Introduction: The Biosimilar Revolution and the High-Stakes Game of Clinical Development
Welcome to the new frontier of pharmaceutical development. For decades, the industry’s narrative was dominated by the quest for novel, first-in-class molecules—a high-risk, high-reward saga of discovery. Today, a powerful new chapter is being written, one driven not by invention, but by meticulous replication and strategic science: the era of the biosimilar. This isn’t just a trend; it’s a seismic shift, promising to enhance patient access, drive down healthcare costs, and inject a ferocious new brand of competition into the biologics market, which is projected to exceed $600 billion by 2026 [1].
But make no mistake. Stepping into the biosimilar arena is like navigating a complex, high-stakes labyrinth. The path to success is not a straight line but a winding journey fraught with scientific, regulatory, and commercial challenges. The prize—a share of the blockbuster revenue once held exclusively by innovator biologics—is immense. The cost of a misstep, however, can be catastrophic, leading to regulatory rejection, wasted investment, and a closed window of market opportunity. At the very heart of this labyrinth lies the most critical challenge of all: the design and execution of clinical trials. How do you prove your product is, for all intents and purposes, the same as a reference product that itself has inherent variability? How do you satisfy regulators, convince physicians, and win over payers in a landscape built on trust and data?
This is where the game is won or lost. Unlike novel drug development, the goal isn’t to prove efficacy and safety from scratch. The goal is to demonstrate “biosimilarity”—a concept that is deceptively simple in theory but profoundly complex in practice. It requires a paradigm shift in thinking, moving away from the traditional, sprawling Phase I-II-III sequence towards a targeted, evidence-based approach where every piece of data, from the earliest analytical characterization to the final confirmatory study, forms a single, cohesive argument.
What is a Biosimilar? A Refresher on the Fundamentals
Before we dive into the strategic depths of trial design, let’s ensure our foundational understanding is solid. A biosimilar is a biological product that is highly similar to, and has no clinically meaningful differences from, an existing FDA-approved reference product [2]. Biologics, or biological products, are large, complex molecules—often proteins—derived from living organisms like bacteria or mammalian cells. Think of monoclonal antibodies like adalimumab (Humira) or infliximab (Remicade); these are the titans of the biologic world.
The complexity of these molecules is the very reason we have biosimilars and not “bio-generics.”
Differentiating Biosimilars from Generics and Novel Biologics
Imagine the difference between building a bicycle and replicating a high-performance jet engine. A generic drug is like the bicycle. It’s a small, chemically synthesized molecule (e.g., atorvastatin, the generic for Lipitor) with a simple, well-defined structure. You can precisely replicate the chemical formula, and you know you have the exact same active ingredient. The clinical trial path for generics is therefore straightforward, typically requiring only a simple bioequivalence study in a handful of healthy volunteers to show that the drug gets into the bloodstream at the same rate and concentration.
A biosimilar, on the other hand, is the jet engine. It’s a massive, intricate protein with a specific three-dimensional structure, complex post-translational modifications like glycosylation (the attachment of sugar chains), and it’s produced in living cells. This manufacturing process, no matter how controlled, has inherent variability. You can’t create an identical copy; the goal is to create a highly similar one. This distinction is everything. It means you can’t rely on a simple blood test alone. You need a “totality of the evidence” approach to convince regulators that the minor structural differences that inevitably exist have no impact on how the drug works or how safe it is for patients. This is the fundamental challenge that drives the entire clinical development strategy.
The Shifting Paradigm: From ‘De Novo’ Discovery to Demonstrating ‘Sameness’
Developing a novel biologic is a journey into the unknown. You have a new molecule, a new target, and you must painstakingly prove its safety and efficacy over many years and through multiple large, expensive clinical trials. The focus is on establishing the product’s own clinical benefit-risk profile.
Biosimilar development flips this script entirely. The reference product’s safety and efficacy are already established and accepted. Your mission, should you choose to accept it, is not to rediscover this clinical value but to demonstrate that your product is so similar to the reference product that you can rely on the innovator’s legacy of data. The goal is not discovery, but confirmation.
This requires a different mindset. You are part scientist, part detective. You must first deeply understand the reference product—its structure, its function, its clinical behavior—and then build a scientific bridge of evidence, piece by piece, that links your product to it. The heavy lifting is front-loaded in the analytical and pharmacokinetic stages, with the goal of reducing the size, scope, and uncertainty of the final, and most expensive, confirmatory clinical trials.
The Strategic Imperative: Why Effective Trial Design is the Cornerstone of Biosimilar Success
In this context, clinical trial design is not just a scientific exercise; it’s a critical business strategy. An efficient design can save tens of millions of dollars and shave years off the development timeline. A poorly conceived study, however, can lead to ambiguous results, regulatory delays, and a fatal erosion of your competitive advantage.
Consider this: you are racing against other biosimilar developers to launch as soon as the reference product’s patents expire. Every month of delay is a month of lost market share, potentially worth hundreds of millions of dollars. Your trial design must therefore be a masterclass in precision and efficiency. It must be sensitive enough to detect any potential differences between your product and the reference, yet robust enough to provide unequivocal evidence of similarity. It must satisfy the stringent demands of global regulators while also generating the data needed to convince skeptical physicians and cost-conscious payers to adopt your product.
This article is your guide through that labyrinth. We will dissect the strategies for effective biosimilar clinical trial design and execution, from navigating the global regulatory tapestry to mastering the intricacies of pharmacokinetic studies, from taming the specter of immunogenicity to leveraging digital tools for a competitive edge. Let’s begin building the bridge from scientific rigor to commercial triumph.
The Regulatory Tapestry: A Global Perspective on Biosimilar Approval Pathways
Before a single patient is enrolled, the entire biosimilar development program is shaped by the regulatory framework. Unlike the largely harmonized path for new drugs, the guidelines for biosimilars can differ significantly between regions. Understanding these nuances is not just a matter of compliance; it’s fundamental to designing a global development program that is both scientifically sound and commercially viable. A strategy optimized for the U.S. Food and Drug Administration (FDA) might not be sufficient for the European Medicines Agency (EMA), or vice versa. Let’s unravel this complex regulatory tapestry.
The Foundation: The U.S. Biologics Price Competition and Innovation Act (BPCIA)
In the United States, the legal pathway for biosimilars was established by the Biologics Price Competition and Innovation Act (BPCIA) of 2009, passed as part of the Affordable Care Act [2]. This landmark legislation created an abbreviated licensure pathway for biological products shown to be “biosimilar to” or “interchangeable with” an FDA-licensed reference product. This was the moment the starting gun was fired for the U.S. biosimilar market.
The “Totality of the Evidence” Approach Explained
The BPCIA framework is built upon a central philosophy: the “totality of the evidence.” This means that the FDA doesn’t look at any single piece of data in isolation. Instead, they evaluate the entire package of information you submit—a comprehensive story that begins with deep analytical characterization and builds through animal studies, human pharmacokinetic (PK) and pharmacodynamic (PD) data, and clinical immunogenicity and efficacy/safety data.
Think of it as a pyramid. The base of the pyramid is the most extensive and foundational layer: analytical studies. This is where you demonstrate that your molecule’s structure and function are highly similar to the reference product’s. As you move up the pyramid, the required studies become progressively more targeted and are designed to resolve any residual uncertainty that remains from the lower levels. If your analytical data is incredibly robust and shows an extremely high degree of similarity, the burden on the upper levels—the expensive clinical trials—may be reduced. Conversely, if there are lingering questions from the analytical comparison, you’ll need to address them with more extensive clinical data. This stepwise, risk-based approach is the essence of the BPCIA pathway.
Understanding the Stepwise Approach to Development
The FDA’s stepwise approach can be visualized as a series of gates. You must pass through each gate before proceeding to the next.
- Analytical Characterization: This is the non-negotiable foundation. Using a battery of state-of-the-art techniques, you create a detailed “fingerprint” of both your biosimilar candidate and the reference product. You compare primary structure (amino acid sequence), higher-order structures (folding, aggregation), and critical post-translational modifications. You also conduct functional assays to compare biological activity. The goal is to establish a high degree of similarity and identify any minor differences.
