerning participant liability.50 The blurring of liability boundaries, the anonymity of DAO participants, and the automatic execution of smart contracts complicate the traditional concept of legal liability, both within the DAO context and in interactions with external parties.50 While current legal precedent generally protects research funders from unlimited liability for alleged harms 51, a fully permissionless system could alter this dynamic by creating a “specter of limitless liability” for those involved, or, conversely, a lack of clear accountability for adverse outcomes, which could have a chilling effect on legitimate research.51 This situation presents a paradox of IP and openness, requiring a balance between incentivizing innovation and preventing monopolization. The pharmaceutical industry heavily relies on patents for R&D incentives, often being considered the “poster child for the patent system”.18 Permissionless models, however, advocate for openness and shared data.1 The central challenge is how to foster open, collaborative innovation, which might reduce individual firm IP control, while still providing sufficient financial incentives for the massive, risky investments required for drug development. Therefore, a “permissionless” IP model in pharma cannot simply abandon patents; it must innovate within or around existing IP frameworks, perhaps through novel licensing agreements, prize systems, or “viral clauses” 26, to balance the public good (access, affordability) with private incentive (profit, continued innovation). The emerging AI inventorship issue 49 further complicates this, raising fundamental questions about who owns the “permissionless” discovery when AI plays a significant role.
The following table provides a concise comparison of the benefits and risks associated with Traditional (Permissioned) R&D versus a potential Permissionless R&D model in the pharmaceutical industry.
Table 1: Comparison of Traditional vs. Permissionless R&D: Benefits and Risks
| R&D Aspect | Traditional (Permissioned) R&D | Permissionless R&D (Potential/Proposed) |
| Pace of Innovation | Slow, sequential, gatekeeper-dependent 10 | Accelerated, parallel experimentation, eliminates gatekeepers 1 |
| Development Cost | Extremely high (>$800M per drug), increasing (Eroom’s Law) 1 | Potential for significant cost reduction (e.g., via DCTs, MIDD, prize systems) 1 |
| Participant/Developer Access | Centralized, controlled access for approved entities 7 | Decentralized, open participation for anyone willing to act 6 |
| Regulatory Oversight | Rigorous ex-ante approval at multiple stages (IND, NDA/BLA) 11 | Minimal prior approval, potential for ex-post addressing of issues 8 |
| Patient Safety Assurance | High standards via extensive preclinical/clinical trials, IRB oversight, post-market monitoring 11 | Potential for inadequate testing, unforeseen adverse effects, lower safety bar 3 |
| Quality Control | Centralized QA/QC, strict SOPs, facility inspections 34 | Fragmented QC, potential for poor manufacturing practices, increased counterfeit risk 34 |
| Intellectual Property Model | Strong patent monopolies to incentivize R&D 18 | Open/shared IP (e.g., data, compounds), prize systems, “part open, part closed” models 1 |
| Liability Framework | Clear sponsor liability for product safety/efficacy 51 | Blurred/distributed liability, potential for “limitless liability” or lack of accountability 50 |
| Ethical Governance | Formal IRB review, informed consent, protection of vulnerable populations 29 | Community-driven/emerging ethics, risk of exploitation, data privacy breaches 38 |
5. The Current Regulatory Landscape and Pathways for Evolution
Overview of FDA and EMA Drug Approval Processes
The current global pharmaceutical landscape is defined by comprehensive regulatory frameworks, primarily governed by agencies such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA). These bodies meticulously oversee every stage of drug development to ensure safety, efficacy, and quality.
