The path to market for generic drugs is paved with scientific rigor and exacting standards. For business professionals in this competitive landscape, understanding the nuances of generic drug development is not just an advantage—it’s a necessity. At the heart of this process lies a critical discipline: reverse engineering. But not just any reverse engineering will do. The golden keys to unlocking market success are precision and reproducibility. This in-depth guide will explore why these two pillars are paramount, how they are achieved, and how they can transform data into a powerful tool for market domination. We’ll delve into the intricate dance of analytical chemistry, regulatory hurdles, and strategic planning that defines the journey of a generic drug from the lab bench to the pharmacy shelf.
The Imperative of Sameness: Why Generic Drugs Must Mirror their Innovator Counterparts
Have you ever wondered what makes a generic drug a trustworthy alternative to its brand-name predecessor? The answer lies in a concept known as pharmaceutical equivalence. For a generic drug to be approved for public use, it must be, in essence, a mirror image of the original innovator product. This means it must contain the same active pharmaceutical ingredient (API), in the same dosage form and strength, and be administered via the same route. But the similarities don’t stop there. The generic must also demonstrate bioequivalence, meaning it is absorbed into the bloodstream and performs its therapeutic action in the same way and to the same extent as the brand-name drug.
This requirement for “sameness” is not arbitrary. It is the bedrock of patient safety and drug efficacy. When a patient switches from a brand-name drug to a generic, they expect and deserve the same clinical outcome. Any significant deviation could lead to treatment failure or adverse effects. This is where the meticulous process of reverse engineering comes into play, guided by the unwavering principles of precision and reproducibility.
Deconstructing the Innovator: The Art and Science of Reverse Engineering
Reverse engineering a drug is akin to being a master watchmaker meticulously disassembling a complex timepiece to understand its inner workings. The goal is not just to identify the main components but to understand how they are put together, the quality of each part, and the intricate interplay between them. In pharmaceutical terms, this process, often referred to as deformulation, involves a deep dive into the innovator drug’s composition.
Identifying the Core: The Active Pharmaceutical Ingredient (API)
The first and most crucial step is the unequivocal identification of the Active Pharmaceutical Ingredient (API). This is the molecule responsible for the drug’s therapeutic effect. Scientists employ a battery of sophisticated analytical techniques to confirm its chemical structure, purity, and physical properties. Think of the API as the engine of the car—its performance is non-negotiable.
Beyond the Active: Unraveling the Excipient Matrix
But a drug is more than just its API. It also contains a variety of excipients, which are inactive substances that serve a multitude of purposes. They can act as fillers, binders, disintegrants, lubricants, and coatings, among other roles. These excipients are not mere window dressing; they are critical to the drug’s stability, bioavailability, and overall performance. The reverse engineering process must, therefore, painstakingly identify and quantify each excipient to understand the complete formulation “recipe.” This is where the true complexity of deformulation lies. The excipient matrix can be a complex puzzle, with each piece needing to be precisely placed.
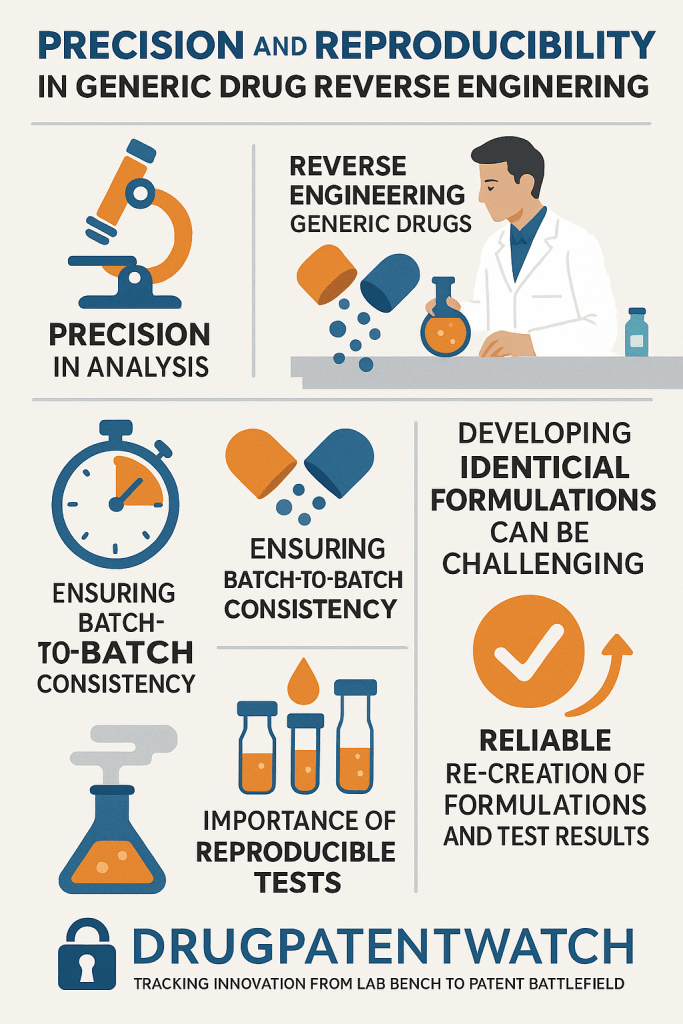
Precision: The Bedrock of Analytical Excellence
In the context of generic drug reverse engineering, precision refers to the closeness of agreement between independent test results obtained under stipulated conditions. It’s about getting the same result over and over again when analyzing the same sample. High precision is the hallmark of a reliable analytical method.