- Non-clinical Studies: This typically involves in vivo animal studies. However, the FDA has shown increasing flexibility here. If the analytical and functional data are compelling enough, extensive animal toxicology studies may not be necessary. The focus is often on comparative animal PK/PD studies to provide an initial in vivo bridge.
- Human Pharmacokinetic (PK) and Pharmacodynamic (PD) Studies: This is the first step into the clinic. A comparative PK study, usually in healthy volunteers, is almost always required. It aims to show that your biosimilar is absorbed, distributed, metabolized, and excreted in the same way as the reference product. A comparative PD study, which measures the drug’s effect on the body using biomarkers, is also expected if a relevant biomarker exists.
- Comparative Clinical Study (The Confirmatory Trial): If any residual uncertainty about biosimilarity remains after the preceding steps, the FDA will require at least one clinical study to confirm that there are no clinically meaningful differences in efficacy and safety. This is typically an equivalence trial in a sensitive patient population.
- Immunogenicity Assessment: Because all biologics have the potential to trigger an immune response, a comparative assessment of immunogenicity is a critical and mandatory component of the clinical program.
This stepwise process allows for a tailored, science-driven development program. As Dr. Sarah Yim, former Director of the Office of Therapeutic Biologics and Biosimilars at the FDA, has emphasized, “The goal of a biosimilar development program is to demonstrate biosimilarity, not to independently establish the safety and effectiveness of the proposed product. The stepwise approach allows developers to leverage what is already known about the reference product, potentially streamlining development” [3].
The European Medicines Agency (EMA): Pioneering the Biosimilar Framework
While the U.S. was establishing its pathway, the European Union was already well ahead. The EMA created the first comprehensive legal and regulatory framework for biosimilars back in 2005, giving them a significant head start in experience and approvals [4]. Their approach, while sharing the same core scientific principles as the FDA’s, has some important distinctions.
Key Differences between FDA and EMA Guidelines
While both agencies demand a robust “totality of the evidence,” their emphasis and specific requirements can differ.
- Pharmacokinetic Studies: The EMA has traditionally shown a preference for single-dose crossover studies for PK assessment, whereas the FDA is often more accepting of parallel-group designs, particularly for biologics with long half-lives where a crossover design is impractical.
- Reference Product Sourcing: The EMA generally requires that the reference product used in comparative studies be one that is sourced from within the European Economic Area (EEA). The FDA requires the use of a U.S.-licensed reference product. This creates a significant logistical and financial challenge for developers seeking global approval, often forcing them to run separate “bridging studies” to link the data from U.S.- and EU-sourced reference products.
- The Concept of Interchangeability: The U.S. BPCIA created a separate, higher standard called “interchangeability.” An interchangeable biosimilar can be substituted for the reference product at the pharmacy level without the intervention of the prescribing physician (subject to state pharmacy laws). To achieve this designation, a developer must conduct additional studies, typically “switching studies,” demonstrating that alternating between the reference product and the biosimilar causes no increased risk or diminished efficacy compared to remaining on the reference product alone [5]. The EMA does not have a formal designation of interchangeability; substitution policies are decided at the national level by individual EU member states.
The Concept of Extrapolation: A Major Cost-Saver
Perhaps one of the most powerful and commercially significant concepts in biosimilar development is extrapolation. This is the idea that if biosimilarity is established in one therapeutic indication, it may be possible to approve the biosimilar for other indications of the reference product without conducting dedicated clinical trials in those other indications [6].
For example, if a biosimilar to adalimumab (Humira) demonstrates equivalent efficacy, safety, and immunogenicity in patients with rheumatoid arthritis, regulators may be willing to extrapolate that finding and also approve it for psoriasis, Crohn’s disease, and other approved indications of Humira. This is a massive advantage, saving developers the enormous cost and time of running separate confirmatory trials for every single indication.
The justification for extrapolation rests on the “totality of the evidence.” If the analytical and PK data are strong, and the mechanism of action of the drug is the same across different diseases, regulators can be confident that the biosimilar will behave similarly in all approved patient populations. Both the FDA and EMA support extrapolation, but they may require detailed scientific justification, particularly if the drug’s mechanism of action differs between indications or if different patient populations present unique safety concerns.
Harmonization and Divergence: Navigating Other Key Markets (e.g., Japan’s PMDA, Health Canada)
Beyond the FDA and EMA, other major regulatory bodies have established their own biosimilar pathways. Japan’s Pharmaceuticals and Medical Devices Agency (PMDA) and Health Canada largely follow principles similar to the EMA, having established their frameworks relatively early. However, subtle differences in data requirements, particularly around the reference product source and the acceptance of foreign clinical data, still exist.
For a company with global ambitions, the ultimate goal is to design a single, global clinical development program that can satisfy the requirements of multiple regulatory agencies simultaneously. This “holy grail” requires deep regulatory intelligence, proactive engagement with agencies (through formal meetings like FDA Type 2 meetings or EMA Scientific Advice), and a meticulously designed program that incorporates elements to satisfy the most stringent requirements of each target market. For example, a global program might use a three-arm PK study (Biosimilar vs. U.S. Reference vs. EU Reference) to build the necessary data bridge from the outset.
Navigating this global regulatory tapestry is the first and most critical strategic step. A misreading of the map can lead you down a dead-end path, while a well-plotted course can set you on the fast track to global market access.
Laying the Groundwork: The Crucial Role of Pre-Clinical and Analytical Characterization
If the biosimilar development program is a skyscraper, then the analytical and pre-clinical data form its deep and expansive foundation. This is where the case for biosimilarity is first built, and its strength determines the stability and height of the entire structure. In the modern biosimilar paradigm, the emphasis has dramatically shifted “left,” concentrating the most intensive scientific scrutiny on this earliest phase. The philosophy is simple: if you can comprehensively demonstrate that your molecule is, for all practical purposes, a structural and functional twin of the reference product, the need for extensive, large-scale human testing diminishes significantly. This is the cornerstone of the streamlined development pathway.
The Analytical Pyramid: The Foundation of Biosimilarity
The FDA and EMA both view the evidence for biosimilarity as a pyramid. The broad, heavy base of this pyramid is composed of extensive and sophisticated analytical characterization. This is the most critical data set in the entire submission.
“The foundation of a successful biosimilar program is built in the laboratory, not the clinic. Advances in analytical science have given us an unprecedented ability to characterize these complex molecules. A robust analytical similarity package is the most convincing piece of evidence a developer can present to a regulator, as it provides the scientific rationale for why the clinical performance is expected to be the same.”
— Statement from the International Generic and Pharmaceutical Medicines Association (IGPA) Biosimilars Committee [7]
The goal of this analytical exercise is to create a high-resolution “fingerprint” of both the biosimilar candidate and the reference product and then overlay them to find a match. This isn’t a single test, but a battery of orthogonal methods designed to probe every conceivable attribute of the protein.
State-of-the-Art Analytical Techniques (e.g., Mass Spectrometry, NMR)
Developers employ a vast arsenal of cutting-edge technologies to dissect these molecules. This isn’t just about ticking boxes; it’s about using the right tool for the right question to build a holistic picture.
- Primary Structure Analysis: This confirms that the fundamental building blocks are correct. Techniques like mass spectrometry (MS) and Edman degradation are used to verify the amino acid sequence is identical to that of the reference product. Any deviation here is an immediate red flag and likely a program-killer.
- Higher-Order Structure (HOS) Analysis: Proteins are not just strings of amino acids; they are folded into complex 3D shapes that are critical for their function. This HOS is assessed using a suite of biophysical methods:
- Circular Dichroism (CD): Measures the secondary structure (alpha-helices and beta-sheets).
- Fourier-Transform Infrared Spectroscopy (FTIR): Also provides information on secondary structure.
- Nuclear Magnetic Resonance (NMR): Can provide an exquisitely detailed 3D structural map, though it’s often complex and reserved for smaller biologics.
- X-ray Crystallography: The gold standard for 3D structure, but challenging to perform for large, flexible antibodies.
- Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS): A powerful technique that measures the “breathing” of the protein, revealing its conformational dynamics and flexibility. This can detect subtle differences in folding that other methods might miss.
- Post-Translational Modifications (PTMs): Living cells decorate proteins with various chemical modifications after they are synthesized. The most critical of these for many biologics is glycosylation, the pattern of sugar chains attached to the protein. These “glycans” can dramatically impact a protein’s stability, half-life, and immunogenicity. An array of techniques, including liquid chromatography-mass spectrometry (LC-MS), are used to meticulously map and compare the glycosylation profiles of the biosimilar and the reference product. Other PTMs like oxidation and deamidation are also scrutinized.
- Purity, Impurities, and Aggregation: The analysis must also show that the product is pure and that any process-related impurities (e.g., host cell proteins, DNA) are controlled to safe levels. A critical focus is on aggregation, where protein molecules clump together. Aggregates are a major safety concern as they are often highly immunogenic. Techniques like size-exclusion chromatography (SEC) and dynamic light scattering (DLS) are used to quantify and characterize aggregates.
Identifying Critical Quality Attributes (CQAs)
Not all molecular attributes are created equal. A Critical Quality Attribute (CQA) is a physical, chemical, biological, or microbiological attribute that must be controlled within a specific limit to ensure the desired product quality, safety, and efficacy [8].
The first step in designing the analytical program is to identify the likely CQAs for the reference product. This is done through a combination of literature review, deep understanding of the molecule’s structure-function relationship, and risk assessment. For a monoclonal antibody, CQAs would include things like:
- Correct primary amino acid sequence.
- Antigen binding affinity.
- Fc receptor binding (which mediates its effector functions).
- Specific glycosylation patterns known to affect half-life or function.
- Levels of aggregation and fragmentation.
The entire analytical program is then designed to compare the biosimilar and reference product across all these identified CQAs. The goal is to show that any minor differences observed are not statistically significant and, more importantly, fall within a pre-defined “equivalence range” that is known to be clinically irrelevant.
In Vitro Functional Assays: Proving Biological Equivalence Before Human Trials
Showing that two proteins look the same isn’t enough; you must also show they act the same. This is the role of in vitro functional assays. These laboratory-based tests measure the biological activity of the drug, providing a direct link between its structure and its clinical effect.
For a monoclonal antibody like rituximab, which targets the CD20 protein on B-cells, the functional assays would be designed to measure its key mechanisms of action:
- Antigen Binding: An ELISA or surface plasmon resonance (SPR) assay would be used to show that the biosimilar binds to CD20 with the same affinity and kinetics as the reference product.
- Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC): This is a key mechanism for rituximab, where the antibody flags cancer cells for destruction by immune cells (like Natural Killer cells). A cell-based assay would be used to demonstrate equivalent ADCC activity.
- Complement-Dependent Cytotoxicity (CDC): Another mechanism where the antibody activates the complement system to kill target cells. Again, a cell-based assay would compare the CDC potency of the biosimilar and the reference product.
A comprehensive panel of such functional assays, covering all known mechanisms of action, provides powerful evidence that the biosimilar will perform as expected in patients. Strong concordance in these assays can significantly de-risk the subsequent clinical program.
Animal Studies: When and Why They Are Still Necessary
With the power of modern analytics, the role of animal studies in biosimilar development has evolved. They are no longer a default requirement but are used strategically to address specific questions that cannot be answered in vitro.
The most common reason to conduct an animal study is for a comparative in vivo PK/PD assessment. This is especially important if there are minor differences in CQAs (like glycosylation) that could theoretically impact the drug’s half-life or distribution in a living system. A study in a relevant animal species (often non-human primates for monoclonal antibodies) can provide reassurance that these minor differences have no in vivo consequences.
In some cases, a toxicology study in animals may be requested by regulators, particularly if the biosimilar has a novel manufacturing process or contains impurities that are different from the reference product. However, the trend is towards reducing and refining the use of animals. The FDA’s 2022 guidance, for example, explicitly states that animal toxicity data may be unnecessary if the developer provides a strong scientific justification based on other evidence [9].
Ultimately, the pre-clinical and analytical package is about building an irrefutable scientific argument. It’s a painstaking process of characterization and comparison that, when done correctly, leaves regulators with very few “residual uncertainties.” It’s this lack of uncertainty that paves the way for a streamlined, targeted, and ultimately successful clinical trial program.
Designing the Core Engine: Pharmacokinetic (PK) and Pharmacodynamic (PD) Studies
If analytical characterization is the foundation, then pharmacokinetic (PK) and pharmacodynamic (PD) studies are the core engine of the biosimilar clinical program. This is the critical “bridging” phase where we move from the laboratory bench to human subjects for the first time. The data generated here provide the first direct, in-vivo confirmation that the biosimilar behaves in the human body just like the reference product. A successful PK/PD program is a massive step towards regulatory approval and can dramatically influence the design—and even the necessity—of the large, expensive confirmatory efficacy trial.
The Pharmacokinetic Bridge: Demonstrating Bioequivalence
Pharmacokinetics is the study of “what the body does to the drug.” It tracks the journey of the drug through the body—its absorption, distribution, metabolism, and excretion (ADME). For a biosimilar, the primary goal of the PK study is to demonstrate that your product has the same concentration-time profile in the blood as the reference product. In essence, you are proving that the same dose delivers the same amount of drug to the site of action for the same amount of time. This concept is known as bioequivalence.
Study Design Principles: Crossover vs. Parallel Group Designs
The choice of study design is a critical strategic decision. The two most common designs for biosimilar PK studies are the single-dose crossover design and the parallel-group design.
- Two-Way Crossover Design: This is often considered the gold standard for PK studies when feasible. A group of subjects (typically healthy volunteers) is randomized. Half receive the biosimilar first, followed by a “washout” period (long enough for the drug to be completely eliminated from the body), and then they receive the reference product. The other half receives the drugs in the reverse order. The key advantage here is that each subject acts as their own control. This dramatically reduces variability because you are comparing the two drugs within the same person, eliminating inter-subject differences in metabolism and clearance. This statistical efficiency means you can often use a smaller number of subjects to achieve the required statistical power, saving time and money. However, this design is only practical for drugs with a relatively short half-life. For monoclonal antibodies, which can have half-lives of several weeks, the required washout period would be impractically long (often 5-6 months or more), making a crossover study impossible.
- Parallel Group Design: This is the standard design for biologics with long half-lives. Two separate groups of subjects are randomized. One group receives only the biosimilar, and the other group receives only the reference product. Blood samples are then collected over a long period to characterize the full PK profile. Because you are comparing two different groups of people, inter-subject variability is a much bigger factor. This means you will need a larger sample size to be confident that any observed differences are due to the drugs and not just random variation between the two groups. The statistical analysis is a straightforward comparison of the average PK parameters between the two arms.
The choice is dictated by the science of the molecule. For a product like filgrastim (Neupogen), with a half-life of a few hours, a crossover study is perfect. For adalimumab (Humira), with a half-life of 2-3 weeks, a parallel-group design is the only option.
Selecting the Right Population: Healthy Volunteers vs. Patients
Another key decision is whom to conduct the study in.
- Healthy Volunteers: For most biosimilar PK studies, healthy volunteers are the preferred population. Why? Because they provide a “clean” system. They are typically not taking other medications that could interfere with the drug’s PK (drug-drug interactions), and they don’t have the underlying disease, which itself can sometimes alter how a drug is processed. This reduces variability and makes the study more sensitive to detecting potential real differences between the biosimilar and the reference product.
- Patients: In some cases, a study in the target patient population is necessary or preferred. This might be the case for drugs with significant safety concerns that would make it unethical to administer them to healthy individuals (e.g., some oncology drugs). It can also be required if the disease state is known to significantly affect the drug’s PK. For example, some antibodies are cleared more rapidly in patients with a high disease burden. Conducting the study in patients can sometimes be more efficient, as you can combine the PK assessment with a PD and immunogenicity assessment in the same trial.