- FDA Process: The FDA’s drug development process is structured into five key steps: Discovery and Development, Preclinical Research, Clinical Research, FDA Drug Review, and Post-Market Drug Safety Monitoring.11 Research for a new drug typically begins in the laboratory during the Discovery and Development phase. This is followed by Preclinical Research, where drugs undergo laboratory and animal testing to address fundamental safety questions.11 Before human trials can commence, an Investigational New Drug (IND) application must be submitted to the FDA. This application requires detailed information, including animal study data, manufacturing information, clinical protocols, and any prior human research findings.12 Clinical Research then proceeds through three phases:
- Phase 1: Involves 20 to 100 healthy volunteers or patients to assess safety and dosage, typically lasting several months, with approximately 70% of drugs progressing.12
- Phase 2: Expands to several hundred patients to evaluate efficacy and side effects over several months to two years, with about 33% advancing.12
- Phase 3: Involves 300 to 3,000 volunteers with the target condition over one to four years, serving as pivotal studies to demonstrate treatment benefit and monitor adverse reactions, with 25-30% moving to the next phase.12
Upon successful completion of clinical trials, a New Drug Application (NDA) for small molecule drugs or a Biologics License Application (BLA) for biological products is submitted for marketing approval. These applications must demonstrate the drug’s safety, efficacy, quality, and purity.17 The FDA’s review teams thoroughly examine all submitted data before making an approval decision.11 Finally, Post-Market Drug Safety Monitoring (Phase 4) ensures ongoing surveillance of drug safety once products are available to the public.11 - EMA Process: The European Medicines Agency (EMA) primarily utilizes a centralized authorization procedure, allowing pharmaceutical companies to submit a single marketing-authorization application that covers all EU Member States and European Economic Area (EEA) countries.13 The EMA’s Committee for Medicinal Products for Human Use (CHMP) conducts a scientific assessment of the application and provides a recommendation on whether the medicine should be marketed. The European Commission then makes the final legally binding decision.13 Similar to the FDA, EMA’s process includes phased clinical trials (Phase I, II, III) to understand how medicines work and evaluate their benefits and side effects.13 The EMA also places significant emphasis on continuously monitoring risks associated with an authorized medicine, including requiring post-authorization safety studies.13
Regulatory Trends and Adaptations
Regulatory bodies are not static entities; they are actively adapting to new technologies and methodologies, demonstrating a willingness to evolve within their core mission of public health protection.
- Adaptive Trials and Faster Pathways: Despite some media reports suggesting widespread delays, the biopharmaceutical industry is largely maintaining or even increasing its R&D budgets, and actual FDA-related delays are less prevalent than often perceived.54 The FDA is meeting its Prescription Drug User Fee Act (PDUFA) approval decision targets.54 This indicates a more nuanced reality than headlines might suggest.
- Innovation in Clinical Trials: Regulatory bodies are actively embracing innovative trial designs. The US FDA, for example, published draft guidance on Master Protocols (e.g., umbrella, platform, and basket trials) to streamline drug development, emphasizing robust and unbiased results through concurrent control groups, randomization, and blinding.55 They are also closely monitoring the use of Bayesian Methodology in clinical trials and the field of Clinical Pharmacogenomics.55
- Artificial Intelligence (AI) Integration: The rapid proliferation of AI and Large Language Models (LLMs) in drug development and clinical research has garnered significant regulatory attention.55 The FDA published draft regulatory guidance on “Considerations for Use of Artificial Intelligence to Support Regulatory Decision-Making for Drug and Biological Products,” with a focus on developing a risk-based credibility assessment framework for AI models used in regulatory decision-making.55 AI tools are recognized for their potential to enhance R&D capabilities 56 and improve real-time drug efficacy monitoring.20
- Decentralized Clinical Trials (DCTs) Stance: Both the FDA and EMA are increasingly supportive of Decentralized Clinical Trials (DCTs). The FDA’s final guidance on DCTs clarifies requirements for remote participation, the use of digital health technologies, and the involvement of local healthcare providers, while emphasizing that DCTs are subject to the same rigorous regulatory requirements as traditional trials.57 The EMA highlights patient safety, patient and investigator inclusion, and the comprehensive evaluation of DCT risks and benefits.58 Hybrid clinical trials, which combine traditional and decentralized elements, are rapidly increasing in prevalence, exceeding traditional on-site trials in recent years.59 This regulatory modernization represents a de facto embrace of “controlled permissionlessness.” While the pharmaceutical regulatory landscape remains inherently “permissioned,” the active adaptation and evolution demonstrated by regulators—issuing guidance on master protocols, AI, and notably embracing decentralized and hybrid clinical trials—indicate a move towards greater flexibility, efficiency, and remote participation. These adaptations, while still within a regulatory framework, embody hallmarks of permissionless thinking. This suggests that regulators are not static gatekeepers but are evolving, albeit cautiously and incrementally, towards a model that incorporates elements of “permissionlessness” (e.g., remote data collection, AI-driven insights, streamlined trial designs) while maintaining core safety and efficacy oversight. This path to integrating permissionless R&D appears to be a gradual, evidence-based evolution, driven by technological advancements and demonstrated benefits within controlled environments, rather than a radical overhaul.