Why Precision is Non-Negotiable
Imagine trying to replicate a complex recipe where the measurements are inconsistent. A pinch of salt one time, a handful the next. The final dish would be unpredictable, and likely, unpalatable. The same principle applies to drug formulation. Even small variations in the amount of a key excipient can significantly impact the drug’s dissolution profile, stability, and ultimately, its therapeutic effect.
For business professionals, a lack of precision in the deformulation process can have dire consequences, leading to:
- Failed batches: Inconsistent analytical results can lead to the production of batches that do not meet quality standards, resulting in significant financial losses.
- Regulatory delays: Regulatory agencies like the U.S. Food and Drug Administration (FDA) demand robust data demonstrating the precision of the analytical methods used. Insufficient precision can lead to questions, requests for more data, and ultimately, a longer and more costly approval process.
- Inconsistent product performance: If the analytical methods used to develop the generic are not precise, the final product may exhibit batch-to-batch variability, potentially impacting patient outcomes and eroding trust in the brand.
Achieving Analytical Precision: A Multi-faceted Approach
Achieving high precision is not a matter of chance; it is the result of a deliberate and systematic approach. This includes:
- Method Validation: All analytical methods used in the reverse engineering process must be rigorously validated to ensure they are fit for purpose. This involves demonstrating their accuracy, precision, specificity, linearity, and range.
- Instrument Calibration: The sophisticated analytical instruments used in deformulation, such as High-Performance Liquid Chromatography (HPLC) and Mass Spectrometry (MS), must be meticulously calibrated and maintained to ensure they are performing optimally.
- Analyst Training: The scientists performing the analyses must be highly trained and proficient in the specific techniques and instrumentation being used.
Reproducibility: The Ultimate Test of a Robust Formulation
While precision is about the consistency of results within a single laboratory, reproducibility takes it a step further. It refers to the ability to obtain the same results when the analysis is performed in different laboratories, by different analysts, and with different equipment. Reproducibility is the ultimate test of the robustness of both the analytical methods and the reverse-engineered formulation itself.
The Significance of Reproducibility in a Globalized World
In today’s globalized pharmaceutical industry, drug development and manufacturing are often spread across multiple sites and even multiple countries. A generic drug company may have an R&D facility in one country, a manufacturing plant in another, and a quality control lab in a third. For this complex supply chain to function seamlessly, the ability to reproduce results is paramount.
For business leaders, reproducibility is a critical strategic advantage. It enables:
- Scalable Manufacturing: A reproducible formulation and analytical method can be confidently transferred from the small-scale R&D lab to a large-scale commercial manufacturing facility without unexpected issues.
- Supply Chain Resilience: If one manufacturing site experiences a problem, production can be shifted to another site with the assurance that the final product will remain consistent.
- Global Market Access: A reproducible process facilitates the submission of a consistent and robust data package to regulatory authorities in different countries, streamlining the global approval process.
“The ability to consistently reproduce the physicochemical characteristics of the reference listed drug is a cornerstone of generic drug development. It is this reproducibility that provides the foundational evidence for bioequivalence.”
— Adapted from FDA Guidance for Industry, “Quality by Design for ANDAs: An Example for Modified-Release Dosage Forms.”
Strategies for Ensuring Reproducibility
Ensuring reproducibility requires a holistic approach that goes beyond just the analytical methods. It encompasses the entire development process, from raw material sourcing to final product packaging. Key strategies include:
- Quality by Design (QbD): This is a systematic approach to development that begins with predefined objectives and emphasizes product and process understanding and process control, based on sound science and quality risk management. By understanding how raw material attributes and process parameters affect the final product, companies can build reproducibility into the product from the very beginning.
- Robust Method Transfer Protocols: When an analytical method is transferred from one lab to another, a formal method transfer protocol should be followed. This ensures that the receiving lab can perform the method with the same level of precision and accuracy as the originating lab.