Key PK Parameters: AUC, Cmax, and the 90% Confidence Interval
The PK study measures the drug concentration in blood (or serum/plasma) at numerous time points after administration. From these measurements, we calculate several key PK parameters. The most important are:
- Cmax (Maximum Concentration): The peak concentration the drug reaches in the blood.
- AUC (Area Under the Curve): The total drug exposure over time. This is calculated from the concentration-time curve and is represented as AUC_0−t (exposure up to the last measurement time) and AUC_0−infty (total exposure extrapolated to infinity).
To declare bioequivalence, the developer must show that their biosimilar is statistically equivalent to the reference product for these key parameters. The standard statistical test is to calculate the 90% confidence interval (CI) for the ratio of the geometric means (Biosimilar/Reference) for Cmax and AUC. To pass the test, this 90% CI must fall entirely within a pre-specified equivalence margin, which is typically 80% to 125% [10].
This statistical endpoint is non-negotiable. If the 90% CI for your AUC ratio is, for example, 85% to 127%, you have failed the study, even though the point estimate might be very close to 100%. The upper bound of 127% falls outside the 125% limit. This demonstrates the incredible rigor required and why meticulous study conduct and precise bioanalysis are paramount.
The Pharmacodynamic Link: Measuring the Drug’s Effect on the Body
Pharmacodynamics (PD) is the study of “what the drug does to the body.” It measures the physiological or biochemical effect of the drug. If a relevant PD biomarker exists, a comparative PD study is a powerful tool for demonstrating biosimilarity because it provides a direct measure of the drug’s biological activity in humans.
Choosing Relevant PD Biomarkers
A good PD biomarker should be:
- Relevant to the drug’s mechanism of action.
- Sensitive to changes in drug exposure.
- Accurate and precise to measure.
For example, for biosimilars of filgrastim (a colony-stimulating factor), the absolute neutrophil count (ANC) is a perfect PD biomarker. Filgrastim’s job is to stimulate the production of neutrophils, so measuring the change in ANC over time provides a direct readout of the drug’s activity.
Similarly, for insulin biosimilars, a euglycemic clamp study is the gold standard. In this procedure, insulin is infused, and glucose is infused simultaneously at a variable rate to “clamp” the blood sugar at a normal level. The glucose infusion rate (GIR) required to maintain this clamp is a direct measure of the insulin’s activity.
The Challenge of PD Studies for Biologics Without Clear Biomarkers
Unfortunately, for many of the most complex and lucrative biologics, especially monoclonal antibodies used in immunology and oncology, there are no simple, validated PD biomarkers. What biomarker do you measure for adalimumab? It affects a whole cascade of inflammatory cytokines, and no single marker accurately reflects its overall clinical effect.
In these situations, a standalone PD study is not feasible. The assessment of the drug’s effect must come from the clinical efficacy endpoints in the confirmatory trial. However, regulators still expect developers to explore potential biomarkers. You might measure a panel of exploratory biomarkers (e.g., C-reactive protein, various cytokines) as part of the main clinical trial. While this data may not be used for a primary equivalence assessment, it can provide valuable supportive evidence for the “totality of the evidence” package.
A successful PK/PD program is a monumental achievement in a biosimilar’s journey. It provides the strong, human-based scientific rationale that allows you to confidently approach regulators and say, “Our product is absorbed the same, is exposed the same, and, where we can measure it, has the same biological effect. Therefore, you can have high confidence it will have the same clinical outcome.” This sets the stage for the final act: the confirmatory clinical trial.
The Final Frontier: Designing and Executing Confirmatory Clinical Efficacy and Safety Trials
We have arrived at the apex of the development pyramid: the confirmatory clinical trial. This is often the largest, longest, most complex, and most expensive single study in the entire biosimilar program. While the foundation of biosimilarity is built on analytical and PK data, the confirmatory trial serves as the ultimate validation—the final, definitive piece of evidence designed to erase any lingering “residual uncertainty” about the product’s clinical performance. The stakes here are immense. A successful trial paves the path to market, while a failed or ambiguous one can be a fatal blow to the entire program.
The Equivalence Trial: The Linchpin of Clinical Confirmation
Unlike a trial for a novel drug, which aims to prove superiority over a placebo or standard of care, a biosimilar confirmatory trial is typically designed as an equivalence trial (or sometimes a non-inferiority trial). The goal is not to show that your drug is better; the goal is to show that it is not clinically meaningfully different from the reference product. You are trying to prove a negative, which presents unique statistical and clinical challenges.
Defining Equivalence Margins: A Statistical and Clinical Tightrope Walk
The most critical and often most debated aspect of designing an equivalence trial is setting the equivalence margin. This is the pre-defined range around the reference product’s effect within which the biosimilar’s effect must lie to be considered clinically equivalent.
Think of it as walking a tightrope. The margin must be narrow enough to be clinically reassuring—that is, to ensure that you are ruling out any meaningful difference in efficacy. If the margin is too wide (e.g., +/- 20%), a biosimilar could be statistically “equivalent” but still be noticeably less effective than the reference product. Regulators and physicians would reject such a wide margin.
On the other hand, the margin cannot be so narrow that it becomes practically impossible to achieve, requiring a mega-trial with tens of thousands of patients. The trial must be feasible.
Setting the margin is a complex exercise that involves:
- Historical Data Analysis: You must analyze the data from the original pivotal trials of the reference product to understand its effect size and variability.
- Clinical Judgment: What is the smallest difference in outcome that would be considered clinically important by doctors and patients? This is not just a statistical question but a clinical one.
- Regulatory Negotiation: The proposed margin must be justified and agreed upon with regulatory agencies (like the FDA and EMA) before the trial begins. This is a crucial point of discussion in scientific advice meetings.
For example, in a rheumatoid arthritis trial using the ACR20 response rate (a 20% improvement in symptoms) as the primary endpoint, the equivalence margin might be set at +/- 13%. This means the 95% confidence interval for the difference in response rates between the biosimilar and the reference product must fall entirely within that -13% to +13% window [11].
Choosing the Most Sensitive Patient Population and Endpoints
To design an efficient and powerful equivalence trial, you need to maximize your ability to detect a true difference between the products if one exists. This means choosing the most sensitive experimental conditions:
- Sensitive Patient Population: You want to study the product in a patient population where the drug is known to have a large effect and where the disease is relatively homogeneous. For a product approved for multiple indications, you would typically choose the indication that is considered most sensitive for detecting potential differences in both efficacy and immunogenicity. For instance, psoriasis is often chosen for anti-TNF biosimilars because the skin plaques provide a very sensitive and objective measure of efficacy (the PASI score), and the patient population is known to be sensitive to immunogenicity issues.
- Sensitive Primary Endpoint: The primary endpoint of the study must be objective, reliable, and clinically relevant. For oncology biosimilars, this might be Overall Response Rate (ORR) rather than Overall Survival (OS). Why? Because ORR is a more direct measure of the drug’s anti-tumor activity and can be assessed much earlier, making the trial shorter and more sensitive to direct drug effects. OS can be influenced by many other factors, such as subsequent lines of therapy, making it a “noisier” endpoint for an equivalence study.
The design is typically a randomized, double-blind, parallel-group study comparing the biosimilar to the reference product. A placebo arm is generally considered unethical if an effective treatment (the reference product) exists.
The Specter of Immunogenicity: A Critical Safety Consideration
Immunogenicity—the propensity of a biologic drug to trigger an unwanted immune response in the body—is arguably the single greatest safety concern for biosimilars. The human immune system can recognize a therapeutic protein as “foreign” and generate anti-drug antibodies (ADAs). These ADAs can have several negative consequences:
- Neutralizing ADAs: They can bind to the drug and block its activity, leading to a loss of efficacy.
- Binding ADAs: They can bind to the drug and increase its clearance from the body, also reducing efficacy.
- Safety Issues: In rare cases, ADAs can cause hypersensitivity reactions or even cross-react with a patient’s own natural proteins, leading to serious autoimmune-like side effects.
Because even minor differences in protein structure, impurities, or formulation can potentially alter immunogenicity, a head-to-head comparison of the immunogenicity profiles of the biosimilar and the reference product is a non-negotiable regulatory requirement.