- Global Harmonization: Regulatory bodies worldwide are actively collaborating at scientific and technical levels to advance convergence for robust regulatory standards. This includes efforts to modernize global drug development, implement multi-regional clinical trial principles, and accelerate the adoption of Good Clinical Practices (GCPs).55
Discussion of “Precautionary Principle” vs. “Permissionless Innovation” in Policy
The fundamental policy debate often crystallizes around a core question: should innovation be permitted until proven harmful, or should proof of safety be required before anything new is allowed?.8 Historically, the U.S. has, at least traditionally, leaned towards the former, fostering a culture of experimentation, whereas Europe has often defaulted to the latter, embodying a more precautionary approach.8
Critics argue that an overly cautious approach, exemplified by the overregulation of nuclear power, can stifle progress and, paradoxically, cost lives by delaying beneficial innovations.8 The emphasis, they contend, should be on regulating only when there is “real harm, not hypothetical fear”.8 A critical observation in this debate is that regulatory pushes are sometimes influenced by incumbent firms seeking to protect themselves from competition. It has been noted that “Old players love regulation—they can afford it, and it locks out new entrants,” suggesting a risk of regulatory capture where safety concerns can be leveraged to create anti-competitive barriers.8 This highlights a “regulatory capture” risk inherent in the precautionary principle. While ostensibly designed for public safety, a highly permissioned system can inadvertently be co-opted by established players to create significant barriers to entry for smaller, more agile innovators who lack the extensive resources to navigate complex regulatory landscapes. This adds a crucial political economy dimension to the debate, suggesting that policy reforms must actively guard against such capture to truly foster innovation.
The following table provides a detailed overview of the key stages in drug development, outlining the current regulatory requirements and permissions mandated by the FDA and EMA. This illustrates the highly permissioned nature of the existing system.
Table 2: Key Stages of Drug Development with Current Regulatory Requirements (FDA/EMA)
| Stage of Development | FDA Requirements/Permissions | EMA Requirements/Permissions | Key Purpose/Focus |
| Discovery & Development | Initial lab research, target identification, compound synthesis 11 | Lab testing to understand drug mechanism 13 | Identify potential drug candidates and mechanisms of action |
| Preclinical Research | Animal testing for basic safety (toxicity, pharmacology) 11 | Lab and animal testing to understand drug behavior 13 | Assess basic safety, dosage, and biological activity before human trials |
| Clinical Research Phase 1 | IND Application submission (Form FDA 1571, 1572, etc.), IRB approval, 20-100 healthy volunteers/patients 12 | Small number of healthy volunteers/patients 13 | Human safety, dosage range, how drug interacts with body |
| Clinical Research Phase 2 | Up to several hundred patients, additional safety data, refine research questions 12 | Relatively small number of patients with targeted condition 13 | Efficacy in target population, further safety data, optimal dosing |
| Clinical Research Phase 3 | 300-3,000 participants, pivotal studies, long-term/rare side effects 12 | Larger number of patients, demonstrate treatment benefit 13 | Confirm efficacy, monitor adverse reactions, establish benefit-risk profile |
| FDA/EMA Drug Review/Assessment | NDA/BLA submission, data review by FDA teams, approval decision 11 | Single Marketing-Authorization Application (MAA), scientific assessment by CHMP/CVMP, European Commission decision 13 | Thorough examination of all data to determine safety, efficacy, quality, and purity for market authorization |
| Post-Market Monitoring | Ongoing safety monitoring (Phase 4) 11 | Continuous monitoring of suspected side effects, regular assessment of benefit-risk balance, post-authorization safety studies 13 | Real-world safety and efficacy, identification of rare/long-term adverse events, risk management |
6. Hybrid Models and the Future of Pharmaceutical R&D
The trajectory of pharmaceutical R&D is increasingly pointing towards the adoption of hybrid models that strategically integrate elements of permissionless innovation within existing, robust regulatory frameworks. This approach seeks to harness the benefits of decentralization and open collaboration while mitigating the inherent risks.
Exploring Integrated Approaches
The future of pharmaceutical R&D is likely to be characterized by hybrid models that purposefully incorporate decentralized clinical trial (DCT) elements into study designs.59 These models offer unparalleled flexibility and have experienced a rapid increase in prevalence, now exceeding traditional on-site trials in recent years.59 Hybrid trials are particularly effective for studies involving patient populations that are difficult to recruit or those facing significant impediments to frequent site visits.59
Blending Permissioned Oversight with Permissionless Elements
The integration of permissionless elements into the pharmaceutical R&D pipeline requires a strategic blending of established oversight mechanisms with new, more open approaches.