- Comprehensive Documentation: Every step of the reverse engineering and formulation development process should be meticulously documented. This includes detailed information about raw materials, processing parameters, and analytical results. This documentation is essential for troubleshooting issues and ensuring that the process can be reliably reproduced.
The Analytical Toolbox: Techniques for Deformulation
A wide array of sophisticated analytical techniques are employed in the reverse engineering of a generic drug. The choice of techniques depends on the complexity of the dosage form and the nature of the API and excipients.
Chromatographic Techniques: Separating the Components
Chromatography is a powerful set of techniques for separating the components of a mixture.
- High-Performance Liquid Chromatography (HPLC): HPLC is the workhorse of the pharmaceutical analysis lab. It is used to separate, identify, and quantify the API and various excipients. When coupled with a variety of detectors, such as UV-Vis, fluorescence, or mass spectrometry, it provides a wealth of information about the drug’s composition.
- Gas Chromatography (GC): GC is used for the analysis of volatile and semi-volatile compounds, such as residual solvents that may be present from the manufacturing process.
Spectroscopic Techniques: Unveiling the Molecular Structure
Spectroscopy involves the interaction of electromagnetic radiation with matter, providing information about molecular structure and composition.
- Mass Spectrometry (MS): MS is a highly sensitive technique that measures the mass-to-charge ratio of ions. It is invaluable for confirming the identity of the API and for identifying unknown impurities.
- Nuclear Magnetic Resonance (NMR) Spectroscopy: NMR provides detailed information about the molecular structure of the API and can also be used to characterize certain excipients.
- Fourier-Transform Infrared (FTIR) Spectroscopy: FTIR is a rapid and non-destructive technique that can be used to identify functional groups in molecules and to characterize the solid-state properties of the drug.
Solid-State Characterization: Understanding the Physical Form
The physical form of the API and excipients can have a profound impact on the drug’s performance.
- X-ray Powder Diffraction (XRPD): XRPD is used to identify the crystalline form, or polymorph, of the API. Different polymorphs can have different solubilities and dissolution rates, which can affect bioavailability.
- Differential Scanning Calorimetry (DSC): DSC measures the heat flow associated with thermal transitions in a material, such as melting and crystallization. It provides information about the purity and physical state of the drug.
- Particle Size Analysis: The particle size of the API and excipients can influence dissolution rates and bioavailability. Various techniques, such as laser diffraction, are used to measure particle size distribution.
Navigating the Regulatory Maze: The FDA and International Standards
The path to generic drug approval is heavily regulated. Regulatory agencies like the FDA have established stringent guidelines to ensure the safety and efficacy of generic drugs.
The Role of the FDA’s Office of Generic Drugs (OGD)
In the United States, the FDA’s Office of Generic Drugs (OGD) is responsible for reviewing and approving Abbreviated New Drug Applications (ANDAs). A key component of the ANDA is the Chemistry, Manufacturing, and Controls (CMC) section, which provides a comprehensive overview of the drug’s composition, manufacturing process, and the analytical methods used to ensure its quality.
The OGD places a strong emphasis on the demonstration of precision and reproducibility in the CMC data. They want to see that the generic company has a deep understanding of its product and process and has implemented robust controls to ensure consistency.
International Harmonization: The ICH
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) is a global body that brings together regulatory authorities and pharmaceutical industry representatives to discuss scientific and technical aspects of drug registration. The ICH has developed a series of guidelines that have been adopted by many countries around the world. These guidelines provide a framework for ensuring the quality, safety, and efficacy of drugs, including generics.
Adherence to ICH guidelines can facilitate the global registration of a generic drug by ensuring that the data package meets the requirements of multiple regulatory agencies.
From Data to Domination: Leveraging Precision and Reproducibility for Market Success
For business professionals in the generic drug industry, a deep appreciation for the importance of precision and reproducibility can be a powerful driver of market success. By investing in the scientific expertise and technological infrastructure necessary to achieve these principles, companies can:
- Accelerate Time to Market: A robust and well-documented development process, characterized by high precision and reproducibility, can lead to a smoother and faster regulatory review. This means getting the product to market sooner and capturing a larger market share. As an industry expert, Dr. P. K. Rajput, once remarked, “In the generic race, speed to market is everything. A well-executed deformulation and development program is the starting gun.”
- Reduce Development Costs: While investing in high-quality analytics may seem expensive upfront, it can actually save money in the long run. By getting it right the first time, companies can avoid costly delays, failed batches, and the need for extensive rework.
- Build a Reputation for Quality: A company that consistently produces high-quality generic drugs will build a strong reputation with healthcare professionals, patients, and regulatory agencies. This can lead to increased market share and long-term profitability. According to a 2023 report by the Association for Accessible Medicines, the use of FDA-approved generics has saved the U.S. healthcare system over $2.9 trillion in the last decade, a testament to the trust placed in these products.