Designing a Robust Immunogenicity Assessment Plan
Your confirmatory trial must include a pre-specified, robust plan for collecting samples and testing for ADAs. This involves:
- Frequent Sampling: Blood samples for ADA testing should be collected at baseline (before the first dose), at multiple time points during the study, and at the end of the study. A final sample well after the last dose is also important to detect late-onset immune responses.
- Sufficient Duration: The trial needs to be long enough to allow for the development and detection of an immune response. For many chronic diseases, this means a study duration of at least 6 to 12 months.
Assay Development: Tiers of Testing (Screening, Confirmatory, Neutralizing)
The laboratory testing for ADAs is a complex, multi-tiered process. You can’t just run a single test. The industry standard is a three-tiered approach:
- Screening Assay: A highly sensitive assay (like an ELISA) is used to screen all patient samples. This test is designed to have a very low rate of false negatives, meaning it will catch almost every sample that might possibly contain ADAs. The trade-off is that it may have a higher rate of false positives.
- Confirmatory Assay: Any sample that tests positive in the screening assay is then subjected to a confirmatory assay. This test is more specific and is designed to confirm whether the positive result was due to true ADAs or some other interference.
- Neutralizing Assay (NAb): All confirmed positive samples are then tested in a neutralizing assay. This is typically a cell-based functional assay that determines whether the ADAs have the ability to block the drug’s biological activity. This is the most clinically important information.
Developing and validating these three assays is a significant undertaking in itself and must be completed long before the clinical trial starts.
Interpreting Immunogenicity Data: Clinical Relevance is Key
The goal is to demonstrate that there are no clinically meaningful differences in the incidence, titer (amount), and nature (e.g., neutralizing vs. non-neutralizing) of ADAs between the biosimilar and reference product groups. It’s not enough to just report the numbers. You must analyze the clinical impact. Did patients who developed ADAs have a lower response rate? Did they have more infusion reactions? This correlation of immunogenicity with clinical outcomes (efficacy and safety) is the final, critical step in the assessment.
The Switching Study: Building Physician and Patient Confidence
In the U.S., there is a higher regulatory bar known as “interchangeability.” An interchangeable biosimilar has been shown to be safe to switch back and forth with the reference product. To gain this commercially valuable designation, a separate switching study is usually required [5].
The Value Proposition of Interchangeability
An interchangeable designation is highly sought after because it allows for automatic substitution at the pharmacy level (where state law permits), which can dramatically accelerate market uptake. It provides a powerful signal of confidence to physicians, payers, and patients that the biosimilar is truly a seamless replacement for the innovator product.
Designing Studies with Multiple Switches to Mimic Real-World Use
A typical switching study design involves at least three treatment periods. For example:
- All patients start on the reference product for a period to establish a stable response.
- Patients are then randomized. One group stays on the reference product (the control arm). The other group switches to the biosimilar.
- After another period, the biosimilar group might switch back to the reference product, and then back again to the biosimilar, with the study continuing.
This design with multiple switches is intended to mimic a real-world scenario where a patient’s prescription might be filled with either the reference or the biosimilar depending on pharmacy stock or payer preference. The primary endpoints of a switching study are typically comparisons of PK, safety (especially immunogenicity), and efficacy between the arm that stayed on the reference product and the arm that underwent multiple switches. The goal is to show that switching is no different from staying put.
Executing these confirmatory and switching trials is the operational peak of the development journey. It requires flawless execution, from site management and patient recruitment to data analysis and regulatory submission, all under the immense pressure of timelines and budgets.
Strategic Execution: Operational Excellence in Biosimilar Trials
Designing a brilliant clinical trial on paper is one thing. Executing it flawlessly in the real world is an entirely different beast. The operational side of biosimilar clinical trials presents a unique set of challenges that can make or break a program. In the competitive race to market, operational excellence is not a “nice to have”—it’s a core competency. Delays in recruitment, hiccups in the supply chain, or errors in data management can lead to budget overruns and, more critically, cede a first-mover advantage to a competitor.
Site Selection and Patient Recruitment: The Race Against Time
Patient recruitment is consistently one of the biggest bottlenecks in all of clinical research, and for biosimilars, the challenge is amplified. You are often running trials in crowded therapeutic areas like rheumatoid arthritis, oncology, or psoriasis, where dozens of other trials (for both novel drugs and other biosimilars) are competing for the same limited pool of patients.
Targeting “Trial-Naive” vs. “Treatment-Experienced” Patients
A key strategic decision is the type of patient to enroll.
- Biologic-Naive Patients: Enrolling patients who have never been treated with the reference biologic (or any other biologic for their condition) is often the “cleanest” approach from a scientific perspective. It eliminates confounding factors from prior treatments and provides a clearer picture of the drug’s efficacy and, importantly, its de novo immunogenicity profile. This is the preferred population for many confirmatory trials. The challenge? Finding these patients can be incredibly difficult, especially for diseases where biologics have been the standard of care for over a decade.
- Treatment-Experienced (Stable) Patients: An alternative, particularly for switching studies, is to enroll patients who are already on the reference product and are stable. You then randomize them to either stay on the reference or switch to the biosimilar. This recruitment pool is often larger, but the study design is more complex, and you must carefully assess the impact of the switch on efficacy and safety.
A successful recruitment strategy requires a multi-pronged approach: working with high-performing clinical sites with proven track records, leveraging patient advocacy groups, and using sophisticated digital outreach and pre-screening tools to identify potential candidates. Time is of the essence, and every day a trial site is open but not enrolling is a day of lost opportunity.
Overcoming Recruitment Hurdles in Crowded Therapeutic Areas
How do you stand out in a crowded field? One key is making participation as easy as possible for both the site and the patient. This means a well-designed protocol that isn’t overly burdensome with excessive tests or visits. It also means providing excellent support to the clinical sites.
Another challenge is the “no-win” perception. Some patients may be hesitant to enroll in a biosimilar trial because there’s a 50% chance they will get the reference product they could already be prescribed, and a 50% chance they get an “investigational” product that is designed to be no better. Communicating the value proposition—that participation helps bring lower-cost alternatives to market for all patients—is crucial.
The Supply Chain Challenge: Sourcing and Managing the Reference Product
This is a unique and fiendishly complex problem for biosimilar developers. You need to procure large quantities of the innovator’s reference product to use as the comparator in your clinical trials. This is not as simple as placing an order.
First, it is incredibly expensive. You may need to purchase millions of dollars’ worth of your competitor’s drug on the open market. Second, the innovator company is, understandably, not going to make this easy for you. They have no obligation to sell you their product directly for the purpose of being copied. This often forces developers to use third-party distributors to procure the drug, adding complexity and cost.
Ensuring Consistency Across Different Lots of the Reference Product
The reference product itself is a biologic and has inherent batch-to-batch variability. Your clinical trial might span a year or more, during which time the innovator may change its manufacturing process or release new lots of the drug with slightly different quality attributes.
It is absolutely critical for the biosimilar developer to obtain multiple batches of the reference product over time, perform extensive analytical testing on them, and demonstrate to regulators that the specific lots used in the clinical trial are representative of the reference product as a whole. This “bridging” of reference product lots is a critical part of the submission package. Failure to do so can call the validity of the entire comparative trial into question.
Navigating the Complexities of Global Sourcing and Blinding
For a global trial aimed at satisfying both the FDA and EMA, the supply chain becomes even more tangled. You must source both U.S.-licensed reference product and EEA-sourced reference product. You then need a robust system to manage and track these different supplies across clinical sites around the world.
Furthermore, the trial must be double-blinded. Neither the patient nor the investigator should know whether they are receiving the biosimilar or the reference product. This requires a specialized clinical supply team to package both drugs in identical vials, syringes, or pens and label them with randomized codes. Any difference in packaging, color, or even the viscosity of the liquid during injection could unblind the study and compromise its integrity.
Data Management and Biostatistics: Ensuring Integrity and Rigor
In the world of biosimilar trials, the data is everything. The entire program culminates in a statistical verdict: did the confidence interval fall within the equivalence margin or not? There is no room for error or ambiguity.