- “Part Open, Part Closed” Governance: Pharmaceutical companies can adopt a “part open, part closed” governance structure. This involves providing open access to preclinical and clinical data on specific compounds while simultaneously retaining patents and control over core monetization avenues.1 This model allows external researchers to explore new applications, such as “off-label” uses of existing drugs 1, thereby encouraging broader participation in the open aspects of the technology and allowing “a thousand flowers to bloom”.1 Companies can derive significant benefit from third-party innovation by establishing clear rules for external contributions without necessitating prior face-to-face interaction.1
- Open-Source Software and Data Science: The pharmaceutical industry is increasingly embracing open-source software and data science tools across the entire drug development lifecycle.60 Major pharmaceutical organizations, including Roche, GSK, Novartis, and Pfizer, are leveraging open tools to reduce vendor lock-in, accelerate innovation, and enhance data manipulation and analysis, particularly within clinical workflows.60 Initiatives such as Pharmaverse and R Validation Hub actively promote collaboration and the dissemination of reliable information throughout the industry.60 Crucially, open-source tools can and should be utilized in regulatory submissions, with leading pharmaceutical companies actively collaborating with regulatory agencies like the FDA to provide guidance and obtain feedback on their appropriate use.60
- Decentralized Science (DeSci) Principles: Decentralized Science (DeSci), which leverages Web3 technologies such as blockchain, Decentralized Autonomous Organizations (DAOs), and smart contracts, aims to address inefficiencies prevalent in traditional scientific research by offering decentralized funding models, promoting transparency, and fostering collaboration.5 While DeSci faces challenges related to scalability, high transaction costs, data security, and resistance from established centralized institutions, ongoing DeSci projects are actively developing solutions through technological innovation and novel governance models.42
The Role of Technology (AI, Blockchain) in Enabling Controlled Decentralization
Advanced technologies are pivotal in enabling controlled decentralization within pharmaceutical R&D.
- AI-Powered Tools: Artificial intelligence (AI) and machine learning (ML) offer transformative potential to address the persistent challenges of high costs, lengthy timelines, and low success rates in drug discovery.4 AI can significantly accelerate target identification, optimize lead compounds, and guide compound selection by assessing drug-likeness.4 Furthermore, AI-powered predictive quality assurance systems can detect deviations before they impact product quality, and machine learning algorithms can continuously optimize manufacturing processes.34
- Blockchain for Transparency and Trust: Blockchain technology can provide a trustless, transparent, and immutable mechanism for coordinating funding and tracking research progress, thereby addressing misaligned incentives and enhancing reproducibility.5 Decentralized identity systems (DIDs), built on blockchain, promise a model where individuals retain ownership of their digital identities and control when and how their information is shared, without reliance on centralized intermediaries.7
- Real-time Monitoring and Automation: Investing in standardized, integrated platforms that leverage real-time monitoring, automation, and AI is crucial for maintaining consistent quality oversight in decentralized manufacturing environments.34 Such platforms support robust controls and audit readiness across distributed networks.34 The FDA’s issuance of draft guidance on AI and Master Protocols 55, coupled with the increasing regulatory acceptance and support for Decentralized Clinical Trials (DCTs) and hybrid models 57, indicates that regulators are not entirely resistant to change. This suggests an implicit “regulatory sandbox” approach, where new technologies and methodologies are allowed to develop and demonstrate their value within controlled, monitored environments before widespread adoption. This pragmatic middle ground allows for iterative learning, adaptation of regulations based on real-world evidence, and the gradual building of trust in more flexible, decentralized models. Furthermore, the success and trustworthiness of hybrid and permissionless models critically depend on the development of robust, transparent, and secure data governance frameworks. While these models inherently rely on extensive data sharing and real-time monitoring 1, concerns about data security and privacy, especially for sensitive medical and genetic information, are significant.38 The imperative is to establish not just technical solutions (e.g., encryption, access controls, blockchain for immutability) but also clear policies on data ownership, consent for sharing, and ethical use. Without effective data governance, the potential benefits of openness will be severely undermined by risks of breaches, misuse, and a subsequent erosion of trust among patients, researchers, companies, and regulators. Finally, the role of “soft law” and industry-led standards in a shifting paradigm becomes increasingly pronounced. As noted, “soft law”—agency guidance and best practices—becomes essential in a rapidly evolving technological landscape.9 In a hybrid permissionless environment, where rigid, ex-ante regulations might stifle innovation, industry-led standards, collaborative initiatives (e.g., Pharmaverse, R Consortium 60), and guidance from regulatory bodies 55 become crucial. This suggests that the future regulatory paradigm might involve a shift from purely prescriptive rules to more flexible, adaptive frameworks that encourage self-regulation, industry-wide best practices, and continuous collaboration. Regulators may increasingly act as facilitators and overseers of these evolving standards, rather than solely as strict gatekeepers, fostering a shared responsibility model for ensuring safety and quality while promoting innovation.