- Gain a Competitive Edge: In a crowded and competitive market, a company that can demonstrate a superior understanding of its product and process will have a significant competitive advantage. This can be a key differentiator when it comes to securing contracts with large purchasers, such as hospital systems and pharmacy benefit managers.
The Future of Generic Drug Reverse Engineering: Emerging Trends and Technologies
The field of generic drug reverse engineering is constantly evolving, driven by advances in analytical technology and a deeper understanding of the science of formulation. Some of the emerging trends that are shaping the future of the industry include:
- Advanced Analytics: The development of more sensitive and powerful analytical techniques, such as advanced mass spectrometry and solid-state NMR, is enabling a more detailed and comprehensive characterization of innovator drugs.
- In Silico Modeling and Simulation: Computer modeling and simulation are increasingly being used to predict how different formulations will behave in the body. This can help to streamline the development process and reduce the need for extensive clinical testing.
- Continuous Manufacturing: This is a modern approach to manufacturing where the production process is run continuously, rather than in discrete batches. Continuous manufacturing can lead to improved product quality and consistency.
By embracing these new technologies and approaches, generic drug companies can further enhance their ability to develop high-quality, reproducible products that can compete effectively in the global market.
Key Takeaways
- Sameness is Paramount: Generic drugs must be pharmaceutically equivalent and bioequivalent to their brand-name counterparts to ensure patient safety and therapeutic efficacy.
- Reverse Engineering is a Meticulous Process: Deformulation involves the precise identification and quantification of both the active pharmaceutical ingredient (API) and the excipient matrix.
- Precision and Reproducibility are Non-Negotiable: These principles are the cornerstones of reliable analytical data and robust product development, leading to faster approvals and consistent product performance.
- A Sophisticated Analytical Toolbox is Essential: A combination of chromatographic, spectroscopic, and solid-state characterization techniques is necessary for a comprehensive understanding of the innovator drug.
- Regulatory Compliance is Key: Adherence to FDA and international guidelines, such as those from the ICH, is crucial for successful market entry.
- Strategic Investment in Quality Drives Market Domination: By prioritizing precision and reproducibility, companies can accelerate time to market, reduce costs, build a strong reputation, and gain a significant competitive advantage.
Frequently Asked Questions (FAQs)
1. What is the difference between reverse engineering and deformulation in the context of generic drugs?
While often used interchangeably, there’s a subtle distinction. Reverse engineering is the broader concept of taking a product apart to understand how it works. Deformulation is a specific type of reverse engineering focused on determining the qualitative and quantitative composition of a chemical formulation, which is central to generic drug development.
2. How does the FDA’s Quality by Design (QbD) initiative relate to precision and reproducibility?
QbD is a proactive approach that builds quality into a product from the outset. By understanding the relationships between raw material attributes, manufacturing process parameters, and critical quality attributes of the final product, QbD inherently fosters precision and reproducibility. It moves beyond simply testing for quality at the end to designing a process that consistently delivers a high-quality product.
3. Can a generic drug have different excipients than the brand-name drug and still be approved?
Yes, this is possible. The key is that the generic drug must be bioequivalent to the brand-name drug. If a different excipient is used, the generic company must provide data to the FDA demonstrating that this change does not affect the safety or efficacy of the drug. The performance of the product is what ultimately matters.
4. What are the biggest challenges in the reverse engineering of complex dosage forms, such as extended-release tablets or transdermal patches?
Complex dosage forms present significant challenges due to their intricate structures and release mechanisms. For an extended-release tablet, it’s not just about what’s in it, but how the drug is released over time. For a transdermal patch, the adhesive properties and the rate of drug delivery through the skin are critical. Reverse engineering these products requires a deeper level of analytical investigation and a more sophisticated understanding of materials science and biopharmaceutics.
5. How can a smaller generic drug company with limited resources compete with larger companies in terms of analytical capabilities?
Smaller companies can strategically partner with specialized contract research organizations (CROs) that have the state-of-the-art instrumentation and scientific expertise required for complex deformulation studies. This allows them to access top-tier analytical capabilities without the significant capital investment in building and maintaining their own advanced laboratories. A focus on a niche portfolio of products can also allow for a more concentrated and effective use of resources.
Cited Sources
- U.S. Food and Drug Administration. (2011). Guidance for Industry: Quality by Design for ANDAs: An Example for Modified-Release Dosage Forms.
- Association for Accessible Medicines. (2023). 2023 Generic Drug & Biosimilars Access & Savings in the U.S. Report.
- Rajput, P. K. (2015). Generic Drug Product Development: Solid Oral Dosage Forms. CRC Press.