This demands a state-of-the-art approach to data management and biostatistics.
- Electronic Data Capture (EDC): Modern trials rely on EDC systems where data is entered directly at the clinical site, allowing for real-time data cleaning and query resolution. This is far superior to old-fashioned paper case report forms.
- Risk-Based Monitoring: Instead of monitoring 100% of the data at every site, a more efficient “risk-based” approach focuses intensive monitoring on the sites and data points that are most critical to the study’s outcome (e.g., primary endpoint data, safety events, and drug accountability).
- Centralized Statistical Monitoring: Sophisticated statistical techniques can be used to monitor incoming data centrally, looking for unusual patterns or outliers at specific sites that might indicate errors or even fraud.
The Importance of a Pre-specified Statistical Analysis Plan (SAP)
Perhaps the most important document, aside from the protocol itself, is the Statistical Analysis Plan (SAP). This highly detailed document is written before the trial data is unblinded and locked. It prespecifies exactly how the data will be handled and analyzed: how missing data will be treated, what statistical tests will be used for the primary and secondary endpoints, how subgroups will be analyzed, and so on.
Having a locked-down SAP prevents “data dredging” or “p-hacking”—the temptation to keep analyzing the data in different ways until you find a result you like. Regulators scrutinize the SAP to ensure the analysis was objective and scientifically rigorous. Any deviation from the SAP must be thoroughly justified.
In summary, operational execution is the powerful, often unseen, current that carries the ship of biosimilar development forward. A brilliant design can easily be sunk by poor execution, while operational excellence can navigate even the most challenging waters to bring a product safely to the shores of regulatory approval and market launch.
The Digital Transformation of Biosimilar Trials
Just as technology is revolutionizing every other aspect of our lives, it is also profoundly reshaping the world of clinical development. For biosimilar developers, who operate in a hyper-competitive environment where speed, efficiency, and data quality are paramount, embracing this digital transformation is not an option—it’s a strategic necessity. From decentralized trial models to the power of real-world evidence, digital tools are offering new ways to overcome old challenges, accelerate timelines, and build a more compelling case for biosimilarity.
Decentralized Clinical Trials (DCTs): A New Model for Biosimilar Studies?
The traditional clinical trial model is site-centric. It requires patients to travel, often long distances, to a specific hospital or clinic for every visit, assessment, and procedure. This creates a significant burden on patients, limits participation to those who live near a research site, and slows down recruitment.
Decentralized Clinical Trials (DCTs), or “hybrid” trials, offer a more patient-centric alternative. They leverage a suite of digital technologies to move parts of the trial out of the clinic and into the patient’s home. For a biosimilar trial, this could look like:
- Telehealth Visits: Routine follow-up visits can be conducted via secure video calls, saving the patient time and travel costs.
- Home Health Nursing: A trained nurse can visit the patient’s home to administer the study drug (if it’s an injection), draw blood for PK or ADA testing, and assess for side effects.
- Wearable Sensors and ePROs: Patients can use wearable devices (like smartwatches or activity trackers) to continuously collect objective data (e.g., activity levels, sleep patterns). They can also report symptoms and quality of life information directly through an app on their smartphone using electronic Patient-Reported Outcome (ePRO) tools.
- Direct-to-Patient Drug Shipment: The study drug can be shipped directly to the patient’s home from a central pharmacy, bypassing the site’s pharmacy altogether.
While a fully “siteless” trial is still rare, a hybrid model that blends on-site visits for key procedures (like initial screening or imaging) with decentralized elements for more routine follow-up is becoming increasingly popular. The benefits for biosimilar trials are clear:
- Accelerated Recruitment: By removing geographical barriers, you can recruit from a much wider patient pool.
- Improved Patient Retention: A more convenient trial experience means patients are more likely to stay enrolled until the end.
- Richer Data: Continuous data from wearables can provide a more holistic view of the patient’s experience than episodic data collected only during site visits.
Of course, DCTs also present new challenges in logistics, data security, and regulatory oversight, but their potential to make trials faster, more efficient, and more patient-friendly is undeniable.
Leveraging Real-World Evidence (RWE) and Real-World Data (RWD)
The data collected within the controlled environment of a randomized clinical trial (RCT) is essential for regulatory approval. But what happens after the product is launched? How does it perform in the messy, unpredictable “real world”? This is where Real-World Data (RWD) and Real-World Evidence (RWE) come into play.
- Real-World Data (RWD): This is health data collected from sources outside of traditional clinical trials. This includes electronic health records (EHRs), insurance claims data, data from patient registries, and even data from mobile devices and wearables.
- Real-World Evidence (RWE): This is the clinical evidence derived from the analysis of RWD.
For biosimilar developers, RWE is becoming an increasingly powerful tool across the product lifecycle.
Post-Marketing Surveillance and Safety Monitoring
Once a biosimilar is approved, regulators require the manufacturer to conduct post-marketing surveillance to monitor its long-term safety. This is especially important for detecting rare side effects or immunogenicity issues that might not have appeared in the pre-approval clinical trial.
Instead of running a costly and slow prospective registry study, developers can now leverage massive RWD sources like insurance claims databases. By analyzing the records of tens of thousands of patients who have been prescribed their biosimilar, they can efficiently monitor safety trends and compare them to patients on the reference product, providing continuous reassurance to regulators and clinicians.
Supporting Extrapolation and Payer Negotiations
RWE is also playing a growing role in supporting the case for biosimilarity itself. While an RCT in one indication is still the cornerstone for initial approval, RWE can be used to bolster the argument for extrapolation to other indications. For example, if your biosimilar is approved for rheumatoid arthritis based on an RCT, you can then analyze EHR data to show that in the real world, patients with psoriasis who are switched to your biosimilar have the same outcomes as those who remain on the reference product. This RWE can provide powerful support for getting the psoriasis indication officially added to your label.
Furthermore, RWE is critical in negotiations with payers (insurance companies and health systems). Payers want to see evidence that a biosimilar not only saves money but also delivers the same clinical outcomes in their specific patient populations. A well-executed RWE study can demonstrate the real-world value of the biosimilar, securing its place on the formulary and driving market access. As one industry expert, Dr. Evelyn Conrad, a health economics consultant, states, “For payers, the randomized trial gets a biosimilar in the door. Real-world evidence is what keeps it on the formulary and proves its value year after year.”
The digital transformation is not just about adopting new gadgets; it’s about a fundamental shift towards a more data-driven, patient-centric, and efficient model of clinical development. For biosimilar developers, harnessing these digital tools is a key strategy for navigating the competitive landscape and delivering on the promise of high-quality, affordable biologics.
Beyond the Trial: Commercial and Market Access Strategies
The journey of a biosimilar doesn’t end with a successful clinical trial and a regulatory approval letter. In many ways, that’s just the end of the beginning. The ultimate success of a biosimilar is not measured by its p-values, but by its market share. This requires a sophisticated commercial and market access strategy that must be developed in parallel with the clinical program, not as an afterthought. You can have the most scientifically perfect biosimilar in the world, but if you can’t get it on formulary, convince physicians to prescribe it, and navigate the complex patent landscape, the entire multi-hundred-million-dollar investment can fail.
The Role of Patent Intelligence in Biosimilar Strategy
Long before the first analytical test is run, the entire biosimilar project begins with a crucial question: which molecule do we target? The answer is inextricably linked to the world of intellectual property. The innovator company protects its blockbuster biologic with a dense thicket of patents—not just on the molecule itself, but on the manufacturing process, the formulation, the method of use for specific diseases, and even the delivery device. This is often referred to as a “patent estate” or “patent thicket.”
Navigating this thicket is a high-stakes legal and strategic challenge. A biosimilar can only be launched after the key patents on the reference product have expired or have been successfully challenged in court. This is where specialized patent intelligence becomes an invaluable strategic tool.
Using Services like DrugPatentWatch to Identify Opportunities and Mitigate Risks
The decision of which biosimilar to pursue is a multi-billion dollar bet. To make this bet, companies need a clear and comprehensive view of the patent landscape. This involves identifying all relevant patents, understanding when they expire, and assessing their strength and the likelihood of a successful legal challenge. This is an incredibly complex and specialized task.