The following table summarizes the potential risks associated with a permissionless R&D environment across key categories, highlighting their specific manifestations and potential consequences.
Table 3: Summary of Potential Risks in a Permissionless Environment (Patient Safety, Quality, Ethics, IP, Liability)
| Risk Category | Specific Risks | Potential Consequences |
| Patient Safety | Inadequate safety testing, unforeseen adverse effects, lack of efficacy, lower safety bar 3 | Patient harm, severe adverse reactions, ineffective treatments, public health crises 32 |
| Product Quality | Counterfeit/substandard drugs, poor manufacturing practices, insufficient testing, fragmented QC 34 | Compromised drug integrity, loss of public trust, increased healthcare costs, market instability 35 |
| Ethical Concerns | Data privacy breaches, exploitation of vulnerable populations, undue influence from financial incentives, lack of informed consent 30 | Erosion of patient trust, legal/reputational damage, unethical research practices, human rights violations 30 |
| Intellectual Property | Unclear inventorship for AI-discovered drugs, erosion of patent value, challenges in incentivizing R&D 18 | Reduced long-term innovation, decreased investment, complex legal disputes, IP theft 47 |
| Legal Liability | Ambiguous accountability for harm, “chilling effect” on legitimate research due to liability fears 50 | Costly legal disputes, reluctance of researchers/funders to participate, lack of recourse for harmed parties 50 |
7. Conclusion: A Strategic Path Forward
This report has demonstrated that while a fully “permissionless” R&D model in pharmaceuticals presents significant and unacceptable risks to patient safety, quality control, and ethical standards, the strategic integration of permissionless elements offers a compelling path to unleash innovation. The current “permissioned” system, while indispensable for safeguarding public health, is undeniably burdened by high costs, long timelines, and missed opportunities, leading to the phenomenon of “Eroom’s Law”.5
Summary of Key Takeaways
The analysis reveals several critical points for consideration:
- Permissionless principles, such as open participation, parallel experimentation, and leveraging external expertise, can dramatically accelerate drug discovery and reduce costs. This is achieved by tapping into unused data and compounds, as exemplified by cases like Viagra and Goldcorp.1
- Technologies like decentralized clinical trials (DCTs), artificial intelligence (AI), and open-source platforms are already enabling more “permissionless” approaches within the existing regulatory framework, demonstrating practical benefits in terms of efficiency and patient access.20
- Critical challenges persist, particularly in ensuring robust patient safety, maintaining rigorous quality control across distributed networks, upholding fundamental ethical principles (e.g., informed consent, data privacy), and navigating complex intellectual property and liability issues in a less centralized environment.3
- The evolution towards greater permissionlessness in pharmaceutical R&D will likely involve hybrid models and a shift in regulatory philosophy. This necessitates moving towards a model of “controlled permissionlessness,” where innovation is fostered through flexibility and openness, while robust safeguards are maintained through adaptive regulation, advanced data governance, and strong industry-regulator collaboration.
Actionable Recommendations for Stakeholders
To navigate this complex landscape and effectively unleash innovation while preserving public health, specific actions are recommended for key stakeholders:
- For Policymakers and Regulators (e.g., FDA, EMA):
- Continue to evolve regulatory frameworks to embrace and provide clear, risk-based guidance for emerging technologies (AI, DCTs) and open science initiatives. This requires moving beyond a purely precautionary approach to one that balances risk with the imperative for innovation.8
- Explore and pilot “regulatory sandboxes” to allow controlled experimentation with permissionless R&D models. This iterative approach enables the gathering of empirical evidence to inform future policy and build public trust in new methodologies.
- Actively combat “regulatory capture” by ensuring that policies genuinely serve the broader public health and innovation landscape, rather than inadvertently protecting incumbent interests and stifling new entrants.8
- Invest in digital infrastructure for secure, transparent data sharing and robust real-time post-market surveillance. This will enable effective monitoring and adaptation to new R&D models as they emerge and evolve.
- For Pharmaceutical Companies:
- Strategically adopt “part open, part closed” innovation models, sharing preclinical and clinical data and compounds to leverage external expertise and identify new opportunities, while diligently protecting core intellectual property.1
- Accelerate investment in decentralized clinical trial capabilities and open-source data science tools to drive operational efficiency, shorten timelines, and enhance data quality and analysis.20
- Prioritize the development and implementation of robust internal quality control and risk management systems that can operate effectively and consistently in decentralized manufacturing and research environments, leveraging AI for predictive quality assurance.34
- Actively engage with regulatory bodies, academic institutions, and patient advocacy groups to co-create standards, best practices, and ethical guidelines for emerging R&D models, fostering a collaborative ecosystem.60
- For Researchers and Innovators:
- Embrace open science principles, actively contributing to shared data repositories and collaborative platforms to accelerate collective knowledge discovery and enhance reproducibility.
- Champion ethical conduct and patient-centric approaches in all innovative R&D endeavors, ensuring stringent adherence to informed consent protocols and robust data privacy measures.38
- Actively participate in citizen science initiatives and crowdsourcing efforts to democratize research and address unmet medical needs, recognizing the value of diverse skills and contextual knowledge from broader communities.24
By strategically integrating permissionless elements within a carefully managed and adaptive regulatory framework, the pharmaceutical industry can unlock unprecedented innovation, address critical health challenges more efficiently, and ultimately deliver life-changing medicines to patients faster and more affordably, without compromising the fundamental principles of safety and ethical conduct.
Works cited
- Permissionless Innovation – Communications of the ACM, accessed July 17, 2025, https://cacm.acm.org/opinion/permissionless-innovation/
- Costs of Drug Development and Research and Development Intensity in the US, 2000-2018, accessed July 17, 2025, https://aspe.hhs.gov/reports/drug-development-rd-intensity
- Managing risks in drug discovery: reproducibility of published …, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4785199/
- AI-Driven Drug Discovery: A Comprehensive Review | ACS Omega, accessed July 17, 2025, https://pubs.acs.org/doi/10.1021/acsomega.5c00549
- From Challenges to Opportunities: How DeSci Reimagines Science, accessed July 17, 2025, https://public.bnbstatic.com/static/files/research/from-challenges-to-opportunities-how-desci-reimagines-science.pdf
- blockworks.co, accessed July 17, 2025, https://blockworks.co/glossary/permissionless#:~:text=By%20eliminating%20gatekeepers%2C%20these%20systems,to%20meet%20someone%20else’s%20conditions.
- Permissionless Definition & Meaning | Blockworks Editorial, accessed July 17, 2025, https://blockworks.co/glossary/permissionless
- Regulation and the Case for Permissionless Innovation – CPAC.org, accessed July 17, 2025, https://www.cpac.org/post/regulation-and-the-case-for-permissionless-innovation
- CAN WE MAKE MEDICINE MORE PERMISSIONLESS? – Idaho State University, accessed July 17, 2025, https://www.isu.edu/media/libraries/pharmacy/ce/slides/Thierer-Slides.pdf
- Precision Medicine Demands “Permissionless Innovation” – Orion Health, accessed July 17, 2025, https://orionhealth.com/us/blog/precision-medicine-demands-permissionless-innovation/
- The Drug Development Process | FDA, accessed July 17, 2025, https://www.fda.gov/patients/learn-about-drug-and-device-approvals/drug-development-process
- Step 3: Clinical Research – FDA, accessed July 17, 2025, https://www.fda.gov/patients/drug-development-process/step-3-clinical-research
- Authorisation of medicines | European Medicines Agency (EMA), accessed July 17, 2025, https://www.ema.europa.eu/en/about-us/what-we-do/authorisation-medicines
- Navigating EMA Approval: A Comprehensive Guide, accessed July 17, 2025, https://www.numberanalytics.com/blog/ema-approval-process-guide
- Investigational New Drug Applications (INDs) for CBER-Regulated …, accessed July 17, 2025, https://www.fda.gov/vaccines-blood-biologics/development-approval-process-cber/investigational-new-drug-applications-inds-cber-regulated-products
- What is an IND? – NIH Clinical Center, accessed July 17, 2025, https://www.cc.nih.gov/orcs/ind/what-is-an-ind
- BLA vs NDA: Regulatory Differences For Market Approval | Allucent, accessed July 17, 2025, https://www.allucent.com/resources/blog/what-are-regulatory-differences-between-nda-and-bla
- Rethinking Pharmaceutical Innovation Policy | Institute for New Economic Thinking, accessed July 17, 2025, https://www.ineteconomics.org/perspectives/blog/rethinking-pharmaceutical-innovation-policy
- Four Ways Pharmaceutical Companies Are De-Risking R&D with Real-World Data, accessed July 17, 2025, https://cotahealthcare.com/blog/mission/four-ways-pharmaceutical-companies-are-de-risking-rd-with-real-world-data/
- Decentralized clinical trials: challenges and opportunities in the future of clinical research, accessed July 17, 2025, https://www.ideagen.com/thought-leadership/blog/decentralized-clinical-trials-challenges
- Decentralized clinical trials can have big financial upside, study finds, accessed July 17, 2025, https://www.drugdiscoverytrends.com/decentralized-clinical-trials-can-have-big-financial-upside-study-finds/