This is precisely where services like DrugPatentWatch provide critical value. Platforms like this aggregate and analyze vast amounts of patent and regulatory data, providing biosimilar developers with the actionable intelligence they need to make informed decisions. By using DrugPatentWatch, a company can:
- Identify an “at-risk” launch opportunity: Pinpoint the exact dates when key patents are set to expire, defining the earliest possible launch window.
- Analyze the entire patent estate: Go beyond the primary compound patent to map out the web of secondary patents on manufacturing, formulation, and indications that the innovator will use to defend its franchise.
- Monitor patent litigation: Keep track of legal challenges filed by other biosimilar competitors. The outcome of these “patent dance” litigations can dramatically alter the strategic landscape for everyone.
- Inform portfolio strategy: By providing a clear view of the patent landscape for dozens of potential reference products, this intelligence allows companies to prioritize their development pipeline, focusing resources on molecules with the clearest and most profitable path to market.
Without this deep patent intelligence, a company is flying blind. They risk investing hundreds of millions in developing a biosimilar only to find themselves blocked by an unexpected patent or beaten to market by a competitor with a better legal strategy.
Communicating the “Totality of the Evidence” to Stakeholders
Once a biosimilar is approved, the battle for hearts and minds begins. You have convinced the regulators, but now you must convince the end-users: physicians, pharmacists, payers, and patients. These stakeholders are not regulatory scientists; they need the complex story of biosimilarity translated into a clear and compelling narrative. You cannot simply show them a 90% confidence interval and expect them to be convinced.
Educating Physicians, Payers, and Patients
A robust medical affairs and marketing strategy is crucial. This involves:
- Physician Education: Medical science liaisons (MSLs) must be deployed to meet with key opinion leaders and prescribing physicians to walk them through the “totality of the evidence.” This means presenting the analytical data, the PK bridge, the confirmatory trial results, and especially the immunogenicity data in an accessible way. The goal is to build trust and confidence in the science behind the biosimilar.
- Payer Communication: Payers and pharmacy benefit managers (PBMs) are primarily focused on cost, but they also need to be assured of clinical equivalence. The economic value proposition (the savings the biosimilar offers) must be presented alongside a clear summary of the clinical data package. Real-world evidence can be particularly persuasive for this audience.
- Patient Engagement: While direct-to-consumer advertising is complex, providing clear, easy-to-understand educational materials for patients through websites and patient advocacy groups can help demystify biosimilars and address any concerns they may have about switching from a brand-name drug they have trusted for years.
Navigating the Payer Landscape and Pricing Strategies
Ultimately, market access for a biosimilar is driven by pricing and reimbursement. The payer landscape in the U.S. is a complex web of public (Medicare, Medicaid) and private entities, each with its own formulary and reimbursement policies.
The pricing strategy for a biosimilar is a delicate balance. The price must be low enough to offer a compelling discount compared to the reference product, incentivizing payers to grant it preferred formulary status. However, the price must also be high enough to recoup the substantial R&D investment and generate a profit.
Typically, biosimilars are launched at a discount of 15% to 35% off the reference product’s list price [12]. However, the net price after rebates and negotiations can be even lower. The key to success is securing favorable formulary placement. If a major payer makes the biosimilar their “preferred” agent, they will use utilization management tools (like prior authorization or step edits) to steer physicians and patients towards the biosimilar and away from the more expensive innovator product. Without this payer leverage, biosimilar uptake can be slow, even with a significant price discount.
The commercial success of a biosimilar is the culmination of a long, integrated strategy. It begins with savvy patent intelligence, is built on a foundation of rigorous science, and is realized through effective communication and a smart market access plan. In this arena, the science and the business are two sides of the same coin.
Future Horizons: What’s Next for Biosimilar Clinical Development?
The field of biosimilar development is anything but static. It is a dynamic and rapidly evolving discipline, constantly being reshaped by scientific innovation, regulatory evolution, and market forces. As we look to the horizon, several key trends are poised to redefine the strategies for designing and executing biosimilar clinical trials. The biosimilar developers who anticipate and adapt to these changes will be the leaders of tomorrow.
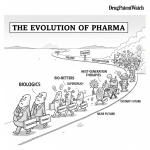
The Rise of Bio-betters and Next-Generation Biosimilars
The first wave of biosimilars focused on creating highly similar copies of existing biologics. The next wave may look quite different. Companies are increasingly exploring the development of “bio-betters.” These are molecules that are based on an existing biologic but have been intentionally modified to improve their properties—for example, by engineering them to have a longer half-life (requiring less frequent dosing), improved stability, or lower immunogenicity.
Bio-betters are not biosimilars; they are considered new molecular entities and require a full de novo development program (like the 351(a) pathway in the U.S.). However, the deep knowledge gained from developing biosimilars—understanding structure-function relationships, advanced analytics, and manufacturing control—provides a powerful springboard for creating these next-generation products.
We will also see the development of biosimilars for increasingly complex products, such as antibody-drug conjugates (ADCs) or even cell and gene therapies in the distant future. These will present entirely new sets of challenges for analytical characterization and clinical trial design, pushing the boundaries of the “totality of the evidence” framework.
Artificial Intelligence and Machine Learning in Trial Design
The integration of Artificial Intelligence (AI) and Machine Learning (ML) is set to revolutionize clinical development, and biosimilar trials are a prime area to benefit. The sheer volume of data generated in a biosimilar program—from high-resolution analytical outputs to genomic data from patients—is staggering. AI/ML can help make sense of this complexity in several ways:
- Predictive Analytics for CQAs: AI algorithms could be trained to analyze the structure of a reference product and predict which quality attributes are most critical to its function, helping to focus the analytical characterization program more efficiently.
- Optimized Trial Design: ML models can analyze historical clinical trial data and real-world data to identify the ideal patient population, the most sensitive endpoints, and the optimal equivalence margins for a confirmatory trial. This could lead to smaller, faster, and more powerful studies.
- Smarter Patient Recruitment: AI can be used to scan millions of electronic health records to identify patients who meet the complex inclusion/exclusion criteria for a trial, dramatically accelerating the recruitment process.
- In Silico Immunogenicity Prediction: Computational models are being developed that can predict the immunogenic potential of a protein sequence. While still in their infancy, these “in silico” tools could one day help to de-risk biosimilar candidates early in development by flagging potential immunogenicity hotspots.
The Evolving Regulatory Landscape and Global Harmonization Efforts
Regulators are not standing still. As they gain more experience with biosimilars, their thinking continues to evolve. We are seeing a clear trend towards placing even greater emphasis on the analytical and PK/PD data, with a corresponding reduction in the expectations for large-scale confirmatory trials, especially for products with a well-understood mechanism of action.
Some experts are even questioning whether a dedicated comparative efficacy trial is always necessary. If a developer can provide an exceptionally strong analytical and functional similarity package, along with equivalent PK data in humans, is a large clinical outcome study truly adding meaningful information, or is it simply an expensive and time-consuming confirmatory step? This debate is ongoing, but the trajectory is towards more streamlined clinical requirements based on the strength of the foundational science.
Furthermore, there is a slow but steady push towards greater global harmonization. Agencies like the FDA, EMA, and PMDA are collaborating more closely, sharing information, and working to align their data requirements. While true global development programs are still challenging, the hope is that in the future, a single, well-designed clinical package will be more readily acceptable across all major markets, reducing the need for duplicative bridging studies and accelerating global patient access.
The future of biosimilar development will be faster, smarter, and more data-driven. It will require a deeper integration of science, technology, and commercial strategy than ever before. The labyrinth is not disappearing, but the tools we have to navigate it are becoming infinitely more powerful.
Conclusion: From Scientific Rigor to Commercial Triumph
The journey of a biosimilar, from a gleam in a strategist’s eye to a staple in the pharmacy, is a modern epic of scientific and commercial ambition. It is a path defined not by the flash of novel discovery, but by the relentless pursuit of similarity—a goal that demands a unique fusion of analytical prowess, clinical precision, and strategic acumen. We have journeyed through the intricate labyrinth of trial design and execution, from decoding the global regulatory tapestry to mastering the high-stakes execution of confirmatory trials, and from harnessing digital tools to navigating the unforgiving terrain of market access.