- Impact of Model-Informed Drug Development on Drug Development Cycle Times and Clinical Trial Cost – PubMed, accessed July 17, 2025, https://pubmed.ncbi.nlm.nih.gov/40135941/
- Innovation and Access to Medicines for Neglected Populations: Could a Treaty Address a Broken Pharmaceutical R&D System? – PMC – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3352855/
- Open Source Drug Discovery – Wikipedia, accessed July 17, 2025, https://en.wikipedia.org/wiki/Open_Source_Drug_Discovery
- Companies are engaging in adaptive R&D, tailoring products to the needs of people in LMICs – Access to Medicine Foundation, accessed July 17, 2025, https://accesstomedicinefoundation.org/resource/companies-are-engaging-in-adaptive-r-and-d-tailoring-products-to-the-needs-of-people-in-lmics
- Open Source Drug Discovery – redefining IPR through open source innovations, accessed July 17, 2025, https://www.researchgate.net/publication/289803325_Open_Source_Drug_Discovery_-_redefining_IPR_through_open_source_innovations
- Be a Citizen Scientist | NIH News in Health, accessed July 17, 2025, https://newsinhealth.nih.gov/2023/11/be-citizen-scientist
- Citizen science to further precision medicine: from vision to implementation | JAMIA Open | Oxford Academic, accessed July 17, 2025, https://academic.oup.com/jamiaopen/article/3/1/2/5651081
- Institutional Review Boards Frequently Asked Questions – FDA, accessed July 17, 2025, https://www.fda.gov/regulatory-information/search-fda-guidance-documents/institutional-review-boards-frequently-asked-questions
- Clinical Research: Benefits, Risks, and Safety | National Institute on Aging, accessed July 17, 2025, https://www.nia.nih.gov/health/clinical-trials-and-studies/clinical-research-benefits-risks-and-safety
- Unanticipated Problems Involving Risks & Adverse Events Guidance (2007) – HHS.gov, accessed July 17, 2025, https://www.hhs.gov/ohrp/regulations-and-policy/guidance/reviewing-unanticipated-problems/index.html
- Medication Without Harm – World Health Organization (WHO), accessed July 17, 2025, https://www.who.int/initiatives/medication-without-harm
- Protecting patient safety – Roche, accessed July 17, 2025, https://www.roche.com/about/sustainability/patient-safety
- Regulating the Shift: Quality and Compliance in Decentralized Drug Production, accessed July 17, 2025, https://www.americanpharmaceuticalreview.com/Featured-Articles/618962-Regulating-the-Shift-Quality-and-Compliance-in-Decentralized-Drug-Production/
- Challenges Leading to Poor Pharmaceutical Quality Control …, accessed July 17, 2025, https://pharmatimesofficial.com/project/challenges-leading-to-poor-pharmaceutical-quality-control/
- Quality assurance in pharmaceutical manufacturing: bridging the gap between regulations, supply chain, and innovations – ResearchGate, accessed July 17, 2025, https://www.researchgate.net/publication/389313408_Quality_assurance_in_pharmaceutical_manufacturing_bridging_the_gap_between_regulations_supply_chain_and_innovations
- The most recurring problems in Quality Control – Alispharm, accessed July 17, 2025, https://www.alispharm.com/articles/the-most-recurring-problems-in-qc/
- The Significance of Ethical Considerations in Drug Discovery Research – Lindus Health, accessed July 17, 2025, https://www.lindushealth.com/blog/the-significance-of-ethical-considerations-in-drug-discovery-research
- Human subject research legislation in the United States – Wikipedia, accessed July 17, 2025, https://en.wikipedia.org/wiki/Human_subject_research_legislation_in_the_United_States
- Research Ethics and Informed Consent | Educational Research Basics by Del Siegle, accessed July 17, 2025, https://researchbasics.education.uconn.edu/ethics-and-informed-consent/
- Ethical considerations for clinical trials on medicinal products conducted with minors – Public Health, accessed July 17, 2025, https://health.ec.europa.eu/system/files/2018-02/2017_09_18_ethical_consid_ct_with_minors_0.pdf
- How Decentralized Science (DeSci) Improves Research – Ulam Labs, accessed July 17, 2025, https://www.ulam.io/blog/how-decentralized-science-is-revolutionizing-research
- New psychoactive substances – Alcohol and Drug Foundation, accessed July 17, 2025, https://adf.org.au/drug-facts/new-psychoactive-substances/
- How will deregulation in the US affect the international medical …, accessed July 17, 2025, https://medtechintelligence.com/feature_article/how-will-deregulation-in-the-us-affect-the-international-medical-device-market/
- The Impact of Social Factors on Drug Development – Altasciences, accessed July 17, 2025, https://www.altasciences.com/resource-center/blog/impact-social-factors-drug-development
- Ensuring ethical standards and procedures for research with human beings, accessed July 17, 2025, https://www.who.int/activities/ensuring-ethical-standards-and-procedures-for-research-with-human-beings
- Drug patents: innovation v. accessibility – PMC, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC3680575/
- The Inflation Reduction Act Is Negotiating the United States Out of Drug Innovation | ITIF, accessed July 17, 2025, https://itif.org/publications/2025/02/25/the-inflation-reduction-act-is-negotiating-the-united-states-out-of-drug-innovation/
- Emerging Legal Terrain: IP Risks from AI’s Role in Drug Discovery – Fenwick, accessed July 17, 2025, https://www.fenwick.com/insights/publications/emerging-legal-terrain-ip-risks-from-ais-role-in-drug-discovery
- [2408.04717] Redefining Accountability: Navigating Legal Challenges of Participant Liability in Decentralized Autonomous Organizations – arXiv, accessed July 17, 2025, https://arxiv.org/abs/2408.04717
- No Liability For Contributing Funding For Research Activities | Drug & Device Law, accessed July 17, 2025, https://www.druganddevicelawblog.com/2025/01/no-liability-for-contributing-funding-for-research-activities.html
- Permissionless Innovation: A 10-Point Checklist for Public Policymakers | Mercatus Center, accessed July 17, 2025, https://www.mercatus.org/research/policy-briefs/permissionless-innovation-10-point-checklist-public-policymakers
- Rolling NDA and BLA Submissions: Accelerate Your Review Timeline – Certara, accessed July 17, 2025, https://www.certara.com/blog/rolling-nda-and-bla-submissions-accelerate-your-timeline-for-review/
- Forward Through Uncertainty: What Biopharma Leaders Are Saying About the FDA, R&D Investment – THL, accessed July 17, 2025, https://thl.com/articles/forward-through-uncertainty-what-biopharma-leaders-are-saying-about-the-fda-rd-investment/
- Five Regulatory Trends to Harness in 2025 | Contract Pharma, accessed July 17, 2025, https://www.contractpharma.com/exclusives/five-regulatory-trends-to-harness-in-2025/
- Undeterred by Political, Economic Headwinds, Pharma Ups R&D Investment in 2024 and Beyond – BioSpace, accessed July 17, 2025, https://www.biospace.com/business/undeterred-by-political-economic-headwinds-pharma-ups-r-d-investment-in-2024-and-beyond
- FDA’s final guidance on DCTs adds clarity on HCP task log, inspection requirements, data variability | RAPS, accessed July 17, 2025, https://www.raps.org/news-and-articles/news-articles/2024/9/fda-s-final-guidance-on-dcts-adds-clarity-on-hcp-t
- Summary of EMA’s Recommendation Paper on Decentralized Clinical Trial Elements, accessed July 17, 2025, https://www.appliedclinicaltrialsonline.com/view/summary-of-ema-s-recommendation-paper-on-decentralized-clinical-trial-elements
- Hybrid Clinical Trials: The Shift to Decentralization – ObvioHealth, accessed July 17, 2025, https://www.obviohealth.com/resources/hybrid-clinical-trials-the-shift-to-decentralization
- Open-Source Adoption in Pharma: Opportunities and Challenges – Appsilon, accessed July 17, 2025, https://www.appsilon.com/post/open-source-pharma
- Software Development in the Pharmaceutical Sector: Full Guide – JetBase, accessed July 17, 2025, https://jetbase.io/blog/software-development-in-the-pharmaceutical-sector-full-guide
- Open-Source Data Science for Pharmaceutical Companies – Posit, accessed July 17, 2025, https://posit.co/use-cases/pharma/
- Decentralized science (DeSci): definition, shared values, and guiding principles – Frontiers, accessed July 17, 2025, https://www.frontiersin.org/journals/blockchain/articles/10.3389/fbloc.2024.1375763/full
- An ethical exploration of barriers to research on controlled drugs – PMC – PubMed Central, accessed July 17, 2025, https://pmc.ncbi.nlm.nih.gov/articles/PMC4849133/
- Do Private Equity and Other Investors Harm Competition in the Pharmaceutical Industry?, accessed July 17, 2025, https://www.promarket.org/2025/05/15/do-private-equity-and-other-investors-harm-competition-in-the-pharmaceutical-industry/