The core lesson is this: in the world of biosimilars, success is holistic. A triumph in the lab with state-of-the-art analytics is meaningless without a flawlessly executed PK study. A statistically perfect equivalence trial is a hollow victory without a savvy commercial strategy informed by deep patent intelligence. Each phase of development is not a separate silo but an interlocking piece of a single, cohesive argument—the “totality of the evidence.”
The ultimate goal is not merely to create a cheaper copy, but to build a bridge of trust. Trust with regulators, built on a foundation of irrefutable data. Trust with physicians, earned through clear communication and robust clinical evidence. And trust with patients, who rely on the promise that their medicine, whether innovator or biosimilar, is safe and effective.
The challenges are formidable, but the prize is profound. Effective biosimilar development is a key pillar in building a more sustainable and equitable healthcare future. By fostering competition, driving down costs, and expanding access to life-changing biologic medicines, the strategists, scientists, and clinicians who master this complex discipline are not just winning market share—they are advancing a critical mission for global public health. The labyrinth awaits, but for those armed with the right strategies, the path to the center is clear.
Key Takeaways
- Foundation First: The “totality of the evidence” approach means success is built on a massive foundation of state-of-the-art analytical characterization. Investment here de-risks the entire clinical program.
- Regulatory Fluency is Non-Negotiable: Deeply understanding the differing requirements of the FDA, EMA, and other global agencies is crucial for designing a global clinical program that avoids costly delays and duplicative studies.
- The PK/PD Bridge is Critical: Human pharmacokinetic (PK) and, where possible, pharmacodynamic (PD) studies are the essential bridge linking the analytical data to clinical performance. Passing the 80%-125% bioequivalence margin is a key milestone.
- Design Confirmatory Trials for Sensitivity: Confirmatory efficacy trials should be designed as equivalence studies in the most sensitive patient population and with the most sensitive endpoints to efficiently demonstrate no clinically meaningful differences.
- Immunogenicity is a Paramount Concern: A robust, multi-tiered strategy for assessing and comparing immunogenicity is mandatory and central to demonstrating the safety of a biosimilar.
- Operational Excellence is a Competitive Weapon: Flawless execution in patient recruitment, reference product sourcing, and data management is critical for speed-to-market in a competitive landscape.
- Embrace Digital Transformation: Leveraging decentralized trial elements and Real-World Evidence (RWE) can accelerate timelines, improve data quality, and strengthen the value proposition for payers.
- Strategy Begins with Patents: A successful biosimilar program starts with a deep understanding of the reference product’s patent estate, using tools like DrugPatentWatch to identify opportunities and mitigate legal risks.
- Success is Holistic: Clinical, regulatory, and commercial strategies must be integrated from day one. Scientific success must be translated into market access and physician adoption to achieve commercial triumph.
Frequently Asked Questions (FAQ)
1. Why is a large confirmatory efficacy trial sometimes still needed if the analytical and PK data show the products are highly similar?
This is an excellent and central question in biosimilar development. While the goal is to reduce the reliance on large clinical trials, a confirmatory trial serves to address “residual uncertainty.” Regulators may feel that even with strong analytical and PK data, there’s a small but important possibility that minor, unobserved differences could lead to a different clinical outcome. This is particularly true for biologics with complex mechanisms of action or for diseases where the link between PK and clinical effect is not well understood. The confirmatory trial acts as the ultimate safety net, providing direct evidence in patients that these uncertainties do not translate into clinically meaningful differences in efficacy or safety, especially regarding immunogenicity.
2. What is the biggest operational mistake a biosimilar developer can make in their clinical program?
One of the most catastrophic and surprisingly common mistakes is inadequate management of the reference product supply chain. This includes failing to procure enough product for the entire trial upfront, not sourcing from the correct regions (e.g., using only EU-sourced product for a trial intended for FDA submission), or failing to analytically characterize the specific lots used in the trial. A supply chain failure can bring a multi-million dollar trial to a grinding halt. Similarly, failing to prove that the reference product lots you used are representative of the product on the market can undermine the validity of the entire comparison, potentially leading to regulatory rejection.
3. How does the concept of “interchangeability” in the U.S. affect trial design?
Interchangeability requires a higher standard of evidence than biosimilarity. To achieve this commercially valuable designation, a developer must conduct an additional clinical trial—a “switching study.” This study is specifically designed to assess if switching back and forth between the reference product and the biosimilar impacts safety or efficacy. A typical design involves enrolling stable patients on the reference product and then randomizing them to either stay on the reference or undergo multiple switches to the biosimilar. The endpoints focus on PK, immunogenicity, and efficacy to prove that the switched arm is no different from the non-switched arm. This adds significant cost and complexity to the development program but can result in a major competitive advantage in the market.
4. Can Real-World Evidence (RWE) ever replace the need for a randomized controlled trial (RCT) for initial biosimilar approval?
Currently, no. For initial approval, regulators worldwide still require the controlled, head-to-head comparison provided by an RCT to establish biosimilarity. The controlled environment of an RCT is necessary to minimize bias and isolate the effect of the drug itself. However, the role of RWE is rapidly growing. It is becoming essential for post-marketing safety surveillance, for supporting the extrapolation of indications, and for convincing payers of the biosimilar’s value. While it may not replace the pivotal RCT, it is a powerful complementary tool. In the future, for very well-understood products, it’s conceivable that RWE could play an even larger role in a streamlined approval package, but we are not there yet.
5. If my company’s biosimilar has a slightly different glycosylation pattern than the reference product, is the program doomed?
Not necessarily, but it raises the scientific bar significantly. Glycosylation is a Critical Quality Attribute (CQA) that can affect a biologic’s half-life, function, and immunogenicity. If a difference is detected, the burden of proof shifts. The developer must provide a comprehensive scientific justification and robust data to demonstrate that this specific difference has no clinical impact. This would involve: 1) In-depth in vitro functional assays (e.g., Fc receptor binding) to show the difference doesn’t alter the mechanism of action, and 2) A meticulously designed human PK study to prove it doesn’t affect the drug’s exposure. If the PK is shown to be equivalent, and the functional assays are reassuring, regulators may accept the difference. However, it will be under intense scrutiny throughout the review process.
References
[1] IQVIA Institute for Human Data Science. (2022). The Global Use of Medicines 2022: Outlook to 2026.
[2] U.S. Food and Drug Administration. (2009). Biologics Price Competition and Innovation Act of 2009. Public Law 111-148.
[3] Yim, S. (2020). FDA Biosimilars Update. Presentation at the GRx+Biosims Conference.
[4] European Medicines Agency. (2014). Guideline on similar biological medicinal products containing biotechnology-derived proteins as active substance: non-clinical and clinical issues. EMA/CHMP/BMWP/42832/2005 Rev1.
[5] U.S. Food and Drug Administration. (2019). Guidance for Industry: Considerations in Demonstrating Interchangeability With a Reference Product.
[6] European Medicines Agency. (2015). Guideline on similar biological medicinal products. CHMP/437/04 Rev. 1.
[7] International Generic and Pharmaceutical Medicines Association (IGPA). (2021). The Role of Advanced Analytics in Biosimilar Development. Biosimilars Committee White Paper.
[8] International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use. (2009). ICH Harmonised Tripartite Guideline Q8(R2): Pharmaceutical Development.
[9] U.S. Food and Drug Administration. (2022). Draft Guidance for Industry: Studying Multiple Versions of a Reference Product in a Bridging Study.
[10] U.S. Food and Drug Administration. (2015). Guidance for Industry: Scientific Considerations in Demonstrating Biosimilarity to a Reference Product.
[11] Kay, J. (2017). The devil is in the details: non-inferiority and equivalence trials for biosimilars. Annals of the Rheumatic Diseases, 76(11), 1787-1789.
[12] Sarpatwari, A., et al. (2021). Evaluating the impact of biosimilar competition on pricing and use of biologics in the US. Health Affairs, 40(6), 948-956.